Urinary Obstruction: Treatment Measures
Daniel Degner, DVM, Diplomate ACVS, Michigan Veterinary Specialists, Auburn Hills, Michigan
Urinary obstruction is a common condition seen in both dogs and cats. In dogs, acute obstruction is typically caused by urinary calculi lodged in the urethra, while in cats mucus plugs, crystalline plugs, and stones frequently cause obstruction. Other causes in dogs include neoplasia, polyps, scar tissue, strictures, or other functional abnormalities. Within 12 to 24 hours after complete urinary obstruction, serious metabolic disturbances can develop, including metabolic acidosis, azotemia, hyperphosphatemia, and hyperkalemia.
Assessment & Stabilization
Critical care stabilization, including crystalloid fluid therapy, cardiac stabilization, and potentially decompressive cystocentesis, should be initiated before relieving any urinary obstruction (see assessment and stabilization checklists). Because hypothermia can be found in advanced stages of urinary obstruction, the patient should be wrapped in a warming blanket. Cardiac rhythm should be assessed with an ECG and in-house stat blood work conducted to evaluate electrolytes, acid-base status, and azotemia.
If hyperkalemia is affecting cardiac function, administration of insulin and IV glucose or calcium gluconate may be beneficial. If the patient is obtunded, general anesthesia should be avoided during the initial attempt to relieve urinary obstruction Lateral abdominal radiography should also be performed to assess the causes of obstruction prior to correction.
Related Article: Urinary Obstruction in Male Cats
Hints for Urinary Obstruction Relief
For Dogs
A combination of lidocaine 2% and sterile K-Y jelly (Johnson & Johnson, k-y.com) may be mixed in a syringe and injected into the urethra via a urinary catheter after occluding the penile tip in males. Absorption of lidocaine should not cause systemic toxicity, even in patients with cardiac arrhythmias. The mixture should sit for approximately 10 minutes. This may relieve urethrospasm and increase the likelihood of flushing urethral calculi into the bladder.
If this is ineffective, general anesthesia and epidural injection of bupivacaine and morphine may be needed to relax the urethra. An appropriately sized urinary catheter is passed retrograde to the level of the urinary obstruction. A gloved finger via the rectum is used to compress the urethra proximal to the obstructing stone.
Saline is injected via the catheter to distend the urethra, then the urethral compression with the finger is released and the urinary stone flushed into the bladder. If this is unsuccessful, the process is repeated. If the stone cannot be retropulsed back into the bladder and the patient has major metabolic derangements, a temporary cystostomy tube (Stamey or nephrostomy catheter) can be inserted percutaneously into the bladder. After electrolyte abnormalities, acidosis, and azotemia have resolved, urethrostomy is performed.
For Cats
Unless the cat is obtunded, sedation or general anesthesia is usually required to relieve urethral obstruction. The tip of the penis should be massaged to loosen mucus or crystalline plugs. The penis is extruded and pulled caudally to straighten out the urethral path, and the prepuce is grasped at its reflection. A 22-gauge lacrimal catheter can be used to flush the urethra. Other options would include the use of an olive-tip catheter or an open-ended Tomcat catheter. After relieving urinary obstruction, a 3-French red rubber catheter (or other soft catheter) should be placed and connected to a closed urinary collection system.
Initial Assessment Checklist
Check for hydration, shock, and hypothermia
Obtain ECG
