Top 5 Juvenile Orthopedic Conditions
Pilar Lafuente, DVM, PhD, DACVS-SA, DECVS, DACVSMR, CCRT, PGDipl Vet Ed, FHEA, MRCVS, Universidad Internacional de La Rioja, Logroño, Spain, VetCT, Cambridge, United Kingdom
Many orthopedic conditions can affect dogs and cats. Some start at an early age, with consequences that may remain throughout the animal’s life. Joint pathologies are of particular concern because of the likely development of secondary osteoarthritis (OA), a common cause of chronic pain and lameness in adult dogs. Although clinicians may be presented with various congenital deformities and conditions, the common orthopedic pathologies found in juvenile patients include hip dysplasia, elbow dysplasia, medial patellar luxation (MPL), shoulder osteochondritis dissecans (OCD), and panosteitis.
1. Hip dysplasia
This pathology has a multifactorial etiology that affects the coxofemoral joint, most commonly in large-breed dogs (especially the German shepherd dog), but can also affect small-breed dogs and cats. Genetic and environmental factors can lead to joint laxity, which subsequently causes abnormal development of the acetabulum and femoral head, ultimately resulting in OA. Diagnosis in young patients is based on clinical signs (eg, difficulty in rising, swinging of the hindlimbs, pain, subluxation and laxity of the femoral head [Ortolani test]). Radiographic findings that confirm hip dysplasia are joint subluxation, incongruency, and early degenerative changes (Figure 1).
Related Article: Canine Hip Dysplasia Part 1
Figure 1. Ventrodorsal radiograph of the pelvis in a 12-month-old Labrador retriever with bunny-hopping and pain on extension of the hips. Bilateral coxofemoral subluxation and mild OA are evident.

Treatment depends on the severity of clinical signs; if mild, a nonsurgical approach (eg, weight management, NSAIDs, joint supplements, exercise modification, physiotherapy) can be elected. Some surgical therapies are performed during early stages of the disease, before skeletal maturity and development of OA, to relieve clinical signs and limit disease progression.
Figure 2. Postoperative ventrodorsal radiograph of the pelvis after triple pelvic osteotomy.

Case selection is important, as some factors (eg, age, subluxation and reduction angles, acetabular coverage of the femoral head) may affect the success of these procedures (eg, juvenile pubic symphysiodesis, triple pelvic osteotomy [TPO, Figure 2], double pelvic osteotomy [DPO]). Salvage procedures (eg, total hip replacement, femoral head and neck excision) are usually reserved for severe cases that do not respond to conservative treatment and are performed after growth has ceased.
2. Elbow dysplasia
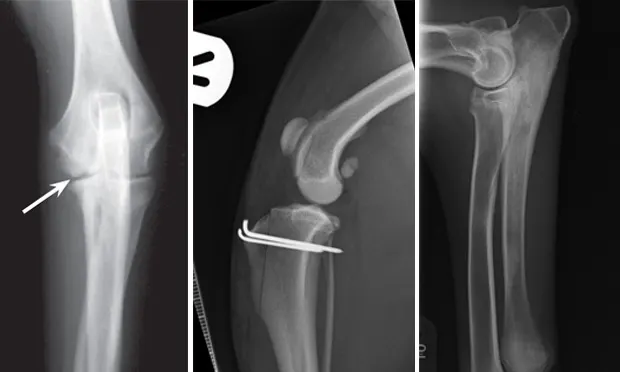
Elbow dysplasia is an umbrella term for several conditions (eg, ununited anconeal process [UAP], medial coronoid disease [MCD], osteochondrosis [OC]/OCD, incongruency) resulting in OA. Most patients are affected by only 1 or 2 of these conditions at the same time (eg, fragmented medial coronoid process, humeral OCD). The causes are multifactorial; genetic and environmental factors are involved. Dogs present with unilateral or bilateral lameness or stiffness of the forelimbs with effusion, pain, and decreased range of motion of the elbow. In dogs older than 5 months of age, radiographs of the joint may show a radiolucent line in the anconeal process (ie, UAP; Figure 3), an articular defect in the medial aspect of the humeral condyle (ie, OC, OCD; Figure 4), sclerosis and blunting of the medial coronoid process (ie, MCD), degenerative changes, or joint incongruency.
MCD (with or without fragment) is the most common among these conditions. Advanced imaging techniques (eg, CT) help in visualization of the coronoid process, which may appear fragmented or sclerotic (Figure 5), be associated with osteophytosis, or have radial incisure irregularities.

