Top 5 Canine Ophthalmologic Emergencies
DJ Haeussler, Jr, DVM, MS, DACVO, The Animal Eye Institute, Cincinnati, Ohio
Prompt, accurate recognition and treatment (or referral) of canine ophthalmologic emergencies are of paramount importance. Early and correct identification and treatment of an abnormality could mean the difference between a patient losing its vision or the clinician being able to salvage vision and, in many instances, the globe itself. This article discusses 5 of the top canine ophthalmologic emergencies seen in general practice.
1. Descemetocele & Corneal Rupture
A descemetocele is an extremely deep corneal ulcer in which the corneal epithelium and stroma have been completely eroded, leaving only Descemet’s membrane and corneal endothelium (Figure 1).1 A descemetocele typically occurs after a corneal ulcer has become infected with a corneal infiltrate (eg, bacterium, fungus), which results in stromal erosion extending deep into Descemet’s membrane. When Descemet’s membrane (usually 3-12 μm thick1) fractures, a corneal rupture can occur. Diagnostic testing should include menace response, dazzle reflex, pupillary light reflexes (direct and consensual), fluorescein staining, and Schirmer tear testing. In addition, corneal culture and susceptibility testing should be conducted. Tonometry is typically avoided because of the potential for corneal rupture.

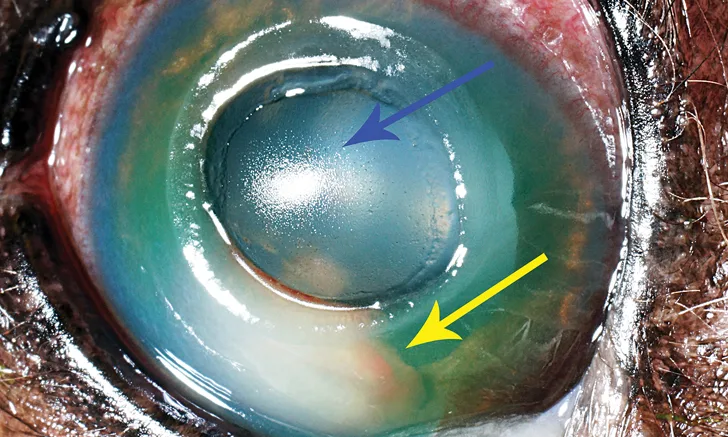
Large central corneal descemetocele (blue arrow) with hypopyon (yellow arrow). Corneal vascularization, edema, and conjunctival hyperemia are also present.
A full-thickness corneal rupture can result in aqueous humor loss and, occasionally, iris prolapse, hyphema, corneal fibrin clot, and/or decreased depth of the anterior chamber (Figure 2).1 If the rupture is not addressed quickly, bacterial contamination of the anterior chamber can occur, resulting in endophthalmitis, which carries a poor prognosis for vision and saving the globe.1,2 In affected patients, diagnostic testing should consist of menace response, dazzle reflex, pupillary light reflexes (direct and consensual), and fluorescein staining. Schirmer tear testing is typically avoided, as the test strip can dislodge a fibrin clot. Tonometry is avoided because of the potential risk for re-injuring a sealed corneal rupture; however, cytology and corneal culture and susceptibility testing should be conducted.

Central corneal rupture with fibrin clot (blue arrow), corneal edema, iris prolapse, hyphema, corneal vascularization, edema, and conjunctival hyperemia
In general, an Elizabethan collar is recommended as a preventive measure in patients with corneal rupture or rerupture. Topical fluoroquinolone treatment can also be initiated. In addition, a topical mydriatic such as atropine should be administered q24h to facilitate mydriasis and improve patient comfort. In the case of corneal rupture, amoxicillin–clavulanic acid (13.75 mg/kg PO q12h3) is advantageous because it can reach therapeutic levels in the anterior chamber.3 Carprofen (2.2 mg/kg PO q12h4) is also indicated as an anti-inflammatory. In addition, immediate referral to a board-certified ophthalmologist should be recommended, along with consideration of options such as conjunctival pedicle grafting, corneoconjunctival transposition, corneal transplantation, or corneal collagen extracellular matrix grafting.1
2. Proptosis
Proptosis is forward displacement of the globe with simultaneous entrapment of the eyelids behind the equator of the globe (Figure 3).5,6 The condition occurs more often in brachycephalic breeds6,7; of note, considerably greater trauma is necessary to cause proptosis in dolichocephalic breeds.


