
Accurate medical records are crucial for providing the best possible patient care and facilitating client and team communication. Poor medical recordkeeping can result in license discipline or support a legal claim of professional negligence or malpractice. Goals for improving medical recordkeeping skills should include promoting continuity of patient care and ensuring the patient record reflects a high level of professionalism.
Following are the author’s top tips to help improve medical recordkeeping and avoid deficiencies.
1. Understanding & Keeping Up With State & Federal Requirements
State and federal recordkeeping requirements are designed to ensure patient records are standardized, accessible, retrievable, and confidential. States have their own expectations for what should be included, with some requirements being comprehensive and detailed and others more general. For example, records may be required to include the reason for the visit (eg, wellness, illness, urgent care), or physical examinations may need to be performed and documented within 12 hours of anesthesia.
State practice acts typically detail how long patient records should be retained, how information can be shared, who information can be shared with, and how records should be disposed of when the retention period has expired. These requirements also typically include the necessary steps for compliance (eg, recommended time frame to respond to a client request for a record release or to sign a consent form). Additional recordkeeping for certain activities (eg, administering, prescribing, or dispensing extra-label medications, compounded medications, and controlled substances) may be needed.
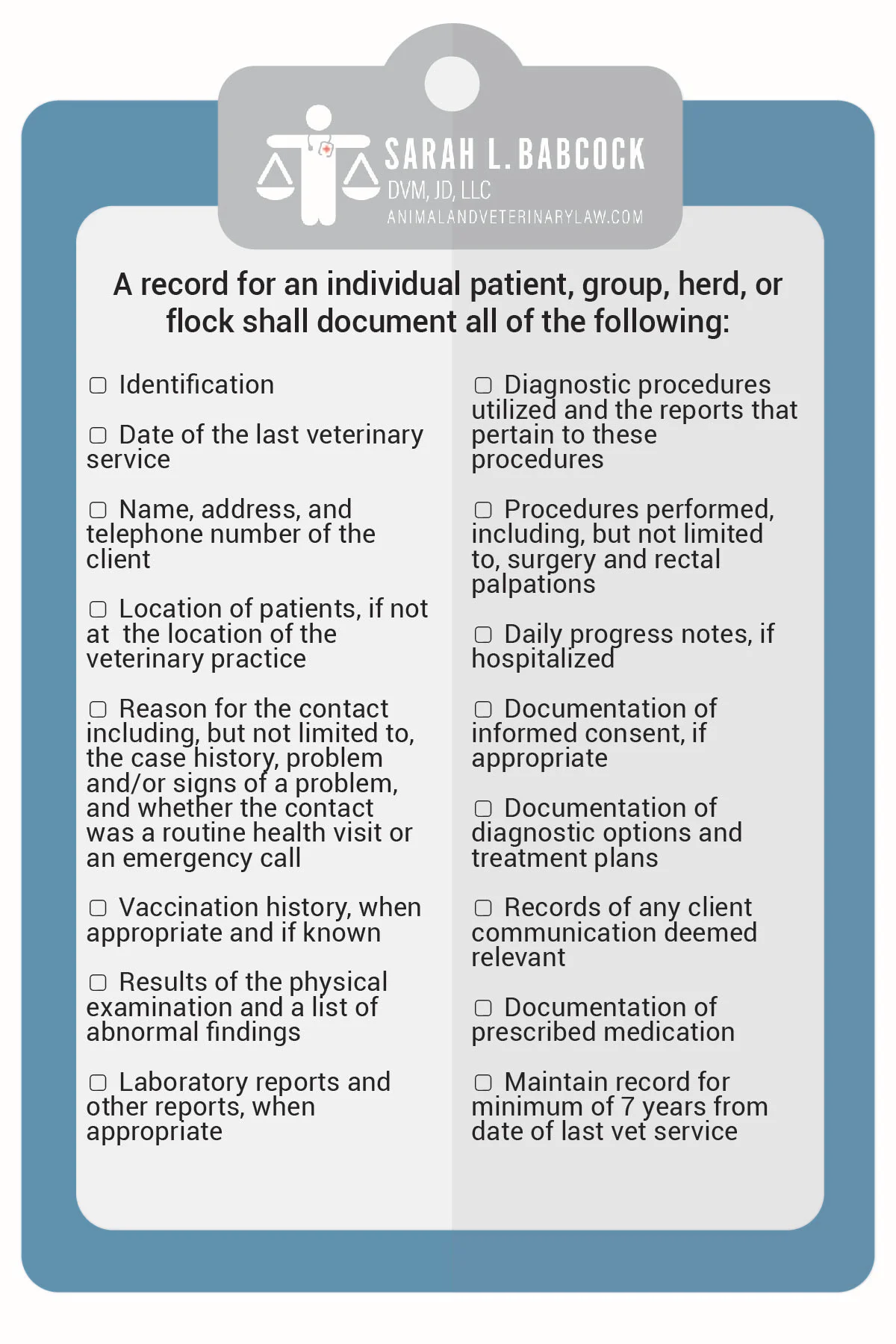
Team members can keep up to date on recordkeeping requirements via local and state organized veterinary medicine groups that offer resources (eg, newsletters, continuing education, notices). Creating a checklist or template that covers state and federal requirements can help with consistent and thorough medical records (Figure 1).
