Struvite Crystalluria: Three Cases
The true significance of urine sediment findings from in-house urinalysis needs to be considered in broader context with other key clinical information, such as patient history, examination results, and findings on diagnostic imaging.
The following cases demonstrate the importance of evaluating the total clinical picture and explore how preparing dry-mount urine sediment cytology can maximize the potential of in-house urinalysis. Dry-mount cytology is a quick and relatively easy technique useful not only for evaluating conditions such as urinary tract infection (UTI) or neoplasia but when seeking a pathologist’s second opinion regarding cells found in urine sediment. Cells prepared for dry-mount urine sediment cytology are preserved indefinitely and, therefore, are not subject to degradation during shipment to an outside laboratory.
Related Article: Struvite Urolithiasis
Case 1: Acute Trauma
A previously healthy castrated German shepherd dog (5 years of age) presented after being hit by a car. As part of the diagnostic workup, urinalysis was performed (Table; Figures 1 and 2).
|
What two types of crystals are present?
Based on the urinalysis, which finding is useful for identifying one of the crystals?
What conditions are commonly associated with each type of crystal present?
|

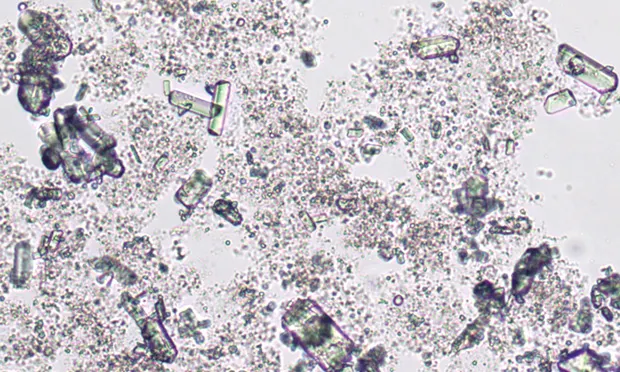
Figure 1. Struvite crystals in urine sediment wet mount from a dog that had sustained vehicular trauma. Two types of crystals are present. One appears as refractile, colorless, variably shaped grit or amorphous debris. The second type of crystal forms 3-dimensional, 6- to 8-sided prisms and rectangles. The amorphous crystals, which are abundant in the background, obscure detailed morphology of many of the 3-dimensional struvite crystals. (unstained wet mount; 10× objective)
Figure 2. Magnification of Figure 1 showing struvite crystals as variably sized, 3-dimensional, 6- to 8-sided prisms surrounded by amorphous phosphate crystals. One erythrocyte is visible (arrowhead). (unstained wet mount; 20× objective, digitally zoomed)

* Values outside reference interval or valueUSG = urine-specific gravity
Related Article:Urine Crystals in Dogs & Cats
Diagnosis:
Incidental Crystalluria
Interpretation & Discussion
Incidental crystalluria from amorphous phosphate and struvite crystals was present in this patient. Based on cytology alone, amorphous crystals could be either phosphate or urate; further urinalysis information is required for specific identification.
Because the crystals are colorless and the patient’s urine is mildly alkaline, these are amorphous phosphate crystals. Amorphous urate crystals are less common, tend to form in acidic urine, and are yellow or yellow–brown. Although amorphous crystals may be seen with various conditions, their presence here is a nonspecific finding and does not typically augment the clinical picture.
Related Article: Nutritional Management of Urolithiasis
Struvite crystalluria may be seen in clinically normal patients, patients with struvite or mixed-content uroliths, or patients with UTI. Struvite crystals can also develop during refrigerated storage of urine samples. In this case, clinical context is essential when determining the significance of the patient’s struvite crystalluria. This dog did not exhibit lower urinary tract signs. Abdominal radiography to detect injuries related to trauma revealed no radiopaque cystic calculi. Leukocytes were not observed in the urine sediment, indicating that lower urinary tract inflammation and, therefore, infection or presence of uroliths were unlikely.
The 1+ heme reaction was secondary to mild hematuria noted in the wet mount and may have been secondary to cystocentesis or blunt trauma. The presence of erythrocytes, hemoglobin, and myoglobin may also contribute to the heme reaction. Given this patient’s history, muscle damage and myoglobinuria could have contributed to the positive heme reaction. Multiple factors likely contributed to the 2+ proteinuria, including urine concentration, the presence of heme protein, and possibly other factors related to recent trauma or occult disease. Also present was 1+ bilirubin, which is a normal finding in concentrated canine urine; this is not a normal finding in some other species.
Struvite crystalluria was incidental and may have been secondary to the highly concentrated urine or possibly refrigerated storage, as handling factors can promote precipitation of crystals in urine.1
|
Amorphous phosphate and struvite (also known as magnesium ammonium phosphate; Figure 2)
Urine pH is helpful when identifying amorphous crystals; amorphous phosphate crystals occur in alkaline urine, whereas amorphous urate crystals occur in acidic urine.
