Interpretation of Serum Alkaline Phosphatase in Dogs
Cynthia R. L. Webster, DVM, DACVIM, Cummings School of Veterinary Medicine at Tufts University

Profile
Definition
An increase in serum ALP activity is a common, nonspecific finding in dogs that is associated with drug induction (corticosteroids, anticonvulsants), extrahepatic diseases (pancreatitis, endocrinopathies), or primary liver pathology (including nodular hyperplasia in older dogs).
Problems
What is the clinical significance of an increase in total ALP? Is the increase in serum total ALP associated with hepatobiliary disease or primary bone disorders or due to drug induction from corticosteroids or phenobarbital? Are increases due to corticosteroid or phenobarbital resulting from enzyme induction or drug-induced hepatotoxicity?
When increases in total ALP are due to hepatobiliary disease, are they associated with primary hepatobiliary disease, or do they represent secondary involvement of the liver? Conditions in which total ALP may be elevated without the presence of clinically significant hepatobiliary disease are listed in the Box.
Box: Conditions Other Than Primary Liver Disease Associated with Increased Serum Total ALP Activity
Bone disorders
Young animals (normal physiologic-related finding)
Osteosarcoma
Osteomyelitis
Endocrinopathies
Diabetes mellitus
Hypothyroidism
Hyperadrenocorticism
Gastrointestinal disease
Pancreatitis
Inflammatory bowel disease
Hypoxia/Hypotension
Congestive heart failure
Hypotensive crisis
Severe hemolytic anemia
Status epilepticus
Neoplasia
Hepatic metastasis
Paraneoplastic induction
Drug induction
Corticosteroids
Phenobarbital
Systemic infections
Incidence/Prevalence
Unknown, but increased total ALP is one of the most common abnormalities detected on biochemical profiles in dogs.1
Signalment
Young dogs have increases in bone isoenzymes due to increased osteoblastic activity in growing bones.
Breed-specific hepatopathies in Labrador retrievers, Doberman pinschers, Dalmatians, cocker spaniels, Bedlington terriers, and Skye terriers should alert the clinician to the possibility of a primary hepatobiliary disorder.
Nodular hepatic hyperplasia is a common, age-related, incidental lesion in dogs with a reported incidence from 70% to 100% in dogs older than 14 years of age.
Cause/Risk Factors/Pathophysiology
The primary clinical asset of serum total ALP determination is its sensitivity (80%) for hepatobiliary disease.2 (Sensitivity is the ability of the test to detect animals that have hepatobiliary disease.) The major limitation in interpreting serum total ALP is its low specificity (51%) for hepatobiliary disease. (Specificity is the ability of the test to exclude the presence of hepatobiliary disease.) The low specificity of serum total ALP is due to presence of several ALP isoenzymes (bone, liver, corticosteroid-induced) and the unique susceptibility of the enzyme to induction by drugs.
Bone ALP accounts for about one third of normal serum total ALP and is elevated with conditions associated with increased osteoblastic activity, such as bone growth in young dogs, or with pathologic conditions, such as osteomyelitis, osteosarcoma, or renal secondary hyperparathyroidism.3 Typically, bone ALP elevations in these conditions are mild to moderate (three to five times the upper limit of normal).
Liver ALP is a membrane-bound enzyme present on biliary epithelial cells and hepatocytes. Increases in serum liver ALP are due to elution of the enzyme from the membrane following hepatobiliary damage. The largest increases are seen with focal or diffuse intrahepatic or extrahepatic cholestasis. Mild to moderate increases are seen with chronic hepatitis and hepatic necrosis.
Corticosteroid-induced ALP is produced by the liver and is found on hepatocyte membranes.4-6 This enzyme increases from de novo synthesis of the enzyme in dogs exposed to endogenous or exogenous corticosteroid excess.
Diagnosis
Clinical findings can be used as an aid in identifying the source of total ALP elevation. Similarly, diagnostic imaging can be helpful in determining the root of the problem, as can laboratory analysis and biopsy. The following indicators areimportant.
