Tracheal Collapse: Extraluminal Rings & Tracheal Stents
Chick Weisse, VMD, DACVS, Animal Medical Center
Tracheal collapse, or tracheal chondromalacia, is a progressive, degenerative condition of the hyaline cartilage rings that support the tracheal lumen. Weakening of the trachealis muscle contributes to the loss of tracheal lumen during various phases of respiration. The resulting clinical syndrome typically manifests as a "goose honk" cough with varying degrees of dyspnea and is most commonly identified in toy breeds. Conservative management techniques and medical management (Table 1) can be useful to palliate clinical signs for years; however, more aggressive treatment is often required for animals in which these conventional treatments eventually fail.
Always pursue aggressive medical therapy before attempting more invasive techniques-invasive techniques are essentially salvage procedures associated with considerable risk. In addition, other concurrent conditions, such as underlying pulmonary, cardiac, laryngeal/upper airway, and endocrine disorders, should be appropriately addressed before invasive tracheal procedures are considered. If conservative therapy fails to provide a reasonable quality of life for the patient, extraluminal tracheal rings and tracheal stents are the more invasive treatments currently available. There is a tendency to compare these two treatment options; however, both are important in managing this frustrating disease process.
Table 1: Conservative Management Options
Step-by-Step: Applying Tracheal Extraluminal Rings & Stents
Step 1
Diagnosis. Accurate diagnosis of the location of the collapse is important before choosing which technique to perform or recommend. Routine radiography can be useful for diagnosis of concurrent conditions and the presence of tracheal collapse, but more dynamic studies are necessary to fully appreciate the extent of the collapse. During inspiration, the subatmospheric airway pressures generated in the cervical trachea lead to collapse in that location; during expiration, increased intrathoracic pressures lead to collapse of the intrathoracic trachea. Individual static radiographs may fail to document the full extent of the collapse as shown above, which is the same dog during two different phases of respiration (cervical tracheal collapse during inspiration and intrathoracic tracheal collapse during expiration).

Procedure Pearl
At least one suture of each ring must engage the dorsal trachealis muscle-otherwise this muscle will continue to collapse within the tracheal lumen.
Step 2
Rings or stent. Whether to use rings (A) or a stent (B) remains one of the most difficult and controversial decisions to be made during treatment of tracheal collapse. The decision is ultimately based on individual factors; however, some basic guidelines can be followed (Table 2). In general, extraluminal tracheal ring surgery is associated with high risk in the immediate postoperative period. Patients typically have a good recovery from stent placement; however, there is potential risk for stent fatigue and fracture in these patients over the long term. Regardless of the treatment used, a comprehensive discussion with the client is important to ensure that what the surgery can and cannot accomplish is clear. Tracheal collapse is progressive, and all current treatments are purely palliative.
Most patients will still require lifelong medical treatment after ring or stent placement. In addition, concurrent bronchial collapse seems to carry a worse long-term prognosis; however, such patients may still benefit from treatment.

