Colonic Volvulus & Entrapment in a Labrador Retriever
Kiersten Campbell, DVM, Ocean State Veterinary Specialists, Greenwich, Rhode Island, Bay State Veterinary Emergency Services, Swansea, Massachusetts
Aleisha Michael, DVM, University of Minnesota
Stan Veytsman, DVM, VCA Palm Beach Veterinary Specialists, West Palm Beach, Florida
Clinical History & Signalment
Gunner, a 7-year-old, 77.2-lb (35-kg) neutered male Labrador retriever, was presented for 3 episodes of acute-onset vomiting. His owner reported that the vomitus contained pieces of socks. Gunner also had decreased appetite and thirst, lethargy, and a small amount of diarrhea.
Gunner had been presented with similar clinical signs 2 years prior. At that time, jejunotomy to remove a sock obstruction and a prophylactic right-sided incisional gastropexy were performed, and recovery was uneventful.
Physical Examination
On physical examination, Gunner was bright, alert, and responsive. He was mildly dehydrated (approximately <5%), tachycardic (heart rate, ≈150 bpm), and tachypneic (respiratory rate, ≈50 breaths per minute). He also had apparent mild abdominal discomfort on palpation. Remainder of the physical examination, including rectal examination, was unremarkable.
Diagnosis
Based on Gunner’s history of dietary indiscretion with foreign body obstruction and prophylactic gastropexy, as well as current clinical signs, differential diagnoses included mechanical ileus secondary to foreign body obstruction, functional ileus secondary to gastroenterocolitis, pyloric hypertrophy, pancreatitis, hepatic disease, renal disease, toxicosis, and metabolic disease.
CBC and serum chemistry profile results were unremarkable.
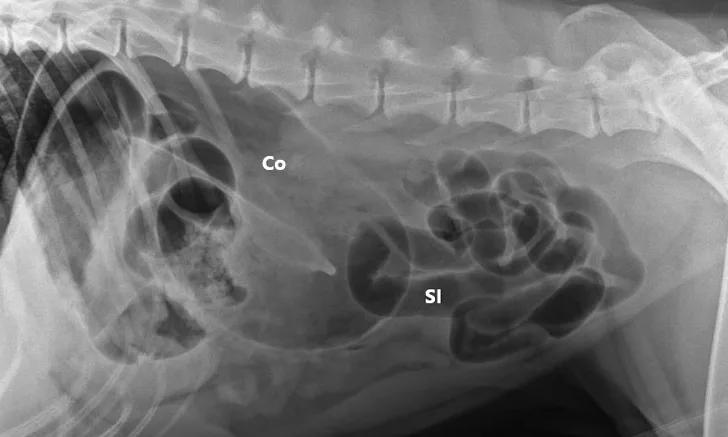
Three-view abdominal radiographs revealed a single bowel loop markedly dilated with gas and amorphous material in the cranial abdomen thought to represent the colon due to its unusual position (ie, could not be tracked from caudal to cranial aspect on lateral radiograph; Figure 1). The small intestines were displaced caudally with no evidence of ileus (ie, gas filled but normal and uniform in diameter), and the descending colon was not fully visualized.
Pneumocologram (ie, negative-contrast colonography) was recommended. An 18-gauge catheter was placed in each of the cephalic veins, and lactated Ringer’s solution (700 mL IV bolus over 20 minutes) was administered for rehydration and maintenance. Maropitant (1 mg/kg IV once) was administered as an antiemetic.
A lubricated 10 French red rubber catheter was inserted rectally and connected to a 60-mL catheter-tip syringe. Air (2 mL/kg) was injected while the anus was occluded by pinching off the anal tissue. Additional 3-view abdominal radiographs revealed normal-diameter, gas-filled small intestines; a markedly gas-distended proximal colon; soft-tissue opacity abnormally located in the right cranial abdomen; and narrowing of the distal lumen of the descending colon (Figure 2). The remainder of the radiographs were unremarkable. Radiographs were assessed by multiple board-certified radiologists, and there was a high index of suspicion for colonic torsion.

FIGURE 1A
Right lateral (A), left lateral (B), and ventrodorsal (C) abdominal radiographs demonstrating marked dilation of a single bowel loop with gas and amorphous material in the right cranial abdomen, suspected to be the colon (arrows). Caudal displacement of the small intestines (SI) can also be seen. The descending colon (Co) is poorly visualized.