History/Physical Examination
History of drug administration: Particularly corticosteroids (oral, parenteral, or topical) or phenobarbital, but also other potentially hepatotoxic drugs, such as potentiated sulfonamides and nonsteroidal antiinflammatory agents
Bone pain: Osteomyelitis, osteosarcoma
Polyuria/polydipsia: Hyperadrenocorticism, diabetes mellitus, chronic liver disease, congenital portosystemic shunts
Dermatologic disorders: Hyperadrenocorticism, hepatocutaneous syndrome
Diffuse cerebral signs: Hepatic encephalopathy from chronic liver disease or congenital portosystemic shunts
Pot belly: Abdominal wall muscle atrophy with centripetal redistribution of fat in hyperadrenocorticism
Jaundice: Prehepatic (hemolytic anemia), hepatic, or posthepatic hyperbilirubinemia
Abdominal effusion: Chronic liver disease, neoplasia, pancreatitis, congestive heart failure• Hepatomegaly: Primary liver disease, steroid hepatopathy, passive congestion, hepatic lipidosis
Dyspnea/increased lung sounds: Congestive heart failure
Abdominal pain: Pancreatitis, cholecystitis, gastric ulceration
Chronic intermittent gastrointestinal signs: Gastric ulceration secondary to chronic liver disease, congenital portosystemic shunts, chronic pancreatitis, inflammatory bowel disease
Imaging
Radiography
Hepatomegaly: Steroid hepatopathy, congestive heart failure, hepatic lipidosis, and focal and diffuse hepatobiliary disease
Microhepatica: Chronic end-stage hepatobiliary disease, congenital portosystemic shunts
Choleliths: 50% are visible radiographically and may be associated with secondary cholecystitis.
Decreased abdominal detail: Ascites
Cardiomegaly and signs of pulmonary edema: Congestive heart failure
Lytic bone lesion: Bone tumor or infection
Ultrasonography
Focal or multifocal hepatic lesions: Hepatobiliary neoplasia, nodular hyperplasia, metastatic disease, abscess
Diffusely hyperechoic liver: Steroid hepatopathy, hepatic lipidosis, lymphosarcoma
Diffusely hypoechoic liver: Passive congestion, lymphosarcoma, suppurative hepatitis
Normal liver: Does not rule out primary hepatic disease
Gallbladder/biliary tree: Gallbladder mucocele, distention of intra- and/or extrahepatic biliary tree, bile duct mineralization, choleliths
Portal vasculature: Single or multiple acquired portosystemic shunts, portal vein thrombosis, passive congestion
Pancreas: Enlarged hypoechoic, surrounded by hyperechoic fat with pancreatitis
Thickened gastrointestinal wall with retention of normal layering: Inflammatory bowel disease
Hepatic metastasis: Primary neoplasia of spleen, stomach, pancreas, intestine, or adrenals
Laboratory Analysis
Hyperadrenocorticism: Mild polycythemia, mild thrombocytosis, mild to moderate increase in ALT and GGT, hypercholesterolemia
Primary liver disease: Concurrent increases in serum ALT, AST, and GGT; hypoalbuminemia; low blood urea nitrogen; hypocholesterolemia; hypoglycemia. Note: The specificity of the total ALP for hepatobiliary disease can be improved to 94% if used in combination with serum GGT.
Chronic liver disease: Pure transudate or modified transudate as evidenced by abdominal tap
Acute pancreatitis: Acute nonseptic neutrophilic inflammation as evidenced by abdominal tap; increase in serum amylase and/or lipase
Diabetes mellitus: Persistent hyperglycemia
Malignancy: Malignant effusion as evidenced by abdominal tap. High protein fluid with exfoliated neoplastic cells (pancreatic, intestinal, adrenal adenocarcinoma, or lymphoma). Absence of neoplastic cells, however, does not rule out cancer. Hemorrhagic effusion with ruptured hemangiosarcoma.
Definitive Diagnosis
Disease-specific
Hyperadrenocorticism: Failure to suppress on an LDDS test. Exaggerated response to an ACTH-stimulation test.
Hepatobiliary disease: Abnormal hepatic function test: Elevated total serum bile acids. Hyperbilirubinemia with a normal PCV is due to hepatic or posthepatic disease. Blood hyperammonemia confirms the presence of hepatic enceph-alopathy. Increased prothrombin time or partial thromboplastin time can accompany severe hepatobiliary disease.
