Which Drugs Are Used to Treat Feline Asthma?
Glenn A. Olah, DVM, PhD, DABVP (Feline), Winn Feline Foundation, Albuquerque Cat Clinic, Albuquerque, New Mexico
Profile
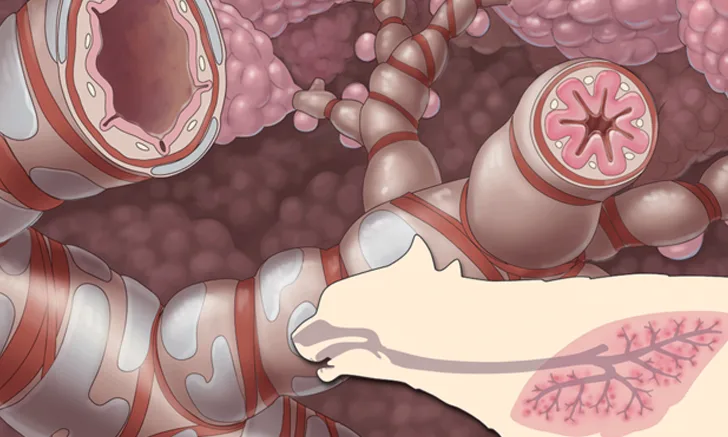
Feline asthma is an allergic airway inflammatory disease triggered by aero-allergens, resulting in type 1 (IgE-mediated) hypersensitivity reaction and dominated by type 2 T-helper cells.1,2 It affects about 1%–5% of the feline population, with a median age of 4–5 years; Siamese and Havana brown cats are overrepresented.2,3
Hallmark features → Naturally occurring asthma
Eosinophilic airway inflammation
Mucus hypersecretion
Bronchoconstriction
Hyperresponsiveness (in response to both allergenic and nonallergenic stimuli)
Airway remodeling2,4,5
Inflammation in airways → Can lead to irreversible airway-remodeling damage2,4
Controlling inflammation is, therefore, the primary goal of therapy.
Despite similarities between human and feline asthma, much about the inflammatory processes that occur in feline asthma remains to be ascertained.6
Primary treatment options → Primary therapeutic approaches include
Glucocorticoid (steroidal) therapy: systemic and inhalant
Bronchodilator (asthmatic crisis) therapy
Supplemental/concomitant therapy
Glucocorticoid (Corticosteroid) Therapy
Glucocorticoids, although nonspecific in their actions, are the mainstays of treatment for feline asthma. Glucocorticoids have potent antiinflammatory effects and are used to suppress airway inflammation and thus slow down or minimize irreversible airway-remodeling damage. Detailed explanation of the pharmacology, mechanisms of action, and resistance of glucocorticoids in the inflammatory process are beyond the scope of this article but can be found in the literature.7,8
General note → Two distinct protocols: systemic (oral, injectable) and aerosol inhalant (metered dose inhaler [MDI])
If the patient does not have good response to oral corticosteroids, it may be unlikely that response to inhaled corticosteroids would be better.
Avoid glucocorticoid therapy if possible → In cats with concurrent diabetes mellitus, heart disease, or chronic FHV-1 infection
Other contradictions: pancreatitis, GI ulceration (except ulcers secondary to IBD), concurrent administration of NSAIDs9-12
Individual cats can vary greatly in their response to the therapeutic and adverse effects of glucocorticoids.
There may be qualitative differences between the effects of different glucocorticoids in the same cat.13
Systemic Glucocorticoids
Cats generally tolerate systemic glucocorticoids well and tend to develop fewer adverse effects than do dogs. Nevertheless, long-term, high-dose therapy can lead to cushingoid effects.
Other adverse effects include PU/PD, polyphagia, alopecia, skin atrophy, poor wound healing, bruising, increased susceptibility to infections, weight gain with or without concurrent muscle mass loss, and obesity.6
Caution: Steroid-induced diabetes mellitus may occur, and cats with underlying heart disease may develop heart failure9 (see also Inhalant Glucocorticoids6).
PREDNISOLONE & PREDNISONE
Formulation → Oral, parenteral
Dose → Oral prednisolone/prednisone: 1–2 mg/kg PO q24h or 0.5–1 mg/kg PO q12h for 10–14 days, then taper over next 2–3 months until <0.5 mg/kg q48h (if possible) or taper to lowest effective dose3,6,14-17
Emergency dose → Injectable prednisolone sodium succinate: 15–30 mg/kg IV; repeat q4–6h as needed.18
Key Points
Cats do not convert prednisone (a prodrug) to prednisolone (the active compound) very efficiently, although the reason (enzyme, process) remains unknown; therefore, oral prednisolone is preferred over oral prednisone in cats when possible.