Diagnosis: Colonic Volvulus & Colonic Entrapment
Treatment & Management
Gunner was placed under general anesthesia for an exploratory celiotomy, which revealed a transverse and descending colonic entrapment around the intact right-sided incisional gastropexy site with 180-degree counterclockwise colonic volvulus (Figure 3). The entrapment was gently reduced, and the colon was derotated to a normal anatomic position. Colonic tissue appeared erythemic, tissues were grossly normal on palpation, and normal pulsations were palpated in all segments. The colon was deemed viable based on gross examination and clinician experience.
The colon was distended with gas and fluid, and the stomach was distended with gas. Attempts to digitally reduce the gas and fluid in the colon were unsuccessful. An orogastric tube was placed in the stomach, and a lubricated 10 French red rubber catheter was inserted into the rectum and left in place. Audible intestinal borborygmus was appreciated within a few minutes, and the stomach and colon were decompressed of air. Colonic tissues were reassessed and remained grossly normal.
A 4-cm longitudinal, serosal, antimesenteric incision was made using a #11 scalpel blade, starting at the junction of the transverse and descending colon and continuing aborad. A matching 4-cm longitudinal incision was made through the left transversus abdominis muscle.
Left-sided colopexy was completed by apposing the dorsal body wall incision to the lateral colonic incision using 4-0 polydioxanone suture in a simple continuous pattern from caudal to cranial. A matching parallel closure apposed the ventral margin of the body wall incision to the medial margin of the colonic incision. Three additional 3-0 polydioxanone interrupted sutures were placed in the ventral body wall to the medial colonic incision (Figure 4).
The descending colon was unable to contact the previous right-sided incisional gastropexy with cranial traction, and the gastropexy was left intact. The orogastric tube and red rubber catheter were removed; sponge count was confirmed; the abdomen was copiously lavaged with warm sterile isotonic saline; and abdominal closure was performed routinely.
Postoperatively, Gunner continued to receive fluid therapy (lactated Ringer’s solution with 16 mEq/L of potassium chloride, 2.2 mL/kg/hour IV CRI), lidocaine (25-50 µg/kg/minute IV CRI), and fentanyl (2-5 µg/kg/hour IV CRI). He appeared comfortable during hospitalization and began voluntarily eating and drinking within 6 hours postoperatively.
Gunner was discharged within 24 hours postoperatively. Gabapentin (8.3 mg/kg PO every 8 hours for 10 days), codeine (1.2 mg/kg PO every 8 hours for 3 days), trazodone (4.1 mg/kg PO every 8 hours for 10 days), and maropitant (1.7 mg/kg PO every 24 hours for 4 days) were dispensed for the 2-week postoperative recovery period.
Treatment at a Glance
Thorough physical and rectal examinations should be performed in patients presented with acute GI signs.
Early diagnosis and treatment are key to ensuring colonic tissue vitality.
Radiographic findings of colonic torsion include marked gas-filled colonic distention, abnormal location of the ascending or descending colon, and narrowing of the descending colon. The cecum may also be displaced.
Preoperative fluid resuscitation can help stabilize the patient for anesthesia and surgery.
Exploratory celiotomy with colonic derotation and colopexy is recommended for viable tissue.
Prognosis & Outcome
At the 2-week follow-up, Gunner’s abdominal incision had healed without complication. Bowel movements were normal, and there were no subsequent GI concerns at the last follow-up (5.5 months postoperatively). No other issues related to the procedure were reported. Outcome was excellent, with no signs of short-term complications.
Discussion
Colonic torsion (ie, twisting of the colon around its longitudinal axis) and volvulus (ie, pathologic rotation of the colon around its mesenteric axis) are life-threatening conditions that can result in ischemia, necrosis, perforation, sepsis, and death and are defined interchangeably in the literature.1,2
Diagnostic investigation often includes CBC, serum chemistry profile, coagulation profile, and imaging (eg, 2- or 3-view abdominal radiography, negative-contrast colonography, positive barium contrast colonography via enema, abdominal ultrasonography, abdominal CT).