2. Logging Tasks & Creating Protocols
Patient care is often a team effort; however, when multiple team members are involved in a patient’s care or tasks are delegated, medical records should clearly show which team member performed specific actions. In a situation in which one clinician performs the initial examination, a second clinician performs the surgery, and a veterinary technician speaks with the client when the patient is discharged, each role should be clearly documented in the record.
Developing protocols to include both medical and clinic logistics is imperative and should be a collaborative effort. These documents help memorialize specific processes in writing and promote compliance by offering everyone involved the opportunity to be invested in the final product. For example, if a client requests their pet’s records, a protocol should be in place to ensure the clinician completes the record and the clinic requires a release authorization that is documented appropriately.
3. Documenting Client Consent
Client consent is more than a form. Consent includes communication and shared decision-making in addition to paperwork. Following are 3 ways to effectively communicate and document conversations with clients, as well as agreed upon next steps.
When the Client Says Yes
If a client agrees to a procedure, the record should reflect the conversation in detail, including the discussed risks, benefits, costs, possible alternatives, and final decisions. Thought processes leading to diagnosis and decisions, expectations following discharge, and follow-up instructions should be discussed and noted.
When the Client Says No
If the client elects not to follow advice, it is important to be supportive and nonjudgmental but ensure reasonable options are explored to avoid the potential consequences of refusing the recommended plan.1 These conversations should be documented, especially in cases of zoonotic diseases, referrals, and urgent care needs.
If circumstances change, the client should be encouraged to reach out to the clinic. This helps to document the client’s awareness of choices, may allow the client to reconsider without fear of judgment, and highlights the partnership between the client and the clinician.
When the Client Is Not Informed
Clients should be fully aware of all their options, even if cost or other factors may influence decision-making. Following a negative outcome, a client may say, “If I had known about xyz, I would have made a different choice.” Not providing the knowledge to make an informed choice may cause the client to question the care that was provided and/or the validity of their consent.
If a client does not pursue an option because of financial concerns, a cost–benefit analysis should be performed with the client and documented. Although cost is often the primary factor in client decisions, clinicians should not make choices for the client—this includes care practices designed to provide some level of care while working with financial constraints.
The clinic may provide options for a payment plan or referral to a clinic that offers more economical treatment in the area. These options should also be documented.
4. Supporting a Patient Care Plan
Recent updates to the AVMA Principles of Veterinary Medical Ethics highlight the importance of evidence-based medicine,1 which integrates the best research available with clinical expertise and considers the unique needs of each client. If a treatment that lacks scientific support is pursued, clients should be informed and the conversation documented. Similarly, decisions based on atypical facts should be noted in the patient’s record, along with the rationale.
The record should include deviations from standard practice so the plan is easily understood, clearly and concisely demonstrate decisions and next steps, and be brief. Overwhelming the record should be avoided to allow easier interpretation in the future.
5. Committing to Good Documentation
The medical record should reflect the clinician’s professionalism and thought processes. Poor documentation may give the appearance that the care provided was also poor. Incomplete records can contribute to negative outcomes, even if the care provided was satisfactory. Would another clinician be able to pick up the record and provide seamless care based on what is written? If the answer is no, there is room for improvement. A complimentary training covering the top 10 medical recordkeeping mistakes and areas reported in state board license discipline actions as most problematic is available online (see Suggested Reading).