Profile
DefinitionChronic bronchitis and asthma are both chronic inflammatory diseases that occur in the lower airways (bronchi and bronchioles). In practice, it is often difficult to distinguish between the two disorders. Chronic bronchitis is defined in part by the presence of a daily cough; asthma is defined in part by acute bronchoconstriction that may resolve spontaneously or with treatment. Bronchoconstriction may or may not cause cough in an individual cat (known as cough-variant asthma). Thus, cats with a daily cough may have either disorder, while cats without cough may have asthma but do not have chronic bronchitis. Both disorders may result in wheeze and exercise intolerance. Finally, human asthma is a syndrome in which the causes may vary greatly, including allergy, exercise, and cold air, in individual patients. For purposes of this discussion, asthma in cats refers to allergic asthma.
GENETIC IMPLICATIONSSeveral "asthma genes" have been implicated in the pathophysiology of human asthma, and this is also an active area of research in veterinary medicine. The Siamese breed seems to be overrepresented, suggesting an inherited trait.
INCIDENCE/PREVALENCEThere are no precise actuarial data. Chronic bronchial disease (both bronchitis and asthma) probably affects 0.75% to 1% of the feline population in general and may affect 5% of the Siamese breed.
GEOGRAPHIC DISTRIBUTIONNone recognized.
SIGNALMENTSiamese and Siamese-related breeds appear to be at risk. Cats of any age may develop chronic bronchial disease, although young and middle-aged cats (1 to 8 years) most commonly have the disorder. Male and female cats appear to be equally at risk.
CAUSESUnknown. The causes of asthma and bronchitis probably differ. The most common causes of asthma in humans include house dust mites, feline "dander," and cockroaches; chronic bronchitis is the result of cigarette smoke in humans, although this association has not been shown in cats.
RISK FACTORSUnknown. In humans with asthma, there is a 50% chance of developing asthma if both parents are asthmatic. Living indoors or outdoors is not causally associated with development of chronic bronchitis or asthma in cats. Cigarette smoke increases symptoms in human patients with established disease; passive cigarette smoke has been linked to bronchial disease in children. No data confirm this phenomenon in cats, although common sense suggests that exposure to cigarette smoke is probably harmful.
PATHOPHYSIOLOGYUnknown. In humans, cigarette smoke causes cough, airway wall thickening, and hypertrophy of the mucus-secreting apparatus. Asthma is more complex and is better thought of as a "syndrome" with many causes. The most common form, "allergic asthma," results from a complex interplay of activated T lymphocytes, antigen, antigen-processing cells, various cytokine proteins and chemical messengers, and activated eosinophils and other inflammatory cells in the bronchial mucosa. The inflammatory results of these processes include excessive mucus secretion, airway wall edema, and, in asthmatic patients, bronchoconstriction. Airway muscle hypertrophy and hyperplasia are more common in asthmatic than in bronchitic airways. Basement membrane thickening is a feature of asthma in humans but has not consistently been found in cats.
SIGNSCough, mucus production, wheeze, open-mouth breathing, and exercise intolerance directly resulting from the pathophysiologic derangements described above.
HISTORYCough and increased respiratory rate and effort are common to asthma and chronic bronchitis. There is usually a gag/choke or swallow at the end of the cough, signifying excess mucus production. Asthmatic patients may have symptom-free periods, whereas a daily cough is the defining feature of bronchitis.
Diagnosis
PHYSICAL EXAMINATIONPhysical examination may be unremarkable. Most cats with chronic bronchitis or asthma have increased bronchovesicular lung sounds heard diffusely. Wheeze may be heard, especially during expiration.
Respiratory rate may be increased, and there may be nasal flaring. Cyanosis occurs in severe cases.
DIAGNOSIS/DIFFERENTIAL DIAGNOSISThere are no clinical signs or laboratory tests available in general practice that are pathognomonic for asthma or bronchitis. We pursue diagnostic testing in cats with cough, tachypnea, and/or wheeze to determine the presence of other common causes of these signs-for example, heart failure, pneumonia, pulmonary cancer, respiratory parasitism, and inhaled foreign bodies.