Proptosis showing the eyelids trapped behind the equator of the globe. (A) A miotic pupil, common following proptosis, subconjunctival hemorrhages (blue arrow), and (B) hyperemia are also evident.
A traumatic incident that can cause blindness, desiccation of the cornea, and corneal ulceration, proptosis requires immediate attention,6 including initiation of pain medications (eg, carprofen [2.2 mg/kg PO q12h4], tramadol [2-4 mg/kg PO q8h]).
Globes should be salvaged when possible. If more than 2 extraocular muscles are avulsed, the globe should usually be removed, as proper innervation and vascular supply have been compromised. Often, patients with scleral ruptures are candidates for enucleation when the globe develops hyphema, prognosis for return to vision is grave, or the eye remains painful.6,8 Furthermore, in the author’s experience, small scleral tears may result in hyphema, requiring globe replacement; these patients will require acute pain medication for an extended period (eg, 4-6 weeks), and although the globe may become phthisical, owners often are pleased with the cosmetic result.9
Diagnostic testing (eg, menace response, dazzle reflex, pupillary light reflexes [direct and consensual], Schirmer tear testing, tonometry, fluorescein staining) is important in deciding whether the globe can be salvaged or should be removed. Patients have a grave prognosis for return of vision if they lack dazzle and consensual pupillary light reflexes and have intraocular pressures (IOPs) >25 mm Hg (ie, glaucoma).
If the owner is reluctant to make a decision after all options have been discussed, the globe can be replaced and secured with a temporary tarsorrhaphy, then removed later if necessary. This temporary procedure should be performed with the patient under general anesthesia, using stents (eg, IV tubing) and 4-0 to 2-0 monofilament nonabsorbable suture<sup.6sup>
Approximately 20% of dogs with proptosis will regain or retain vision in the proptosed eye.5-7
3. Corneal Laceration
A full-thickness corneal laceration can be devastating. Reported causes have included laceration by cat claw,9 along with contact with a stick or other vegetative foreign body. Potential sequelae can include anterior chamber collapse, hyphema, hypopyon, iris prolapse, cataract, uveitis, and endophthalmitis (Figure 4).10

This cornea was lacerated horizontally (via cat claw) in the dorsal aspect (blue arrow). Iris prolapse, dyscoria resulting from the laceration, fibrin, and hyphema (yellow arrow) are present.
A menace response, dazzle reflex, pupillary light reflexes (direct and consensual), fluorescein staining, and Seidel test should be performed. Referral to an ophthalmologist is critical for reinflation of the anterior chamber, closure of the laceration, and examination of the lens for lens capsule rupture and cataract formation.11 Surgery should be performed with proper microsurgical instrumentation, magnification, and expertise (Figure 5). If a cataract is present from the laceration, referral for phacoemulsification should be considered at the time of corneal laceration repair.

Postoperative appearance of the same eye shown in after repair of the corneal laceration; a bootlace pattern of 8-0 polyglactin 910 suture was used to close the wound (blue arrow). The bubbles visible in the anterior chamber are of minimal significance, as they will resolve in <12 hours and cause no consequence to the eye.
4. Anterior Lens Luxation
Anterior lens luxation is a result of the crystalline lens moving from the patellar fossa in front of the iris and into the anterior chamber (Figure 6).12 Causes can vary and be primary, secondary, congenital, or traumatic.12 Primary lens luxation generally occurs in terrier breeds, although the shar-pei is also overrepresented.12 Secondary lens luxation may be associated with buphthalmos of the globe, which is attributable to glaucoma or chronic lens-induced uveitis secondary to cataract formation.12 Traumatic lens luxation has typically been implicated in cases of blunt trauma and, in the author’s experience, most frequently occurs in animals hit by an automobile.9 Unresolved anterior lens luxation can lead to rapid increase in IOP, which can result in irreversible blindness and pain.12 In addition, corneal edema can develop when the lens contacts the endothelium.12 Finally, the constant intraocular movement of the lens can cause secondary glaucoma and microtrauma to other intraocular structures.12

Visualization of the equator of the lens (blue arrow), a hallmark feature of an anterior lens luxation, as well as posterior displacement of the dyscoric pupil are key in detecting anterior lens luxation.
When evaluating patients with anterior lens luxation, it is important to perform a menace response, dazzle reflex test, pupillary light reflexes (direct and consensual) test, Schirmer tear test, and tonometry. In patients with glaucoma, topical carbonic anhydrase inhibitors and β-blockers (eg, dorzolamide–timolol drops q8h) should be administered, whereas miotics (eg, pilocarpine, latanoprost) are contraindicated because they can severely increase IOP. Referral is recommended for evaluation of anterior lens luxation and to discuss such options as lensectomy.
5. Acute Glaucoma
Primary acute glaucoma involves acute increase in intraocular pressure that can result in vision loss.13 Primary acute glaucoma typically occurs in dogs affected by primary glaucoma. Clinical signs include IOP >25 mm Hg, episcleral injection, corneal edema, loss of menace response, potential loss of dazzle reflex, and mydriatic pupil (Figure 7).13 Initial diagnostics should examine menace response, dazzle reflex, pupillary light reflexes (direct and consensual), and tonometry.

Acute glaucoma in a Great Dane. Note the severe corneal edema, conjunctival hyperemia, and mydriasis. In addition to being a defining clinical sign of glaucoma, the presence of mydriasis suggests clinical evidence of the condition, which can be especially helpful when tonometry is not available.
Therapeutics should not only lower but also maintain lowered IOP, along with vision and comfort. Mannitol (20%) can be administered at 1-2 g/kg IV over 30 minutes.13-15 Topical dorzolamide–timolol inhibitors (eg, dorzolamide q8h) as well as prostaglandin analogues (eg, latanoprost q12h) may also be indicated to lower IOP. These patients can be managed in-house until IOP is within normal limits. Both IOP and vision response should be re-examined within a week. In addition, adjunctive analgesics (eg, carprofen 2.2 mg/kg PO q12h,4 tramadol 2-4 mg/kg PO q8h16) may be necessary. Consultation with an ophthalmologist is helpful to determine a preferred course of therapy and medical and surgical options.
Global Commentary
Top 5 Canine Ophthalmic Emergencies: A Global Perspective