Nodular hyperplasia: Asymptomatic patient, typically older than 8 years of age with mild to moderate increase in total ALP. Other serum liver enzymes and hepatic function tests are normal. Ultrasonography shows multifocal nodules. Hepatic biopsy shows well-circumscribed nodules with normal but often vacuolated hepatocytes surrounded by normal hepatic tissue. Wedge biopsy works best, since nodular hyperplasia must be differentiated from regenerative nodule in a cirrhotic liver, which requires the finding of fibrosis and/or inflammatory changes in surrounding hepatic parenchyma.
Laboratory testing
ALP isoenzyme analysis: Determination of corticosteroid-induced increases in ALP by levamisole inhibition is a sensitive (95%) but not specific (18%) indicator of excess exposure to corticosteroids.7 Many dogs with primary hepatobiliary disease have increases in both corticosteroid-induced ALP and liver ALP.8,9 Corticosteroids induce increases in both liver and bone ALP along with corticosteroid-induced ALP. Phenobarbital increases liver ALP.
Hepatic biopsy: Identify primary hepatic disease, such as lipidosis, neoplasia, vascular, or inflammatory/fibrotic disease. Steroid hepatopathy is characterized by the presence of vacuoles in hepatocytes, which most studies suggest are filled with glycogen5 (Figure 1). May be associated with endogenous or exogenous administration of corticosteroids or with endogenous excess of other adrenal steroids, such as 17-hydroprogesterone.10
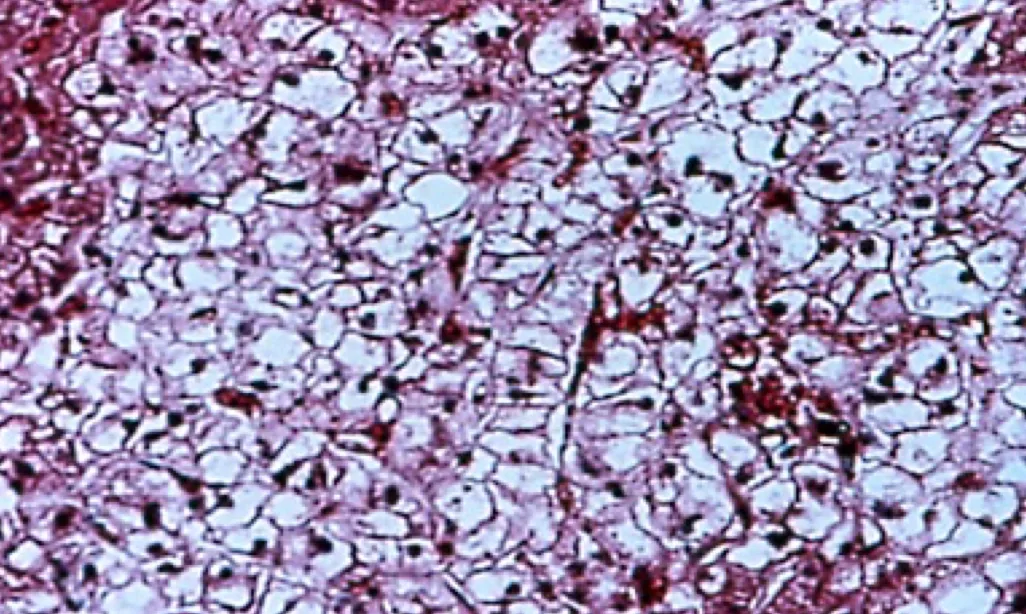
Steroid hepatopathy in a dog on immune-suppressive doses of prednisone
Treatment
Treatment is tailored to the specific disorder. Asymptomatic patients with an increase in serum total ALP or patients with primary hepatic disease on corticosteroids or phenobarbital are particularly problematic. Management of such patients is reviewed in the following discussion.
