Vertebral Magnetic Resonance Imaging
MRI is an excellent tool for assessing vertebral column disorders in domestic species.
Magnetic resonance imaging (MRI) has revolutionized the assessment of vertebral column disorders in both humans and animals. It is noninvasive, provides the clinician with data in multiple image planes, and offers outstanding soft tissue contrast. Certain imaging features may be associated with pathologic processes and can be of prognostic value. Furthermore, MRI may be the only reliable antemortem means of diagnosing certain diseases, such as ischemic myelopathy.
In human medicine, MRI has largely replaced both myelography and computed tomography (CT) as the imaging study of choice for patients with vertebral column disease, and this transition has already begun in veterinary medicine.
AdvantagesThe selection of an appropriate imaging modality should be based on its sensitivity and specificity for detecting disease and associated adverse events as well as for identifying prognostic data. MRI offers equivalent and often superior sensitivity and specificity when compared with other imaging modalities used in human vertebral column diseases. Evidence-based comparisons between modalities are more limited in veterinary medicine, but currently available data do parallel what is known in human medicine.1-7
Use in Clinical Disease Conditions
Disk HerniationIn humans, the accuracy of MRI for detecting disk herniation has been shown to be equivalent to or better than either CT or myelography.1 Of importance, much of these data were generated in the 1980s, when the capabilities of MRI were limited by field strength and software.
Comparative data between MRI and other modalities for cervical and thoracolumbar disk herniation in dogs does not exist. In some instances, neither myelography nor CT has identified disk herniation as clearly as MRI has (Figure 1).
Figure 1. Transverse CT and MRI in a dog with paraplegia. CT shows a subtle hyper- to iso-attenuating, right-sided ventral extradural compressive lesion (A and B) at the level of L2-L3 (arrowhead in A). Transverse T2-weighted MRI shows a large, hypointense, ventral and right lateral extradural compressive lesion (C and D) that nearly entirely effaces the cross-sectional area of the vertebral canal (small arrow in D). The visible spinal cord is reduced to a small crescent (large arrowhead in C) and is hyperintense, which may indicate the presence of intraparenchymal edema or necrosis. Surgical exploration confirmed the presence of severe spinal cord compression due to disk extrusion.

In addition, several studies have shown that T2-weighted hyperintensity within the spinal cord of dogs with thoracolumbar disk herniation was negatively associated with long-term ambulatory outcome.2,3 In one study, the ratio of T2 hyperintensity to the length of the L2 vertebral body (T2 length ratio) was predictive of outcome independent of physical examination-based neurologic score, with each unit of the T2 length ratio increasing the odds of failure by 1.9-fold.3
Fibrocartilaginous EmbolismIschemic myelopathy (from fibrocartilaginous embolism or other causes) is a spontaneous group of vascular diseases of the spinal cord. Gandini and coworkers found that nearly 75% of dogs with ischemic myelopathy due to fibrocartilaginous embolism had normal myelogram results; the most common abnormality in these dogs was intramedullary pattern, which has also been recognized in cases of myelitis, neoplasia, trauma, and disk herniation.4
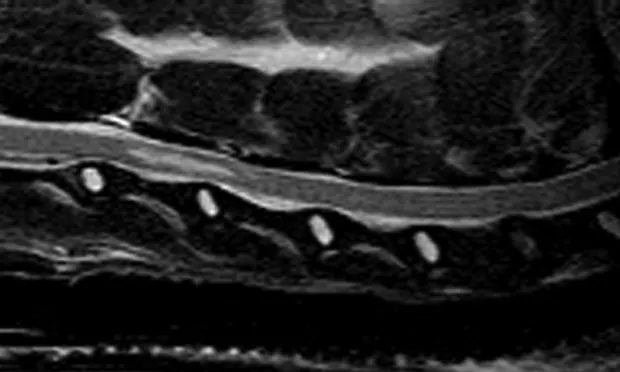
In one recent study, 78.8% of dogs with suspected ischemic myelopathy had abnormal MRI results, which were believed to be relatively specific for this group of diseases (Figure 2).5 In a subsequent report, outcome was adversely affected when lesions within the spinal cord spanned more than 2 vertebrae or when the cross-sectional area of the lesion exceeded 67%.6
Figure 2. Sagittal T2-weighted MRI (A) and lateral cervical myelography (B) in a dog with nonambulatory tetraparesis. The myelogram shows preserved dorsal and ventral subarachnoid contrast columns with possible mild disk-associated compression at C6-C7.