LABORATORY FINDINGS/IMAGINGAsthmatic cats often present with a history of sudden onset of labored breathing that is quickly relieved with some combination of oxygen, bronchodilators, and steroids. In some cases, the only sign is chronic or intermittent cough. Patients with chronic bronchitis have a history of chronic daily cough with gag/choke or swallow at the completion of the cough, representing excessive mucus secretion.
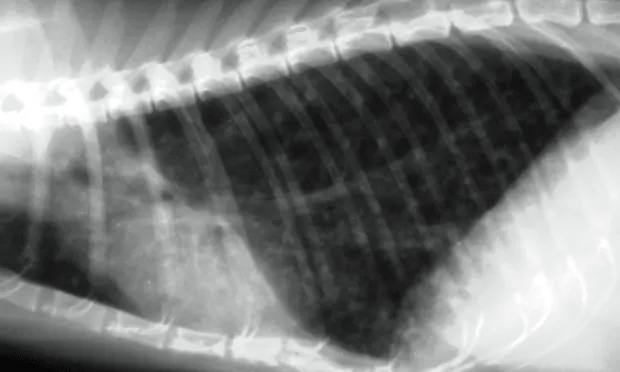
The most common radiographic change common to both feline asthma and bronchitis is peribronchial cuffing, often described as doughnuts or tram lines (Figure 1). Other common causes of cough and increased respiratory effort include pneumonia, heart failure, cancer, and heartworm disease. These disorders usually create radiographic abnormalities that differ from the classic findings of hyperinflation and bronchial markings seen in chronic bronchitis or asthma.

Figure 1. This lateral thoracic radiograph demonstrates classic features of feline asthma, including hyperinflation and peribronchial infiltration (doughnuts and tram lines).
Both bronchitic and asthmatic cats have excessive airway mucus. Nonseptic neutrophils are the predominant cell type in bronchial fluid. Eosinophils may predominate in bronchial fluid from asthmatic cats, although healthy cats also frequently harbor large numbers of eosinophils in the respiratory tract.
We also measure pulse oximetry in cats breathing room air to determine the relative degree of impaired oxygen exchange. In general, a pulse oximeter reading of 95% or above (PaO2 of approximately 80 mm Hg or above) is considered stable; a reading of 90% or below (PaO2 of approximately 60 mm Hg or below) is considered extremely unstable.
Bronchoscopy is usually not necessary for diagnosis. Pulmonary function testing is used to determine airway hyperresponsiveness in asthmatic persons. This technology is now available to approximate airway reactivity in awake, nonrestrained cats (Buxco box, Buxco Electronics; Wilmington, NC).
Skin testing for the presence of antigen-specific IgE has been proposed as a way to determine an underlying "cause" of allergic asthma. However, the biological response of mast cells in skin often differs from that of mast cells in the airways to the same antigen in the same cat. For this reason, the author does not yet recommend this manner of testing.
POSTMORTEM FINDINGS
Bronchitic and asthmatic airway epithelium may thicken (hypertrophy), evolve to a different structure (metaplasia), or simply become damaged (erosion or ulceration).
Bronchitic and asthmatic goblet cells and submucosal glands may enlarge and produce excessive amounts of a particularly thick form of mucus.
Asthmatic bronchial smooth muscle will often spasm and may undergo hypertrophy and/or hyperplasia.

These changes are associated with cellular infiltration of the bronchial mucosa and submucosa. This tissue may also become edematous. See Figures 2 and 3.
F__igure 2. A cross section from the large airway of a cat with asthma, demonstrating the classic findings of smooth muscle hypertrophy,

invagination of epithelium (bronchoconstriction), and luminal exudate.