Patient Monitoring
Asymptomatic patients
Look for signs of occult hyperadrenocorticism. Perform an LDDS or ACTH-stimulation test. Measure cortisol levels initially with ACTH stimulation; if indicated, pursue testing for other adrenal steroids, such as 17-hydroxyprogesterone. If there are no signs of other disease but total ALP is less than 2 times upper limit of normal, monitor total ALP monthly. If total ALP is persistently elevated or more than 4 times upper limit of normal, perform abdominal ultrasonography and evaluate as follows:
Focal or diffuse liver disease: Hepatic biopsy
Bile duct obstruction in the absence of pancreatic disease: Surgical decompression of biliary tract
Gallbladder mucocele: Cholecystectomy
Choleliths (without obstruction) and/or thickened gallbladder wall: Perform cholecystocentesis with bacterial culture and bile sensitivity testing, or give a therapeutic trial of antibiotics and choleretics (ursodeoxycholate).
Dogs on corticosteroids
Typical findings include hepatomegaly, diffusely hyperechoic hepatic parenchyma on ultrasonography, steroid hepatopathy on hepatic biopsy, moderate to marked increases in total ALP (3 to 64 times upper limit of normal), mild to moderate increases in ALT and GGT (2 to 6 times upper limit of normal) with little to no increase in AST (< 2-fold increase).
Signs of possible hepatotoxicity include abnormalities of hepatic function tests, such as increased total serum bile acids, hyperbilirubinemia, hypoalbuminemia, coagulopathy, ascites, or hepatic encephalopathy. Hepatic biopsy shows vacuolar hepatopathy with areas of focal necrosis, cholestasis, and degeneration of hepatocytes.
Treatment involves discontinuing corticosteroids and substituting an alternative immunosuppressive, antiinflammatory agent, such as azathioprine or chlorambucil.
Dogs on phenobarbital
The liver of a dog with cirrhosis due to chronic hepatotoxicity from phenobarbital is shown in Figure 2. Typical findings include increased total ALP usually less than 5 times upper limit of normal, with ALT usually less than 2 times upper limit of normal. GGT, AST, total serum bile acids should be within the normal range.11,12 Ultrasonography yields normal findings, and most dogs do not have hepatomegaly. Biopsy shows diffuse cytoplasmic granularity due to proliferation of smooth endoplasmic reticulum.

Cirrhotic liver in a dog secondary to chronic hepatotoxicity from phenobarbital
Signs of possible hepatotoxicity include abnormal hepatic function tests. ALT, GGT or AST elevations more than 2 times the upper limit of normal. Hepatic biopsy shows chronic inflammatory/fibrotic disease.13 Treatment involves weaning from phenobarbital and onto alternative antiseizure medications, such as potassium bromide; controlling the complications of hepatic failure; and initiating hepatoprotective therapy with ursodeoxycholate and/or S-adenosylmethionine.
Follow-up
Prognostic Significance of ALP
Increases in serum total ALP with primary hepatobiliary disease are indicative of active hepatobiliary disease. The increase is usually-but not always-proportional to the severity of ongoing damage. In end-stage fibrotic liver disease, however, total ALP may not be elevated in proportion to the degree of hepatic disease because of enzyme depletion secondary to replacement of normal hepatocytes by fibrosis.
Since the liver has large regenerative capacity and great functional reserve, the magnitude of elevation of total ALP is not indicative of the degree of functional impairment and is not prognostic. However, the prognostic significance of total ALP can be improved by sequential evaluation, especially in conjunction with hepatic biopsy or function tests. Since the half-life of ALP in dogs is 72 hours, a 50% decrease in total ALP over a 3- to 4-day period may indicate resolution of acute injury. In the absence of hepatotoxicity, serum total ALP elevations due to phenobarbital should return to normal in 2 to 4 weeks after discontinuation of the drug. Increases in total ALP due to corticosteroid excess, however, may take several months to normalize.
Elevations in bone ALP are associated with shorter survival time in appendicular osteosarcoma.14
DX at a glance
Serum Total ALP
Hepatobiliary, bone, and corticosteroid-induced isoenzymes contribute to total serum alkaline phosphatase levels in dogs.
Elevation in the bone isoenzyme is associated with increased osteoblastic activity; in osteosarcoma, the degree of bone ALP elevation predicts survival time.
Definitive diagnosis of induction of the corticosteroid isoenzyme is made by medication history along with the presence of clinical or laboratory signs suggestive of hyperadrenocorticism in combination with abnormal LDDS or ACTH stimulation.
Total ALP is a sensitive but relatively nonspecific indicator of hepatobiliary disease. Specificity for primary hepatobiliary disease is increased when it is used in series with other liver enzymes.