Top 5 Causes of Nonblanching Skin Lesions
Darren Berger, DVM, DACVD, Iowa State University
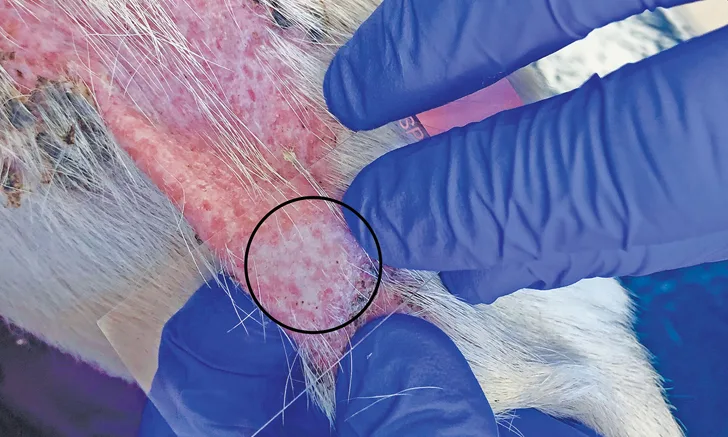
Positive diascopy result indicated by the well-demarcated area of blanching (circle) in a patient with erythemic plaque secondary to calcinosis cutis
Patchy, erythemic-to-violaceous skin lesions are commonly encountered in veterinary patients. Diascopy is a quick and efficient test that can help determine whether lesions are the result of vasodilation secondary to inflammation or associated with a more clinically concerning process.
In diascopy, a clear glass slide is placed over an erythemic lesion and pressure is applied while care is taken not to injure the patient or break the slide. A positive diascopy result occurs when the applied pressure results in blanching of the skin (Figure 1), as seen in cases of erythema secondary to simple vascular vasodilation. A negative diascopy result occurs when the applied pressure does not result in skin blanching.
Following are 5 of the author’s more common causes of skin lesions that will not blanch.
1. Cutaneous Adverse Drug Reactions
Cutaneous adverse drug reactions can result from administration of medications. Commonly implicated substances include antimicrobials (eg, β lactams, sulfonamides), NSAIDs (Figure 2), and antiparasitics.1 Drug reactions can appear as any dermatologic condition, with lesions being focal-to-generalized. Typical lesion patterns include urticarial angioedema, maculopapular eruptions, vesiculobullous reactions, nodules, exfoliative erythroderma, purpuric lesions, pemphigus-like lesions, erythema multiforme, vasculitis, and toxic epidermal necrolysis.2 Clinical signs typically occur within 1 to 3 weeks of initiating administration of the offending drug but can also arise more quickly (eg, within days), after a single treatment, after years of use, or days after the medication has been stopped.2
Because cutaneous adverse drug reactions can overlap with many dermatologic conditions, diagnosis is primarily based on suspicion from patient history, physical examination, and the elimination of other differentials. No particular clinical pathology or histopathology results can specifically indicate a cutaneous adverse drug reaction. Definitive diagnosis typically requires drug provocation testing (ie, readministration of the suspected offending agent), but this is considered unethical in many cases due to the severity and potentially fatal nature of disease.
Treatment consists of supportive care, immunomodulatory therapy (eg, glucocorticoids, cyclosporine), discontinuation of all possible offending drugs or nutraceuticals, and avoidance of chemically related drugs. In rare refractory cases, other immunomodulatory therapies such as intravenous immunoglobulin may be effective.2

Multiple erythemic, erosive nodules along the rostral muzzle of a patient secondary to NSAID administration
2. Petechiae & Ecchymoses from Coagulation Disturbances
Petechiae and ecchymoses are erythemic-to-violaceus macular discolorations of the skin or mucosal surface. They occur secondary to blood vessel bleeding that may coalesce to affect a large surface area (Figure 3). These lesions are often seen with quantitative and/or qualitative hemostatic disorders, the most common of which is thrombocytopenia.3
Diagnosis of these conditions involves a thorough patient history, CBC with blood smear review, coagulation profile, platelet function tests, bone marrow aspiration, infectious disease testing, and, if necessary, genetic testing.3
Treatment is highly variable and depends on the underlying disorder and severity. Skin biopsy acquisition is contraindicated in cases of suspected petechiae and/or ecchymoses.