Evaluate electrolytes, acid-base status, and azotemia
Perform abdominal radiography
Initial Stabilization Checklist
Warm the patient
Start IV crystalloid fluid therapy
Address hyperkalemia if heart is affected
Inject IV calcium gluconate
Inject IV dextrose and regular insulin
Treat metabolic acidosis only if very severe
Relieve urethral obstruction
Perform cystocentesis to empty bladder if urethral obstruction cannot be relieved
Step-by-Step: Urinary Obstruction
What You Will Need
Needle holder
Curved mosquito forceps
Straight mosquito forceps
Adson thumb forceps
Severin tenotomy or iris scissors
Mayo scissors
Scalpel handle
No. 15 and 11 scalpel blades
Small Gelpi retractors
8-French red rubber catheter
Open-ended Tomcat catheter
5–0 Prolene suture (ethicon.com) and RB-1 taper point needle
12-mL syringe
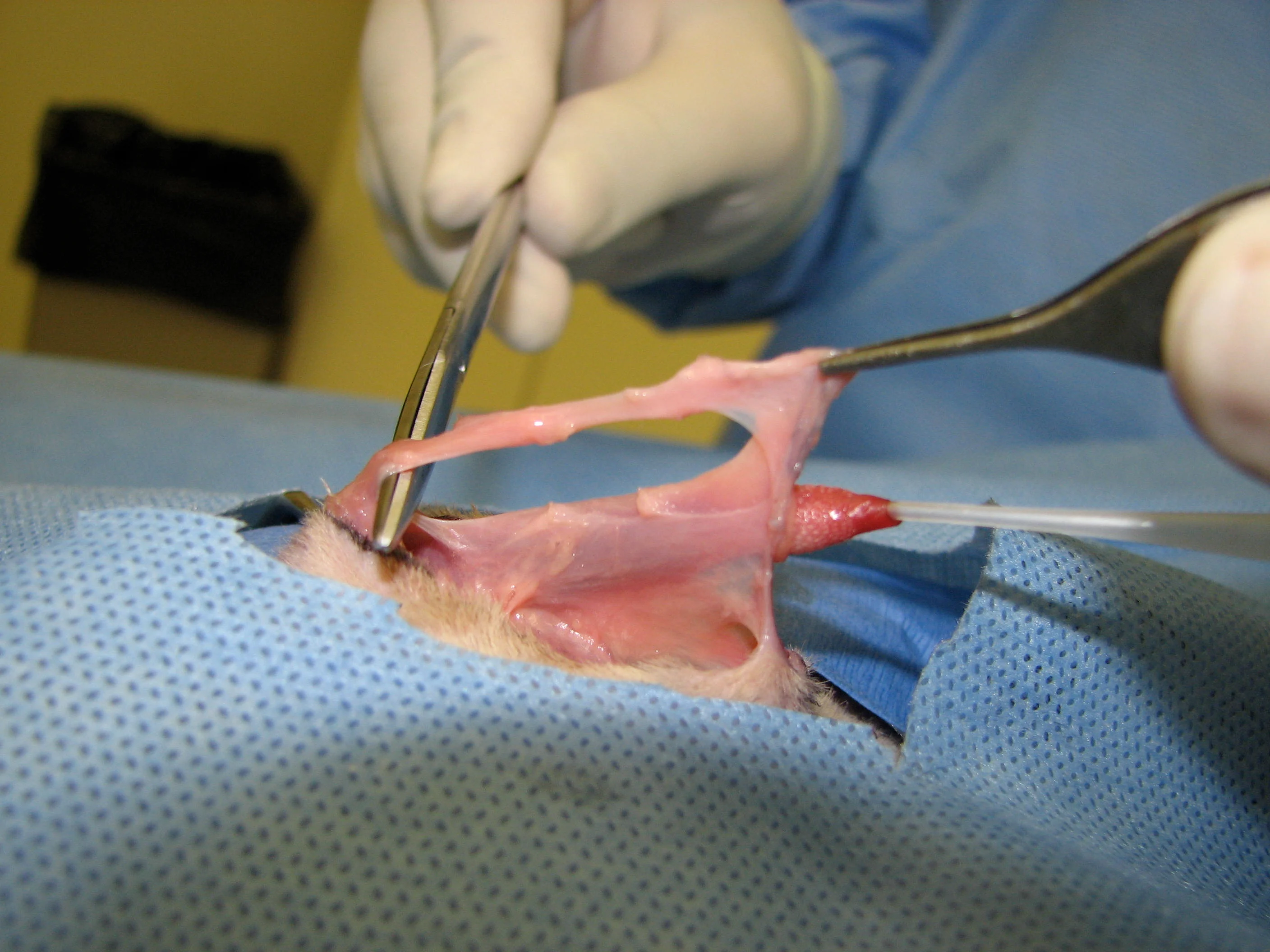
Feline Perineal Urethrostomy
Most cats that develop urinary obstruction do not require surgery unless the obstruction is caused by urinary calculi that could not be medically dissolved or have recurrences of urinary obsrtuction, regardless of cause. Complications could include hemorrhage, leakage of urine into subcutaneous tissues with subsequent tissue necrosis, bacterial cystitis, and urethral stricture.1
The traditional positioning for feline perineal urethrostomy is ventral recumbency with the hindlimbs hanging over the end of the operating table. An alternate position is dorsal recumbency, which allows the surgery to be performed more easily than traditional positioning does.

STEP 1
With the patient in a V-trough and the hindlimbs pulled cranially, place a small towel under the patient’s hindquarters so the perineal region is oriented toward the surgeon.
Step-by-Step: Urinary Obstruction Canine Scrotal Urethrostomy

STEP 1
With the dog in dorsal recumbency, insert a urinary catheter (if possible) into the bladder. However, if the dog has a nonreducible stone lodged at the base of the os penis, this step is not possible and scrotal urethrostomy may be indicated. Other indications for scrotal urethrostomy include penile tumors, recurring urinary obstruction, strictures of the urethral distal to the scrotal urethra, and penile necrosis from iatrogenic trauma during castration (penile ligation).
In intact males, scrotal ablation with castration is performed. If the patient is neutered, a 3-cm skin incision is made starting at the caudal aspect of the pelvis and extending cranially. The subcutaneous tissues are removed from the ventral aspect of the penis. Take note that the retractor penis muscle covers the corpus spongiosum.
Author Insight
Bleeding is expected and will continue until the procedure has been completed.
Postoperative Canine Care
Select an oral narcotic and NSAID for postoperative analgesia.
Prescribe a sedative if excitement causes bleeding at the surgical site.
Prescribe antibiotics for 14 days based on culture and sensitivity findings or empirical selection.
Keep Elizabethan collar on dog for 2 weeks.
Postoperative Feline Care
Keep Elizabethan collar on cat for 2 weeks.
Prescribe oral buprenorphine as needed for the treatment of pain.
Use commercial paper cat litter or shredded paper.
Prescribe antibiotics for 14 days after surgery (selection based on urine culture and sensitivity results or empirically based).
Remove nonabsorbable sutures in 10 to 14 days.
At 2 weeks and 8 weeks after surgery, check the urethrostomy site for patency to determine whether urethral stricture has developed (tip of curved mosquito hemostat should easily insert into the urethral ostium).
ECG = electrocardiogram, IV = intravenous, NSAID = nensteroida antiinflammatory agent
Related Article: Canned Cat Food to Avoid Feline Urinary Obstruction