Amorphous phosphate crystals typically have little clinical significance. Struvite crystalluria may be seen in clinically normal patients, patients with struvite or mixed-content uroliths, and patients with UTI. Struvite crystals may also form with refrigerated storage of urine samples.
|
Case 2: Urolithiasis & Prostatitis
A castrated English bulldog (4 years of age) presented for pollakiuria. The dog’s history included urolithiasis, cystotomy, and prescrotal urethrostomy 8 months before presentation. Multiple surgical revisions of the poorly healing urethrostomy had been performed, and the patient was receiving cephalexin. Palpation revealed urinary bladder distention and prostatomegaly. Diagnostic evaluation included urinalysis (Table), imaging, wet-mount cytology (Figures 3–6), and prostatic fine-needle aspiration (FNA).
Cataracts, commonly identified on physical examination, have diverse etiologies and clinical presentations. View this gallery to see various cataracts in cats and dogs.

Figure 3.
Urine sediment wet mount from a dog with pollakiuria. This lowmagnification scan reveals many 3-dimensional, 6- to 8-sided rectangles of variable length and cells that are likely leukocytes based on their relative size. (unstained wet mount; 10× objective)
|
What type of crystal is present?
What abnormalities are present in this urine sediment?
|
Diagnosis
Urolithiasis, Prostatitis, and UTI with Secondary Struvite Crystalluria
Interpretation & Discussion
The urine sediment had increased leukocytes (ie, pyuria) with struvite crystalluria. These findings alone would raise concern about urinary tract inflammation or infection and potential urolithiasis. Given this dog’s urinalysis findings, extensivehistory of lower urinary tract disease and current pollakiuria, bladder distention, and prostatomegaly, imaging was performed and revealed recurrent urolithiasis. Ultrasound-guided FNA showed chronic prostatitis, which was likely associated with chronic lower urinary tract inflammation and infection secondary to repeated surgical manipulation. Prostatitis is generally uncommon in neutered dogs.
To evaluate the effectiveness of current antibiotic therapy and determine other treatment options, culture and sensitivity testing was performed. In addition, because partial urethral obstruction was a concern based on the history and physical examination, a chemistry panel was performed to evaluate for azotemia and electrolyte derangements. Pseudomonas aeruginosa was cultured from the urine sample, and serum chemistry revealed only mild sodium and chloride abnormalities. Antibiotic treatment was modified based on the sensitivity profile, and cystotomy and scrotal urethrostomy were performed.
A low number of leukocytes (Figure 4) can be seen in normal urine; the expected number is influenced by the collection method. Cystocentesis samples should have fewer than 3 leukocytes/40× high-power field, and those collected by catheterization or midstream voiding should have fewer than 8 leukocytes/40× high-power field.
Considerations for pyuria include primary or secondary bacterial infection, urolithiasis, neoplasia, prostatitis, pyometra, or other less common infections. There were multiple causes of this dog’s pyuria: inflammation associated with poorly healed urethrostomy, chronic prostatitis, urolithiasis, and secondary bacterial infection.
The signs and history of chronic lower urinary tract disease along with severe pyuria and lesser hematuria place this case of struvite crystalluria in dramatic contrast with that observed in the patient in case 1. In addition, this case shows variations of struvite crystal morphology. Many of the crystals occurred as 3-dimensional short rectangles or even squares (Figure 5) rather than the more common long rectangles, prisms, or so-called casket covers. X-shaped struvites (Figure 6) were also rarely seen; they are uncommon and typically occur when urine ammonia concentration is high.
The observation of struvite crystalluria may guide initial therapeutic management of urolithiasis; however, full urolith analysis is necessary because many stones are of mixed mineral content, which was of particular concern for this bulldog given the predisposition of bulldogs for urate urolithiasis. In this case, the trace proteinuria may easily be explained by the presence of inflammation.
|
Struvite crystals are present as 3-dimensional, 6- to 8-sided rectangles of variable width.
The sediment is active with pyuria, hematuria, and bacteriuria.
|
Case 3: Pollakiuria & Dysuria
A spayed crossbreed dog (13 years of age) presented for pollakiuria and dysuria of 2 days’ duration. The wet-mount sediment contained many struvites (not shown), leukocytes, erythrocytes, and abundant amorphous debris (Figure 7). It was difficult to confidently identify bacteria in the active sediment.
Figure 7. Urine sediment wet mount from a dog with pollakiuria and dysuria. Numerous leukocytes (arrows) and erythrocytes (arrowheads) are present. Abundant amorphous material in the background hinders the ability to confidently identify bacteria. (unstained wet mount; 50× objective)
Dry-mount urine sediment cytology (Figures 8 and 9) was performed to assist with detection of bacteria and accurate description of their morphology (cocci vs bacilli). Urinalysis via cystocentesis also was evaluated (Table, above).