Significant T2-weighted hyperintensity is present within the spinal cord overlying the C3-C4 vertebrae (arrowheads in A). This lesion was consistent with fibrocartilaginous embolic myelopathy (FCEM) based on other MRI features and was confirmed as FCEM on necropsy.
Cervical SpondylomyelopathyData comparing MRI and myelography are available from one study in dogs with cervical spondylomyelopathy.7 Both modalities identified the location of the main lesion with reasonable inter-rater agreement. Signal changes within the spinal cord were identified by MRI in 10 of 18 dogs,7 suggesting that this modality could assist in locating compressions associated with significant injury.
Other DiseasesIntravenous contrast can be administered to animals undergoing veterbral column MRI. In certain disease states in which the blood-spinal cord barrier has been disrupted or neoangiogenesis has occurred, contrast material can extravasate into surrounding abnormal tissue.
Contrast is often provided when neoplastic or inflammatory lesions are suspected. It is well known that certain tumor types commonly enhance strongly (eg, meningioma), whereas enhancement is uncommon in other lesions (eg, ischemic myelopathies).
Nonetheless, the ability of postcontrast studies to differentiate among diseases has not been carefully studied in veterinary medicine. Further, contrast enhancement is frequently identified in nonneoplastic diseases such as disk herniation.8
Disadvantages
The major disadvantages associated with MRI are the lack of availability, issues related to patient size, patient and operator safety, the need for general anesthesia, limited field of view, and the time required to obtain a scan.
Lack of FacilitiesAlthough the number of veterinary MRI centers is expanding, many specialty clinics evaluating animals with vertebral column disorders do not have ready access to MRI facilities.
Patient Size ConstraintsThe physical size of patients can limit the use of MRI in veterinary medicine. Available MRI bore diameter and receiver coils may not accommodate the wide variety of patient sizes in veterinary medicine.
Safety ConcernsSafety is also a concern. Veterinary patients with loose metal debris close to vital structures may be at risk for metal heating or fragment migration, and the susceptibility artifact generated by the presence of metal adjacent to structures of interest may hinder image interpretation. The degree to which this is an issue depends on the ferromagnetic and paramagnetic properties of the metal and its volume. Microchips rarely impact the diagnostic value of vertebral column MRI, for example, but patients with cardiac pacing devices cannot be scanned due to magnetic field interference.
Technical MRI staff must be well versed in appropriate safety protocols. Metal instruments cannot come near an MRI machine as they can be strongly drawn toward the bore, which may lead to injury.
Anesthesia and MonitoringGeneral anesthesia is almost uniformly required to perform MRI on domestic species, and technicians must be proficient in anesthetizing these patients. Specialized anesthesia machines and monitoring equipment are required, and patient monitoring equipment in particular has certain limitations associated with interference.
MRI artifacts may be produced by monitoring equipment, and radiofrequency pulses associated with MRI acquisition may hinder readings obtained on monitoring equipment. In my experience, these limitations can be easily overcome, but they are equipment-dependent.
Limited Field of ViewA field of view (the region that can be imaged) must be selected with vertebral column MRI. The size of the field of view varies between different units and scan protocols. Low-field (<1.0 Tesla [T]) and older MRI units may be particularly susceptible to this limitation. Newer, high-field MRI units can subvert field of view limitations using various techniques.
Scan TimeFinally, the time required to perform an MRI study is generally longer than that required for vertebral column CT. It must be remembered that MRI field strength, software, and the number/type of pulse sequences selected highly influence scan times. The time required to scan a particular region of interest varies from 10 to 20 minutes (eg, with a modern 3-T magnet) to 1 to 2 hours (with a low-field or older MRI unit).
Reliability of ResultsAs outlined here, not all MRI units are equal. Field strength, software, receiver coils, protocols, personnel operating the machine, and other factors heavily influence image quality—and thus the reliability of the results.
Economic ImpactThe cost associated with MRI is greater than that for traditional imaging modalities. At our center, the cost for regional vertebral column MRI is about twice as much as that for myelography.
When determining which diagnostic study to undertake, cost must be balanced with the accuracy of the study as well as study-related adverse events and prognostic data. As previously stated, CT and myelography cannot reliably identify certain vertebral column diseases. Likewise, myelography may be less specific than MRI for identifying sites of extradural compression (eg, cervical spondylomyelopathy).7
Adverse events associated with myelography in one study included seizures (28%) and worsening of neurologic signs (33%).7 Although many of these adverse events associated with myelography are transient, there is a case to be made for avoiding even transient patient morbidity. Finally, MRI can provide a greater amount of prognostic data than myelography or CT, which is certainly valuable.