Ecchymotic lesions along the ventral abdomen and thorax in a patient with immune-mediated thrombocytopenia. Photo courtesy of Dr. Ellen Heinrich, Iowa State University
3. Epitheliotropic T-Cell Lymphoma
Epitheliotropic T-cell lymphoma is an uncommon disease of older animals in which neoplastic cells infiltrate the epidermal structures. The exact etiology is unknown, but an association with atopy has been proposed.4
Epitheliotropic T-cell lymphoma has various clinical presentations, including generalized exfoliative erythroderma (Figure 4), erosive-to-ulcerative plaque, cutaneous nodules, mucocutaneous lesions, and/or disease confined to the oral mucosa. Pruritus is common and, in the author’s experience, often leads to a misdiagnosis of allergic hypersensitivity. Patients with disease confined to the mucocutaneous junctions or oral mucosa are commonly misdiagnosed with autoimmune disease.
Diagnosis is confirmed via biopsy with histopathology, which demonstrates the characteristic epitheliotropism of the neoplastic cells and differentiates this condition from nonepitheliotropic cutaneous lymphoma. Prognosis is poor, with a reported median survival time of 6 months following diagnosis.5
Several therapeutic protocols have been proposed in the treatment of epitheliotropic T-cell lymphoma in dogs, but oral administration of lomustine is most commonly used.6

Erythrodermic plaque in an English bulldog with epitheliotropic T-cell lymphoma
4. Cutaneous Vasculitis
Vasculitis is an uncommon disorder characterized by an aberrant immune response that results in blood vessel damage. It is considered to be a reaction pattern with numerous potential triggers. Possible inciting causes include medications, vaccinations, infectious disease, parasites, adverse reactions to food, familial disease, metabolic derangements, neoplasia, and idiopathic forms. Cutaneous lesions are usually well-demarcated and consist of edema, purpura, alopecia, erosions, focal punctate ulcers, crusting, necrosis, and/or eschar formation (Figure 5). Although lesions may occur anywhere, the extremities, tips of the ears, oral mucosa, and tail are more commonly affected.7 Patients may also display systemic signs, which should correlate with disease severity.
Diagnosis is based on clinical suspicion and compatible skin biopsy results. Newer lesions show the best diagnostic yield of biopsy specimens, as chronic lesions may only reveal ischemic changes.7 Following a confirmed diagnosis, the patient should be evaluated for specific etiologies via blood work, urinalysis, tick-borne disease testing, imaging studies, coagulation profiles, and immunologic assays. In cases in which diagnostic testing fails to identify a probable cause, a diet elimination trial should be considered, as a retrospective study previously identified food allergy as the underlying etiology in a subset of cutaneous vasculitis cases.8
Therapy should focus on removal or treatment of the underlying cause and immunomodulation. Prognosis is highly variable and dependent on the underlying cause, lesion extent, and degree of systemic involvement.

Well-demarcated, erythemic, alopecic patch with multiple punctate ulcerations along the caudal lateral pelvic region of a mastiff with acute onset cutaneous vasculitis
5. Erythema Multiforme
Erythema multiforme is an uncommon condition that, in veterinary medicine, is inappropriately synonymous with a drug reaction.9 Similar to vasculitis, numerous potential inciting causes (eg, medications, cutaneous adverse food reactions, bacterial infection, viral infection, vaccinations, neoplasia, idiopathic forms) have been associated with erythema multiforme. Disease varies from mild to severe based on systemic clinical signs. Common lesions include erythematous macules, papules, and plaque with central clearing that creates serpiginous-to-annular areas that eventually become necrotic, crusted, or hyperpigmented (Figure 6).9 Lesions commonly involve the ventrum, concave aspects of the ears, footpads, and/or mucocutaneous junctions.
Diagnosis should be made via biopsy with histopathology, which should demonstrate indicative microscopic changes.9 After diagnosis is confirmed, blood work, urinalysis, infectious disease testing, and advanced imaging should be pursued to evaluate for underlying disease.
Initial treatment should consist of removing potential offending agents (eg, discontinuing medications, treating infections, avoiding suspect dietary antigens) and providing supportive care.9 Mild cases may resolve spontaneously, but immunosuppressive therapy is required in most cases and may be needed lifelong in chronic relapsing or idiopathic cases.9 Prognosis ranges from good to poor and is mostly dependent on the identification of the underlying cause and severity of systemic disease.

Well-demarcated, erythemic, erosive, and crusted lesions along the ventral abdomen of a patient with erythema multiforme