Preparing for Safe, Efficient Surgery
Karen Theresa Ellis, LVT, VTS (Surgery), Gulf Coast Veterinary Specialists, Houston, Texas
Veterinary nurses are an integral part of the surgical team, with responsibilities ranging from client communication to operating room and patient preparation. Refer to these guidelines to help ensure that all stages of a procedure are completed safely and efficiently.
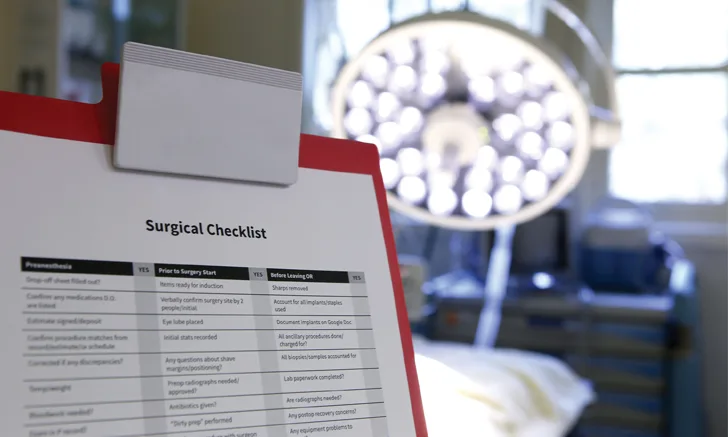
Surgical Checklists
The veterinary nurse should communicate closely with the veterinarian to confirm the procedure being performed, equipment needed, and the anesthetic plan. A surgical checklist can be used as a tool to help ensure that steps are not missed and mistakes are prevented. The World Health Organization (WHO) recommends using a surgical checklist1 divided into 3 stages. (See Surgical Checklist & Table 1.)
At the end of each stage, the veterinary nurse should stop before proceeding further and confirm that previous items have been completed. The checklist helps with memory recall and establishes minimum necessary steps to complete a task.1
When creating a checklist, include items that have been frequently missed or where the consequences of missing the step could be devastating (eg, having no access to blood for a transfusion, failing to discover an item needed for a procedure was unavailable before surgery). The checklist should be short and easy to complete quickly. Print a sample surgical checklist here.
Items for a 3-Stage Checklist
At a minimum, the checklist should include the following:
Preoperative Instructions
When the surgical procedure is first scheduled, review the preoperative instructions with the client to ensure the patient will be fasted according to the veterinarian’s directions and medication will be administered or withheld according to the veterinarian’s preferences.
Hospital Admission
On the day of the surgery, review with the clients the detailed surgical estimate to ensure they understand all the costs, explain the general anesthesia risks, and obtain their signatures on the estimate and the anesthetic release form. The release form explains not only the general anesthesia risks but also the emergency treatment options that can be performed in the event of cardiac arrest. Describe each treatment option clearly and provide the clients adequate time to decide which option is most appropriate for their pet. Ask the clients to confirm the surgery being performed, and use a marker or clipper to identify the surgical location if it is not a standard site. Confirm when the patient last ate and what, if any, medications have been given. If the patient will require other medications during hospitalization, make sure to obtain this information from the clients.
Identify the surgical patient with a neckband that includes at minimum the patient’s name. Based on the hospital, it may be helpful to include items such as breed, sex, color, markings, microchip number, scheduled procedure, or department/ward location in the hospital. Label the patient’s cage or run with an identification card. Always confirm the patient’s identity before performing preanesthetic procedures.
Diagnostic Test Results
Review preoperative diagnostic test results prior to anesthesia induction. Required tests vary based on the patient’s prior medical history and the procedure to be performed. Common tests include a preoperative chemistry profile, CBC, and thoracic radiographs.
Blood tests can help identify potential organ dysfunction, hematologic abnormalities, abnormal platelet counts, and other changes that may affect the anesthetic or surgical plan. Thoracic radiographs allow evaluation of the cardiac silhouette and can help rule out conditions such as metastatic disease, pneumonia, and thoracic trauma.
Additional diagnostics (eg, ECG, coagulation profile, urinalysis, blood pressure measurement) may be indicated in some cases.
Related ArticlesQuiz: Surgical InstrumentsPreoperative Surgical Site PreparationStarting Off Right: Checklists Are Essential for a Good History
Operating Room Preparation
The operating room (OR) and all instrumentation needed should be set up and available prior to induction of anesthesia. The anesthesia machine should be checked for gas levels and tested for leaks. (See Resource.) Intravenous fluids can be set up for use in addition to any warming and monitoring devices. It is helpful to have “pull lists” for the various procedures done at the hospital indicating the instruments or equipment needed for a procedure or particular veterinarian. (See Surgical Pull List.)
Anesthetic Assessment
Review the patient’s record to determine general health and identify specific anesthetic risks. The American Society of Anesthesiologists (ASA) grades a patient’s status on a I to V scale, with level I presenting minimal risk and level V presenting extreme risk.2
Anesthesia Classifications
Use this scale to determine a patient’s status, which will help the veterinary team anticipate potential anesthetic complications.
Patient Preparation
Prior to induction, administer opioid and sedative premedications as prescribed by the surgeon, and place an IV catheter to facilitate induction. Once the patient is under anesthesia, attach the anesthetic monitors and record initial vital signs. Confirm the surgical incision site and the appropriate shave margins for the procedure with the surgeon. Complete all presurgical patient preparation, including bladder expression, preliminary aseptic preparation, and additional radiographs, before entering the OR. Complete the surgical scrub in the OR and position the patient.
Postsurgery
At the end of the surgery, the veterinary nurse should confirm that all procedures have been completed as planned. If any histopathology samples or cultures were taken, they should be labeled and prepared for submission. All sharps should be removed by the veterinarian or surgical assistant and all instruments and sponges accounted for. The surgical team should communicate about any potential postanesthetic/surgical concerns or any treatments needed prior to leaving the OR.
Conclusion
A highly efficient surgical team depends on proper planning, clear team communication, establishing and following surgical protocols, and using checklists during all stages of surgery.3 Each additional minute a patient spends under anesthesia, not just surgical time, can increase a patient’s risk for infection by 0.5%.3 Increasing efficiency can lead to fewer mistakes and shorter anesthetic times, which in turn leads to fewer complications.