Procedure Pearl
Typically, a stent diameter approximately 10% to 15% greater than the maximal tracheal diameter is chosen to ensure proper seating of the stent within the tracheal mucosa and to minimize migration.
Table 2: Ring or Stent?
Step 3
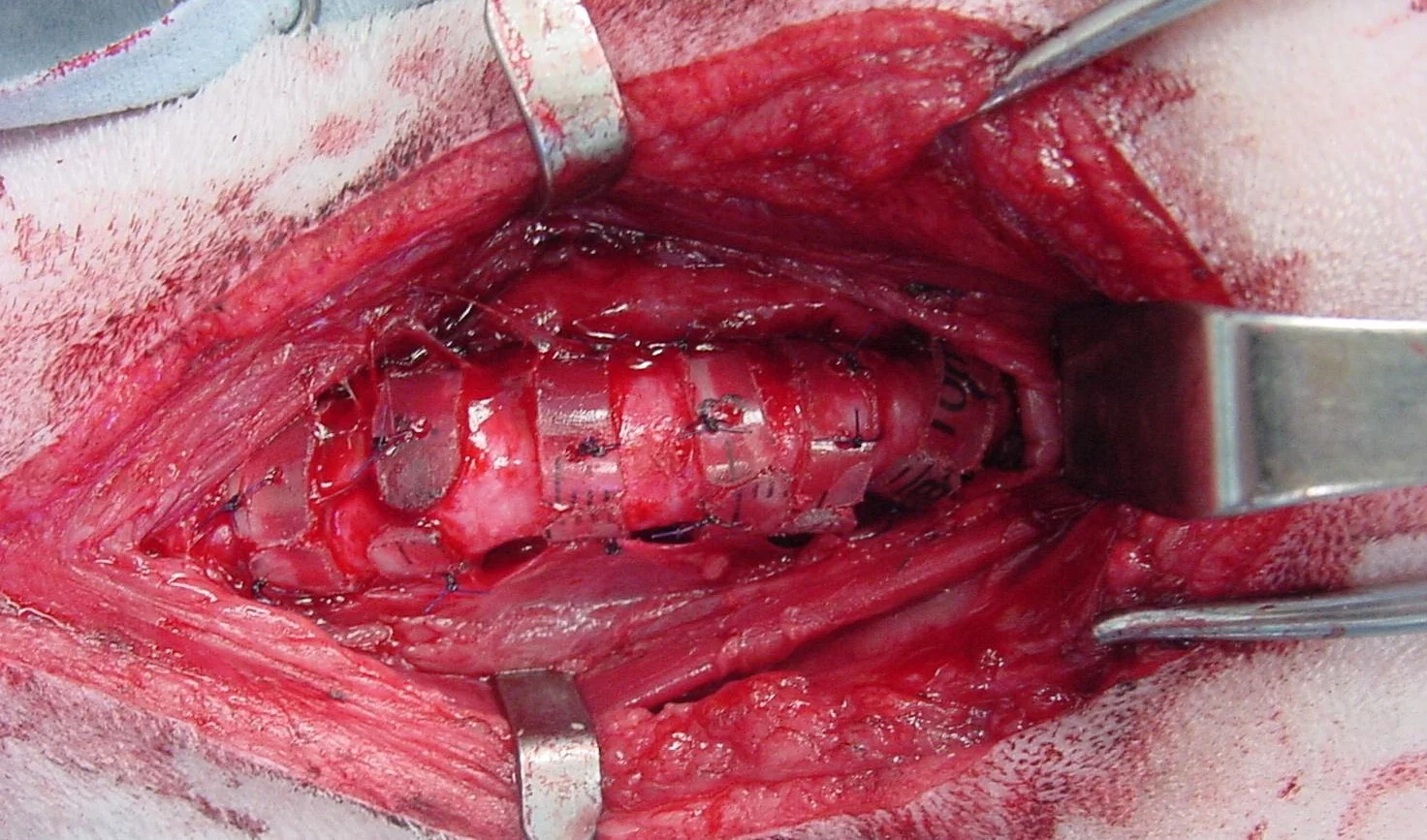
Tracheal ring placement. Place the patient in dorsal recumbency. Make a standard ventral midline cervical incision from the larynx to the thoracic inlet. Separate the subcutaneous muscles and paired sternohyoid muscles by using sharp and blunt dissection to expose the trachea. Take extreme care to avoid stretching or damaging the recurrent laryngeal nerves (A) that course dorsolaterally along the trachea-such trauma can result in laryngeal paralysis. Use curved or right-angled hemostats to facilitate gentle creation of narrow fenestrations around the trachea (B) in order to pass the tracheal rings. The rings are made from polypropylene syringes, or prefabricated rings can be purchased (New Generation Devices, www.newgenerationdevices.com).
Pass four or five polydiaxanone sutures (3-0 or 4-0) around each ring and the tracheal cartilage. Space the rings approximately 5 mm apart, and move the endotracheal tube after placement of each ring to make certain it has not been engaged by a suture (C). Postoperative care typically involves environmental oxygen enhancement as needed, injectable analgesia, intravenous fluids, and supportive care. Antitussives, antiinflammatories, and antibiotics are used on a case-by-case basis.
Procedure Pearl
Aggressive antitussive therapy is necessary following stent placement, particularly in patients with concurrent bronchial collapse, to minimize stent cycling and metal fatigue that occurs during coughing episodes.

A & B
Step 4
Tracheal stent placement. Place the patient in lateral recumbency. Advance a hydrophilic guidewire and marker catheter combination down the esophagus under fluoroscopic guidance. Using positive-pressure ventilation (20 cm H2O), take a radiograph and extrapolate maximal tracheal diameter measurements using the known measurements from the esophageal marker catheter (A). Advance the delivery system and stent down the trachea (B). Withdraw the delivery sheath under fluoroscopic guidance to observe accurate placement of the stent. After complete stent deployment, remove the delivery system and take a radiograph to confirm appropriate stent placement and restored tracheal lumen (C). Postoperative care typically involves environmental oxygen enhancement if necessary as well as continued antitussive therapy (hydrocodone) and antiinflammatory agents (prednisone). Postoperative antibiotics are prescribed if a concurrent airway infection is documented or suspected.