Figure 3. This large airway from a cat with chronic bronchitis demonstrates goblet cell hypertrophy and a mucus plug. Airway smooth muscle is normal and there is no evidence of bronchoconstriction, thus distinguishing bronchitis from asthma.
Treatment
INPATIENT OR OUTPATIENTAsthmatic and bronchitic patients may present in various stages of distress. The decision to hospitalize these patients is made on a case-by-case basis. In addition to clinical criteria, patients with a pulse oximeter reading of 95% or higher are often treated as outpatients; those with readings of 90% or below are frequently hospitalized and treated with oxygen. Between the 90% and 95% values, there is great room for individual clinician decision making.
ACTIVITYCats with bronchitis or asthma usually adjust activity to suit their level of comfort.
CLIENT EDUCATIONBoth chronic bronchitis and asthma are chronic disorders that require chronic treatment. Some patients with asthma outgrow the disease, and others seldom have clinical signs. Some cats with asthma get worse, some get better, and others remain stable for years. Cats with chronic bronchitis tend to slowly deteriorate and become less stable as time passes. These patients rarely if ever "grow out" of the disease.
If inhalants are used, clients must be shown how to use them with their own cat and demonstrate to the clinician to confirm that they can use the medications correctly. Thus, the MDI is used with a "spacer" and facemask that is specifically designed for cats. The spacer is a plastic chamber the size of the cardboard tube in a roll of toilet paper. The MDI fits into one end of the spacer; the other end attaches to the facemask.
The client places the facemask gently over the cat's nose. The MDI is actuated (pressed), and the medication fills the spacer. The cat breathes in and out 7 to 10 times with the mask in place, and treatment is complete.
MEDICATIONSTo some extent, drug therapy depends on whether clinical signs occur daily. Because chronic bronchitis is defined in part by the presence of a daily cough, we treat bronchitic cats with a twice-daily corticosteroid. Asthmatic cats are slightly more complex. Cats that have clinical signs more than twice weekly are treated with daily corticosteroids; those that have clinical signs less than twice weekly are usually treated with just bronchodilators on an as-needed basis. This approach is based on the National Institute of Health's recommendation for humans with asthma and has served as the basis for treatment of more than 125 cats with bronchial disease in the author's practice over the past 6 years.
CorticosteroidsPrednisone can be given at 1 mg/kg Q 12 H for 5 days. The response is usually dramatic. The drug is then tapered to the lowest effective dose. If daily prednisone is required to control clinical signs, the author introduces Flovent (GlaxoSmithKline) (inhaled fluticasone, 110 µg Q 12 H), given as a single "puff" into a feline-specific chamber (Aerokat, Trudell Medical International). The patient then takes 7 to 10 breaths. Prednisone is gradually tapered over a 2-week period to allow the inhaled medication to achieve its full effect.
BronchodilatorsAlbuterol is given by inhalation as needed in the same manner as steroids. Albuterol can be given every one-half hour for 4 to 6 hours if needed in a crisis. Oral drugs can be used for cats that cannot tolerate inhaled albuterol. The pharmacokinetics of theophylline are well described in the feline species; however, in the author's experience, the response to terbutaline (0.1 mg/kg PO Q 12 H) is more consistent. Cats in status asthmaticus can also be treated with parenteral terbutaline (0.01 mg/kg IV or IM).
OxygenOxygen is usually given in an oxygen-enriched cage. The author uses the patient's clinical status and pulse oximeter reading to determine the need for oxygen (pulse oximeter reading > 95% approximates a PaO2 of 80 mm Hg and does not usually require oxygen therapy).
AntibioticsThere is no objective evidence that bacterial infection plays a significant role in the cause or continuation of most cases of feline asthma or chronic bronchitis. In general, antibiotics are rarely indicated for cats with asthma or chronic bronchitis and are appropriate only when there is good evidence of true airway infection.