If oral prednisone must be used, consider increasing the dose.19-21
Of note, prednisolone tablets are not FDA approved for use in cats.
When cats with asthma or chronic bronchitis are treated with high-dose oral glucocorticoids, clinical signs may resolve despite persistent lower airway inflammation.
Exercise caution in equating absence of clinical signs with absence of airway inflammation.
In cats with subclinical airway inflammation, premature tapering of glucocorticoids based on absence of clinical signs may be detrimental.
Current recommendations to taper therapy based on resolution of clinical signs should be reevaluated.14
DEXAMETHASONE
Formulation → Oral, parenteral
Dose → Oral dexamethasone: 0.1–0.2 mg/kg PO q24h for 10–14 days, then taper over the next 2–3 months until <0.05–0.1 mg/kg q48–72h (if possible)22
Emergency dose → Injectable dexamethasone, dexamethasone sodium phosphate: 0.5–1 mg/kg SC, IV, IM23
Can be used in conjunction with β2-agonist for status asthmaticus (acute asthma attack)
Key Points
Dexamethasone 2 mg/mL injectable is FDA approved for use in cats, while dexamethasone SP 4 mg/mL injectable and dexamethasone tablets are not.
Dexamethasone sodium phosphate usually formulated at concentration of 4 mg/mL (equivalent dexamethasone, 3 mg/mL)
It has been suggested that dexamethasone exhibits greater diabetogenic effects than equipotent doses of prednisolone.11
METHYLPREDNISOLONE
Formulation → Oral, parenteral
Dose → Oral methylprednisolone: 0.8–2.2 mg/kg PO q24h or 0.4–1.1 mg/kg PO q12h for 10–14 days, then taper over next 2–3 months until <0.3 mg/kg q48h (if possible) or to lowest effective dose23
Repository dose → Injectable methylprednisolone acetate: 1–5 mg/kg up to 20 mg/cat IM q4–8wk22-24
May last as long as 2–6 months
Emergency dose → Injectable methylprednisolone sodium succinate: 4–6 mg/kg IV slowly over 2 minutes q2–3h as needed23
Key Points
Methylprednisolone acetate has reportedly led to CHF in cats.<sup9 sup>
May predispose cats to CHF through extracellular hyperglycemia10 but requires further evaluation
Iatrogenic hyperadrenocorticism has been reported in a cat following short therapeutic course of methylprednisolone acetate (20 mg SC weekly for 4 weeks).25
Some cats with preexisting FHV-1 infection may become symptomatic when treated with methylprednisolone acetate.26
Methylprednisolone tablets are FDA approved for use in cats, while methylprednisolone acetate is FDA approved for IM (but not SC) injection.
Inhalant Glucocorticoids
Inhalant glucocorticoids have demonstrated efficacy in reducing airway inflammation in asthmatic cats and may be an alternative to systemic therapy.27 Inhalants appear to result in fewer endocrinologic and immunologic side effects as compared with oral or injectable steroids. Although inhaled glucocorticoids may be an appealing alternative, their expense could be a deterrent.8
Inhalants are administered by an MDI attached to a spacer device and facemask; see the literature for product information and use.27,28
Clinically effective absorption can be delayed, with optimal clinical effects not realized for days, possibly up to 1–2 weeks.
In moderately affected cats, concurrent administration of prednisolone at 0.5–1 mg/kg PO q12h tapered over 2–3 weeks can allow time for maximum inhalant effect.29,30
Caution: Aerosol inhalant steroids are not recommended for emergency management of status asthmaticus because of delayed effect. Instead, a fast-acting ß2-receptor agonist is recommended (see Bronchodilators).29,30
FLUTICASONE PROPIONATE
Formulation → Aerosol inhalant (MDI)
Dose → Available in 3 strengths: 44 or 50, 110 or 125, and 220 or 250 μg MDI q12–36h as needed23 (see Key Points)
Key Points
Most commonly used aerosol inhalant corticosteroid
Shows minimal hypothalamic–pituitary–adrenocortical axis (HPAA) suppression in cats.31
Available in three strengths per actuation, with the labeling varying by country: 44 or 50 µg, 110 or 125 µg, and 220 or 250 µg23
In the U.S., MDIs are labeled by amount of drug delivered at the mouthpiece; elsewhere, they can be labeled by amount of drug delivered from the valve, which accounts for apparent dose differences.32
A recent study has shown that fluticasone propionate doses of 44, 110, and 220 μg q12h are equally efficacious in suppressing eosinophilic airway inflammation in experimental models of feline asthma.<sup31 sup>
In contrast, anecdotal responses indicate that 44 µg fluticasone is not always effective clinically, but 110 µg q12h is effective in managing most cats with mild-to-moderate disease; cats with more serious disease require 220 µg q12h.