Figure 8. Urine sediment dry-mount cytology. Many partially degraded leukocytes and bacteria are trapped within purple, lattice-like material. The edge of a struvite crystal is visible (left). (Wright-Giemsa–stained dry mount; 100× objective)
Figure 9. Higher magnification of Figure 8 showing neutrophils (arrow) and bacilli (asterisks) surrounded by nucleoproteins. The border of a struvite crystal (left) is also visible. (Wright-Giemsa–stained dry mount; 100× objective, digitally zoomed)
|
What abnormalities are present in the dry-mount sediment cytology?
What is the lattice-like purple material in the background of the dry mount?
|
Diagnosis
UTI with Bacilli
Interpretation & Discussion
Struvite crystalluria in this patient with lower urinary tract signs was secondary to a bacterial infection. Infection was suggested by urinalysis findings of alkaline urine, proteinuria, pyuria, and hematuria and was supported by urine sediment dry-mount cytology. Urease-producing bacteria (eg, Proteus spp or Staphylococcus spp), produce ammonia that increases urine pH. Alkaline pH and high ammonia concentration favor struvite crystal formation.
The urine sediment wet mount was difficult to interpret because of the density of cells and amount of debris. The presence of pyuria elevated concern that the debris-filled background of the wet mount potentially masked bacteria. Dry-mount cytology was performed to better detect bacteriuria (Figures 8 and 9). This technique has been shown to improve the sensitivity and accuracy of sediment evaluation for the presence of bacterial UTI and can be performed easily in general practice.2-4 In this case, dry-mount cytology clearly revealed the presence of a monomorphic population of bacilli and numerous neutrophils with a background of lysed nuclear material. Although angular crystals could be seen in the dry-mount preparation, they were better identified and quantified in the wet-mount preparation, where fine detail could be appreciated. Urine sediment dry-mount cytology can be useful for identification of microorganisms and cells but not for identification and enumeration of crystals or renal tubular casts.
In addition to better detection and morphologic description of bacteria, dry-mount cytology can aid in identification and preservation of atypical nucleated cells and unusual microorganisms (eg, yeast, fungi). In any fluid sample, cells can degrade after collection and during transport to an outside laboratory; this is particularly the case for urine samples, which are naturally inhospitable to cells. The dry-mount technique helps avoid the challenge of discerning important cytomorphologic details on in-house wet-mount cytology and the frustration of a nondiagnostic result that may be associated with sending a liquid urine sample to an outside laboratory.
Even if a wet mount has already been prepared and stained, the same sample can be converted to dry-mount cytology using the urine sediment that remains in the test tube (see Preparing Urine Sediment Dry Mounts for Cytology, above). Urine sediment wet mounts are prepared by suspending the urine sediment pellet in a volume of urine supernatant that is equal to 10% of the sample volume that was centrifuged to make the sediment. A drop of this sediment suspension is used to prepare the wet mount, and the remaining volume is reserved in the test tube. This preparation will be indefinitely stable and can be either stained and evaluated in-house or sent to an outside laboratory for a pathologist’s opinion. With dry-mount cytology, there is no deterioration during transport.
|
Several degenerate neutrophils with monomorphic bacilli (rods) are in the background and are phagocytosed by the neutrophils. These observations indicate bacterial infection.
The lattice-like purple material in the background is free nuclear material and proteins (ie, nucleoproteinaceous material) from lysed cells.
|
Closing Comments
All three patients presented here had struvite crystalluria, although each had a different clinical presentation. These cases highlight the need to integrate other clinical information with urinalysis data to make optimal decisions about further workup and treatment. The accuracy of urine sediment evaluation can be improved by using dry-mount cytology.
AMY L. WEEDEN, DVM, is a clinical pathology resident at University of Florida. Dr. Weeden completed a shelter animal medicine and surgery internship at Colorado State University and was an associate in private small animal practice for 8 years before returning to University of Florida for specialty training in clinical pathology. Dr. Weeden received her DVM from Louisiana State University.
HEATHER L. WAMSLEY, DVM, PhD, DACVP, is assistant professor at University of Florida. She completed 4 years of specialty clinical training: 1 year as a rotating intern at the Animal Medical Center in New York City and 3 years as a resident at University of Florida, after which she earned certification in clinical pathology. Since 2004, Dr. Wamsley has instructed urinalysis and other clinical pathology wet labs at the NAVC Conference, in addition to participating in a hematology Masterclass and cytology symposium. She received her DVM at University of Wisconsin–Madison before earning a PhD in molecular biology of infectious disease from University of Florida.