Rotation is described as 90-degree partial torsion, 180-degree counterclockwise torsion around the mesenteric root, 270- to 360-degree longitudinal clockwise torsion, or 360-degree counterclockwise torsion and volvulus when viewed intraoperatively from a ventrodorsal perspective. Torsion and volvulus can occur separately or simultaneously; a combination including entrapment has also been described.2-13
Clinical Presentation
Patients may be presented with nonspecific clinical signs (eg, anorexia, dehydration, lethargy, abdominal distention, vomiting, diarrhea, constipation, tenesmus, hematochezia, dyschezia). Physical examination findings can include pyrexia, shock, and acute abdomen.
Although a direct cause of colonic torsion and volvulus has not been established, predisposing factors include patient history of GI disease (eg, lymphoplasmacytic enteritis), parasitism with or without intussusception, previous GI surgery (eg, foreign body obstruction) that may have led to resection of the duodenocolic ligament or adhesion formation, entrapment around a previous gastropexy site or through a mesenteric rent, exocrine pancreatic insufficiency, and hypoadrenocorticism.9 The condition can be idiopathic.9 According to the authors, neoplasia has not been associated with colonic torsion or volvulus. Increased GI motility may be a predisposing factor for colonic torsion and volvulus or entrapment.9
No age or sex predisposition has been identified, but large- and giant-breed dogs are predisposed.9 The most commonly reported breeds are Great Danes, German shepherd dogs, and Labrador retrievers. Other reported breeds include bullmastiffs, cane corsos, collies, German shorthaired pointers, golden retrievers, Gordon setters, hounds, Irish water spaniels, Irish wolfhounds, redbone coonhounds, Russian terriers, Siberian huskies, and vizslas.2-17 Colonic torsion and volvulus have also been reported in an English toy springer spaniel and a domestic shorthair cat.18,19
Surgical & Nonsurgical Management
Nonsurgical management has been described, but exploratory celiotomy remains the standard of care.3,9,13 Surgical correction may include decompressive colocentesis, an intraoperative enema to relieve colonic material, colotomy to remove colonic material, derotation of the colon to the appropriate anatomic location, temporary colostomy, colectomy or colonic resection and anastomosis with pubic osteotomy if access to the rectum is required, or colopexy.9,20 The colon is occasionally derotated into normal anatomic positioning during surgical exploration.
Colopexy is the treatment of choice to prevent future torsion and volvulus, although recurrence has been reported. Three forms of colopexy have been described: left-sided colopexy for the descending colon, right-sided colopexy for the ascending colon, and gastrocolopexy for the transverse colon.21 Colopexy can be performed via direct suture, abrasion/scarification with the back of a scalpel blade or sterile radiopaque gauze, or colonic serosal incision and 2-layer apposition with a matching caudal transversus abdominis muscle incision.21
The authors are unaware of any prospective studies that have compared nonsurgical and surgical management of colonic torsion and volvulus or colopexy treatments. Early identification and surgical intervention should be considered the treatment of choice. Owners of dogs that undergo gastropexy should understand there is a small risk for subsequent colonic entrapment around the gastropexy site.2,9
Prognosis
Overall prognosis for colonic torsion is good, depending on tissue viability. Prognosis is variable and can be guarded to fair in patients with colonic perforation and/or septic peritonitis that require colonic resection and anastomosis. Colonic torsion/volvulus appears to have a more favorable prognosis than mesenteric volvulus. Reported postoperative complications include failure of the colopexy with recurrence of colonic torsion, an intact colopexy with recurrence of colonic torsion, ongoing gastroenterocolitis, and ileus.3
Take-Home Messages
Etiology of colonic torsion and volvulus remains unknown; GI disease and previous GI surgery are predisposing factors.1
Colonic torsion and volvulus or entrapment should be considered in patients with nonspecific GI signs.
Contrast radiography and CT of the colon are useful for rapid diagnosis of colonic torsion and volvulus.
Early surgical intervention is the current standard of care.
Recurrence is rare.
Dogs with prior gastropexy may be at higher risk for colonic entrapment, but further studies are warranted.9
Listen to the Podcast
Dr. Veytsman joined the podcast to discuss the common presenting signs that this very uncommon problem shares with other acute abdominal conditions and much more.