It has been suggested that once-daily dosing is occasionally effective.32
FLUNISOLIDE
Formulation → Aerosol inhalant (MDI)
Dose → 250 μg MDI q12h33
Key Points
Because flunisolide suppresses the HPAA, it is not a first-choice inhalant steroid.
However, it may have an index superior to systemically administered corticosteroids.
Flunisolide can be tried if other steroids are not available or effective.
BECLOMETHASONE DIPROPIONATE
Formulation → Aerosol inhalant (MDI)
Dose → 80–160 μg MDI q12–24h32,34
Key Points
Beclomethasone dipropionate is a first-choice inhalant steroid used to treat human asthmatics but has not been well studied in cats.
Veterinarians can try it if other steroids are not available or effective.
It may have more systemic side effects (eg, HPAA suppression) than does fluticasone.
Bronchodilator (Asthmatic Crisis) Therapy
Bronchoconstriction is one of the hallmark features of feline asthma, and severe bronchoconstriction can lead to a life-threatening asthmatic crisis. Therefore, short-acting bronchodilators are important therapeutic drugs, particularly for treating cats in asthmatic crisis.
Usually not indicated for long-term use → Avoid using as monotherapy, as bronchodilators fail to control airway inflammation that exacerbates airway hyperresponsiveness.<sup2 sup>
If corticosteroid therapy alone fails to control clinical signs → Use bronchodilators symptomatically in combination with corticosteroid therapy.
β2-Receptor Agonists
Short-acting β2-receptor agonists are the drugs of choice for treating status asthmaticus and can be used as an early at-home intervention for asthmatic crisis.
β2-receptor agonists should be used only with careful clinical monitoring in cats with preexisting cardiac disease, hyperthyroidism, hypertension, or history of seizures.
TERBUTALINE
Formulation → Oral, parenteral (short-acting)
Emergency dose → 0.01 mg/kg SC, IM, IV
If beneficial, breathing rate will decrease by ~50% within 10–30 minutes.
Can be readministered 30 minutes later at the same dose if minimal effect has been noted
A heart rate approaching 240 bpm indicates that the drug has been absorbed.17,23,32
Long-term oral dose → 0.625–1.25 mg/cat PO q8–12h or 0.1–0.2 mg/kg PO q8–12h17,32,35
Key Points
Terbutaline is the treatment of choice for acute respiratory difficulty when inhaled albuterol therapy is not possible.
Most adverse effects are dose-related and associated with sympathetic stimulation, including
Increased heart rate, tremors, CNS excitement (nervousness), dizziness
Effects are generally transient and mild and do not require discontinuation of therapy.23
Transient hypokalemia has been reported in humans.23
ALBUTEROL SULFATE (USAN) & SALBUTAMOL SULFATE (INN)
Note → Albuterol and salbutamol are the same drug. Albuterol (90 μg/actuation) is the name used in the U.S. as assigned by the U.S. Adopted Names (USAN), and salbutamol (100 μg/actuation) is the name used in the rest of the world as assigned by the World Health Organization (WHO [International Proprietary Name, or INN]).
Formulation → Aerosol inhalant (MDI; short-acting)
Emergency dose → 90 μg (albuterol) or 100 μg (salbutamol) per actuation, ×2 actuations MDI q30min as needed for up to 4–6h23
Key Points
Two enantiomers of albuterol (salbutamol) exist.
R-albuterol (R-salbutamol) is the pharmacologically active form.
S-albuterol (S-salbutamol) is the inactive form and can cause paradoxical inflammation and broncoconstriction.36
Avoid long-term use of albuterol (salbutamol); standard formulations are racemic mixtures.
The R-enantiomer formulation is available but very expensive.