Antileukotriene (or Receptor) InhibitorsThese drugs block production or ligation of leukotrienes (LTs) to their receptors. The product of LTC4 and LTD4 metabolism, LTE4, is a useful marker for the production of these molecules in humans with asthma. Recent data suggest that LTE4 in urine, and thus LTC4 and LTD<sub4sub> in the bloodstream and airways, is not increased in cats with experimentally induced allergic airway disease or naturally occurring bronchitis. In addition, direct instillation of LTC4 into the airways of normal cats has no adverse effect on feline airway structure or function. No current data support the use of antileukotriene drugs to treat cats with asthma or chronic bronchitis.
CONTRAINDICATIONS & INTERACTIONSIf bronchodilator drugs that increase beta-adrenergic tone increase myocardial contractility, cats with hypertrophic cardiomyopathy may theoretically have a worsening of their outflow tract obstruction. However, in practice this occurrence is rare.
Because inhaled steroids are not absorbed into systemic circulation, they do not interact significantly with other drugs. As a result, they are rarely contraindicated by other treatments or comorbid diseases.
PRECAUTIONSAsthma can be acute and life-threatening. Bronchitic or asthmatic patients should be seen immediately if clinical signs worsen.
ALTERNATIVE & NOVEL THERAPIESNo alternative therapies reliably benefit cats with asthma or chronic bronchitis. Experimentally, cyproheptadine was shown to block allergen-induced airway smooth-muscle contraction in feline tissue baths and cyclosporine was used to inhibit the development of airway reactivity. However, neither drug has lived up to its promise in a clinical setting.
NUTRITIONNo dietary changes reliably benefit cats with asthma or chronic bronchitis. Grossly obese patients will benefit from weight reduction so that the diaphragm can fully expand during inhalation.
Follow-up
PATIENT MONITORINGPatients with newly diagnosed chronic bronchitis or asthma should be rechecked within 7 to 10 days to ensure that medications are being dispensed properly.
PREVENTIONThere are no recognized common triggers of asthma or chronic bronchitis in cats. Anything that can be inhaled can theoretically trigger an asthmatic or bronchitic cough.
COMPLICATIONS/COURSEIn some cats (15% to 25%), the right middle lung lobe collapses. Although this may cause no additional clinical signs, it can be an additional cause of chronic cough. The collapsed lung lobe reexpands in fewer than 50% of cases.
Untreated asthma can be rapidly fatal. Untreated chronic bronchitis often gets worse and may result in chronic debilitation.
AT-HOME TREATMENTAerosolized particles and dry, unhumidified air may contribute to clinical signs. Humidification of room air to at least 40% is recommended. Air purifiers are probably only helpful if they are effective for the size of the room (or the house) where the cat spends most of its time. Common sense dictates that cats with bronchial disease should not be exposed to dust, molds, cigarette smoke, fireplace exhaust, construction debris, carpet sweepings, and other particulate matter.
FUTURE FOLLOW-UPStable cats should be reevaluated every 3 to 6 months. Unstable patients should be evaluated as often as needed until they become stable.
In General
RELATIVE COST$-$$ Initial evaluation and diagnosis$-$ Initial treatment$ Monthly medication
PROGNOSISAsthma and chronic bronchitis are not curable. Spontaneous resolution is common in adult humans who developed asthma in childhood. This may or may not be true in asthmatic cats. Some cats with asthma or bronchitis may be only mildly symptomatic, and others may have life-threatening illness. Education is critical so that our clients develop realistic expectations of the effectiveness of drug therapy for their pets.
TX at a glance
• Asthmatic patients with a pulse oximeter reading of 95% or higher are often treated as outpatients; those with readings of 90% or below are frequently hospitalized and treated with oxygen.• Bronchitic cats are treated with a twice-daily corticosteroid.• Asthmatic cats that have clinical signs more than twice weekly are treated with daily corticosteroids; those that have clinical signs less than twice weekly are usually treated with just bronchodilators on an as-needed basis.• Prednisone and albuterol can be administered by inhalation with use of a spacer and facemask in asthmatic cats; the response to prednisone is often dramatic.