Figure 3.
Mediolateral radiograph of the elbow in a 7-month-old German shepherd dog with joint effusion and pain of the elbow. A radiolucent line (arrow) can be observed between the anconeal process and proximal ulna, consistent with UAP.
Initially, nonsurgical treatment of the primary condition (eg, weight management, analgesics, joint supplements, exercise modification, physiotherapy) can be instituted. When indicated, arthroscopy with fragment removal and abnormal cartilage debridement is recommended for fragmentation of the coronoid process in clinically affected animals that do not respond to conservative management (Figure 6).
The response to surgical treatment can vary, and development of OA continues in the joint despite treatment. Other surgical options include subtotal coronoid ostectomy (SCO), sliding humeral osteotomy (SHO), proximal abducting ulnar osteotomy (PAUL), or biceps ulnar release procedure (BURP).
Management of joints with significant OA can also be nonsurgical (eg, weight loss, analgesics, joint supplements, exercise modification, physiotherapy) or surgical (eg, canine unicompartmental elbow [CUE] replacement, total elbow replacement). Removal of the cartilage flap with debridement of the subchondral bone arthroscopically is also recommended for OCD lesions. The UAP can be reattached and compressed to the proximal ulna via a lag screw if degeneration of the fragment is not advanced. If fragment degeneration is advanced, however, removal by arthrotomy is recommended. If joint incongruency is evident, proximal ulnar osteotomy/ostectomy may be performed to improve congruency.
3. Medial patellar luxation
With this developmental disease, coxa vara (ie, decreased angle of inclination of the femoral head) and diminished anteversion angle (ie, less cranially oriented) of the femoral head result in medial displacement of the quadriceps mechanism. This muscular displacement results in abnormal forces that predispose the patella to luxate medially (Figure 7). MPL (95% of cases) is more common than lateral patellar luxation (LPL; 5% of cases); MPL especially affects small-breed dogs, although large-breed dogs may also be affected.1 Patellar luxation can be graded from 1 to 4, depending on the frequency of luxation and difficulty of manual reduction.
Related Article: Medial Patellar Luxation
Grade 1 MPL is usually nonclinical and generally does not require surgical treatment, while grade 4 always requires surgical repositioning of the patella in the groove. The decision to pursue surgical treatment in dogs with grades 2 and 3 MPL depends on the severity of clinical signs. Surgical treatment includes various techniques (eg, trochleoplasty, en block recession trochleoplasty, wedge recession trochleoplasty, abrasion trochleoplasty, trochlear chondroplasty [Figure 8], tibial tuberosity transposition [TTT], antirotational sutures, joint capsule imbrication or release).

Figure 7.
Ventrodorsal radiograph of the pelvis and hindlimbs in a 12-month-old Cavalier King Charles spaniel with MPL of the right stifle. Internal rotation of the tibial tuberosity is evident.
Intraoperative exploration of the trochlear depth and quadriceps mechanism alignment determine the surgical technique to perform. However, osseous techniques (ie, TTT, trochleoplasties) have been associated with lower risk for patellar reluxation (Figure 9) and higher success rates than soft tissue techniques alone (ie, imbrication, release, and antirotational sutures).2
4. Shoulder OCD
Abnormal endochondral ossification of the articular cartilage leads to an area of increased thickness (ie, OC) that eventually breaks and forms a cartilaginous flap (ie, OCD). Multiple factors play a role in this pathology, including genetics and environmental factors (ie, high protein diets, calories, calcium).
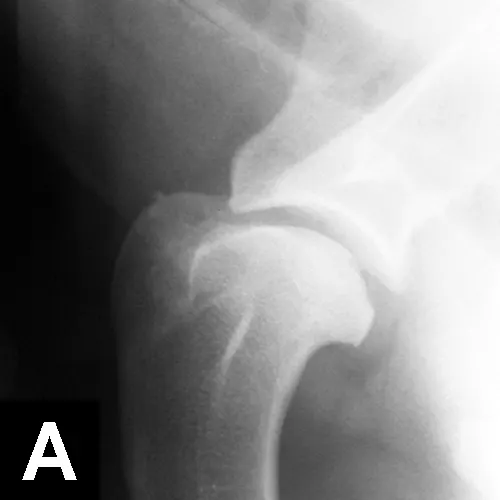
Figure 10A.
Mediolateral radiographs of the shoulder in an 8-month-old German short-haired pointer with left forelimb lameness. Flattening of the humeral head with sclerosis of the underlying subchondral bone suggests OCD.
Large-breed dogs are most commonly affected, usually presenting with unilateral or bilateral forelimb lameness between 4 and 8 months of age. Muscle atrophy and pain during shoulder manipulation may be found in affected dogs. Diagnosis is based on clinical signs and radiographic visualization of flattening of the caudal aspect of the humeral head (Figure 10A). Positive-contrast arthrography may help in the diagnosis when radiographs are unclear (Figure 10B). Advanced imaging (eg, CT, MRI) can be helpful in elusive cases.Surgical or arthroscopic removal of the cartilage flap with debridement of the subchondral bone often leads to an excellent prognosis (Figure 10C).
Figure 11. Mediolateral radiograph of the antebrachium in a 6-month-old German shepherd dog with shifting lameness. Patchy increased opacity within the medullary cavity of the ulnar diaphysis and proximal metaphysis suggest panosteitis.

Related Article: Osteochondritis Dissecans of the Shoulder
5. Panosteitis
Panosteitis is a self-limiting inflammation of bone marrow in long bones. Large-breed dogs (particularly the German shepherd dog) are most commonly affected, although smaller breeds can also be affected. Males seem to be affected more frequently; most patients are between 5 and 12 months of age (range, 2 months–5 years).3 Affected dogs usually present with shifting lameness, which may range from mild lameness to inability to walk. Clinical signs include pain on palpation of the affected long bones, especially in the forelimb. Radiographic findings vary, depending on disease stage, but increased medullary densities at the level of the nutrient foramen and periosteal reaction are common (Figure 11). Clinical signs typically resolve by 18 to 20 months of age. Treatment does not appear to influence the outcome and consists of supportive measures (eg, rest, analgesics).