Albuterol (salbutamol) may be considered for intermittent, short-term asthma intervention, but its long-term use for feline asthma management may be detrimental.36
Clinical effects in humans usually occur within 15 minutes and can last 3–4h.<sup37 sup>
Anecdotally, effects are similar in cats.<sup17,32 sup>
SALMETEROL XINAFOATE
Formulation → Aerosol inhalant (long-acting)
Dose → 25 μg for long-term/maintenance use38
Key Points
Salmeterol may be given before bedtime to provide bronchodilation throughout the night or given twice daily in more severe cases in which a β2-receptor agonist is beneficial.
A large U.S. human trial showed statistically and clinically significant increase in asthma-related deaths in subjects receiving salmeterol.39
Warning
Per FDA black label warning for human use, this drug should be used only when nothing else works to control asthma symptoms; its use for the treatment of asthma without a concomitant long-term asthma control medication (eg, inhaled corticosteroid) is contraindicated.
Salmeterol–chlorofluorocarbon (CFC) inhalant has been discontinued in the U.S. since 2002 but is still available in the UK.
FLUTICASONE PROPIONATE–SALMETEROL XINAFOATE COMBINATION
Formulation → Aerosol inhalant (MDI)
Dose → 250 μg fluticasone, 25 μg salmeterol MDI q12–48h32,40
Key Points
Combination inhaler products should only be used to treat asthma not controlled by other long-term asthma-control medication (eg, inhaled corticosteroids).
Methylxanthines
Methylxanthines promote airway smooth muscle relaxation and bronchodilation via phosphodiesterase inhibition and adenosine receptor antagonism23,41 and are generally less-effective bronchodilators than are the β2-receptor agonists.17,32,42,43
THEOPHYLLINE
Formulation → Oral
Dose → 4 mg/kg PO q8–12h17,43
20–25 mg/kg PO q24h for extended-release products44
Key Points
Extended-release products are no longer available in the U.S.44
Generic extended-release theophylline offered from various manufacturers should be avoided because pharmacokinetics vary and are unpredictable.32
Clinicians should consider several known drug interactions.23
Because of its low therapeutic index and pharmacokinetic characteristics, dosage should be based on lean body mass.17,32,43
Because of adverse effects, use theophylline and other methylxanthines cautiously.
CNS stimulation/excitement, insomnia, GI disturbances (eg, vomiting, diarrhea), nausea, polyphagia, PU/PD
Seizures or cardiac dysrhythmias may occur in severe intoxications.23
Therapeutic drug monitoring is advised.23
AMINOPHYLLINE
Formulation → Oral
Dose → 5–6 mg/kg PO q12h32,43
Key Points
Aminophylline should rarely be used for treatment of asthma, as other safer, more efficacious bronchodilators are available (eg, β2-receptor agonist).32
Side effects are similar to those listed for theophylline.
Oxygen
When a cat is in respiratory distress, it is appropriate to provide an oxygen-rich environment. However, oxygen supplementation by mask should not be forced if the cat experiences untoward stress. A mild sedative may aid in decreasing anxiety associated with hypoxia.
Patient handling should also be minimized to avoid worsening respiratory distress.32
Methods of supplemental oxygen delivery → flow-by, face mask, Elizabethan collar canopy, nasal catheter, oxygen chamber
Doses45
Flow-by: flow rate 6–8 L/min to achieve ~25%–45% FiO2
Face mask: flow rate 6–8 L/min to achieve ~35%–55% FiO2
Elizabethan collar canopy: flow rate of 2–5 L/min to achieve ~30%–40% FiO2
Nasal catheter: flow rate of 100–150 mL/min to achieve ~30%–50% FiO2
Oxygen chamber with controlled O2, humidity, and temperature
Antibiotics (Mycoplasma felis)
Mycoplasma felis is a primary pathogen that can mimic or aggravate asthma. The following empirical doses are based on treating upper respiratory M felis infections.
Dose → Medications with efficacy against M felis
Doxycycline: 5 mg/kg PO q12h or 10 mg/kg PO q24h for 2–4 weeks46
Marbofloxacin: 2.75–5.5 mg/kg PO q24h for 2–4 weeks23
Pradofloxacin: 7.5 mg/kg PO q24h for 7 days23,46
Azithromycin: 5–10 mg/kg PO q24h for 2 weeks23
Key Points
Mycoplasma spp are the smallest known prokaryotes, lack a cell wall, and require sterols for growth.
They are considered to be normal commensal organisms associated with the mucous membranes of the upper respiratory system in cats.