How MRI Works
The BasicsMRI is a technique for rendering high-contrast images of structures by manipulating the energy state of protons, which make up approximately 70% of most tissues. The MRI machine uses an extremely powerful magnet to orient all protons in 1 direction. A radiofrequency pulse is then delivered that flips protons into a high-energy orientation. Protons are then allowed to return to their original energy state, which is termed relaxation. Relaxation occurs in multiple planes and leads to the release of energy (known as signal), which is detected via a receiver coil. A computer is used to display signal data as an image.
Image ContrastThe contrast characteristics of images (referred to as image weighting) can be altered by changing when and how protons are flipped and when the machine “listens” for energy release. Common weightings include T1, T2, T2*, fluid attenuated inversion recovery (FLAIR), and short tau inversion recovery (STIR). T2-weighted images are often used to detect pathology such as edema, necrosis, or hemorrhage, which appear bright, or hyperintense, on the resulting image.
Contrast enhancement: Extravasation of intravenous contrast material into parenchyma, which is visible on MRI as hyperintensity. Enhancement may indicate neoangiogenesis or blood-spinal cord barrier breakdown.
CT–myelography: An imaging study in which iodinated contrast is injected into the subarachnoid space, after which a CT image is generated.
CT reconstruction: A technique whereby CT images obtained in a certain plane (ie, transverse, dorsal, sagittal) can be reformatted into a different plane. This technique may enhance lesion visualization.
Field of view: The anatomic area visualized in MRI.
Field strength: The strength of the magnetic field an MRI generates, which is usually measured in Tesla. Higher-field magnets produce a stronger signal, which usually translates into better image quality and/or more rapid image acquisition.
Gradient: Small differences in magnetic field produced by MRI that are used to help locate where signal originates within a patient.
Hyperintensity: A state in which the MRI signal of tissue is higher than normal. Hyperintense lesions appear bright on resulting images.
Hypointensity: A state in which the MRI signal of tissue is lower than normal. Hypointense lesions appear dark on resulting images.
Image weighting: The contrast characteristics of an image. Using multiple image weightings enhances lesion visualization and determination of underlying pathology.
Magnet bore: The cylindric opening within an MRI unit into which the patient is placed.
Pulse sequence: The timing of radiofrequent pulses and receiver coil detection of signal that determines image weighting.
Radiofrequent pulse: A short-duration radiofrequent wave that changes the orientation of protons within the patient and ultimately allows signal to be released as protons relax to a lower energy state.
Receiver coil: A coil placed around an anatomic area of interest to allow the detection of signal.
Signal: The brightness of an image, which relates to the amount of nuclear magnetic resonance detected by a receiver coil.
VERTEBRAL MAGNETIC RESONANCE IMAGING • Jonathan M. LevineReferences
1. Lumbar herniated disk disease and canal stenosis: Prospective evaluation by surface coil MR, CT, and myelography. Modic MT, Masaryk T, Boumphrey F, et al. Am J Roentgenol 147:757-765, 1986.2. Prognostic value of magnetic resonance imaging in dogs with paraplegia caused by thoracolumbar intervertebral disk extrusion: 77 cases (2000-2003). Ito D, Matsunaga S, Jeffrey ND, et al. JAVMA 227:1454-1460, 2005.3. Magnetic resonance imaging in dogs with neurologic impairment due to acute thoracic and lumbar intervertebral disk herniation. Levine JM, Fosgate GT, Chen AV, et al. J Vet Intern Med 23:1220-1226, 2009.4. Fibrocartilagenous embolism in 75 dogs: Clinical findings and factors influencing the recovery rate. Gandini G, Cizinauskas S, Lang J, et al. J Small Anim Pract 44:85-89, 2003.5. Magnetic resonance imaging findings and clinical associations in 52 dogs with suspected ischemic myelopathy. De Risio L, Adams V, Dennis R, et al. J Vet Intern Med 21:1290-1298, 2007.6. Association of clinical and magnetic resonance imaging findings with outcome in dogs suspected to have ischemic myelopathy: 50 cases. De Risio L, Adams V, Dennis R, et al. JAVMA 233:129-135, 2008.
Comparison of magnetic resonance imaging and myelography in 18 Doberman pinscher dogs with cervical spondylomyelopathy. da Costa RC, Parent J, Dobson H, et al. Vet Radiol Ultrasound 47:523-531, 2006.8. Contrast enhancement of extradural compressive material on magnetic resonance imaging. Suran JN, Durham A, Mai W, Seiler GS. Vet Radiol Ultrasound 52:10-16, 2011.