M felis has been suggested to cause lower respiratory tract and pleural cavity disease, acting as a primary pathogen and possibly exacerbating clinical signs in cats with asthma.47-52
Tetracycline, fluoroquinolone, and macrolide antimicrobials are most frequently used treatments for respiratory Mycoplasma spp infection in cats.<sup51 sup>
Immunomodulators (Cyclosporine)
In asthmatic patients, immunomodulatory therapy (specifically, cyclosporine) refers to the use of treatment designed to normalize inappropriate responses of the immune system.
Initial cyclosporine dose → 5–7 mg/kg PO q24h23
Doses are empirical and based on those recommended for treating allergic dermatitis in cats.<sup23 sup>
Therapeutic drug monitoring, blood trough level in 72 hours53: 300–600 ng/mL
Most human medical centers perform cyclosporine assays that can be applied to veterinary patients, providing a faster turnaround time than with veterinary laboratories.
Key Points
Cyclosporine can be considered for treating feline asthma in patients with concurrent diseases (eg, diabetes mellitus, severe heart disease) that may contraindicate glucocorticoid therapy.12
Cyclosporine treatment does not appear to inhibit early-phase asthmatic response or mast cell degranulation following antigen challenge in sensitized cats.<sup54 sup>
However, it reduced airway eosinophilia, airway responsiveness, and histologic changes/airway remodeling in an experimental model of feline asthma.55
Cyclosporine is FDA approved for use in cats with atopic dermatitis but not those with asthma.
Further studies are needed to validate its use for treating feline asthma.
Additional Therapies
Omega-3 Polyunsaturated Fatty Acids
Omega-3 polyunsaturated fatty acids (PUFAs) with antioxidant/luteolin provide antiinflammatory effects by inhibiting key inflammatory signaling pathways.
They may have some beneficial effects in reducing airway hyperresponsiveness.2,56
Inhaled Budesonide
Inhaled budesonide at 400 μg/cat MDI q12h has been shown to be well tolerated in asthmatic cats, with improvement in clinical signs.
However, it may suppress the HPAA in some cats.57
Inhaled Lidocaine
Chronic nebulized lidocaine 2% with no preservatives and administered at 2 mg/kg q8h appears to be well tolerated in cats, causing no signs of toxicity.58
Lidocaine decreases hyperresponsiveness and improves airway flow, but it does not reduce airway eosinophilia.
It is not a suitable monotherapy but may serve as an adjunct to other treatments.2,58
Potential Future Therapies
Allergen-Specific Immunotherapy
Has potential to be curative treatment by inducing immunologic tolerance to allergens
Has met with some success in treating human asthmatics2,59
Abbreviated protocol referred to as rush immunotherapy (RIT) has been shown to successfully reduce airway eosinophilia in experimental feline asthma.2,60
Limitations of therapy rest with methods of determining exact (or closely matched) allergens required for inducing immunologic cure.2,61
Sensitivity and specificity of intradermal skin testing and serum allergen testing have so far produced unreliable asthma allergen-specific IgE.2,62
Stem Cell Therapy
May decrease long-term lung remodeling2,63
Tyrosine kinase inhibitor (TKI): masitinib at 50 mg PO q24h64
Stem cell factor is associated with proliferation and activation of mast cells and eosinophils; blockage of this factor is possible with TKIs.2,65
Side effects (eg, severe proteinuria, neutropenia, GI disturbances) may limit the use of TKIs as treatment for feline asthma.2,56,66
Ipratropium (Anticholinergic)
Ipratropium bromide with or without albuterol (inhaled aerosol) is not routinely used in cats at this time, but better potency of this combination may warrant further studies and its possible use in cats in asthmatic crisis.38,67,68
Emergency dose of 20 μg/90 μg MDI (ipratropium bromide–albuterol) has been documented.38,68
Precautionary Warning
Avoid/Ineffective Therapies
Several drug classes have been investigated for treating feline asthma because of their benefits in treating human asthma. However, their efficacy in treating feline asthma has been disappointing and, therefore, these drugs are not recommended at this time.
Cetirizine (antihistamine)69
Cyproheptadine (antiserotonergic and antihistamine)15,69
Zafirlukast (antileukotriene)15
CHF = congestive heart failure, FHV-1 = feline herpesvirus type 1, FiO2 = fraction of inspired oxygen, HPAA = hypothalamic–pituitary–adrenal axis, IBD = inflammatory bowel disease, IgE = immunoglobulin E, MDI = metered dose inhaler, PU/PD = polyuria/polydipsia, TKI = tyrosine kinase inhibitor