Tooth Resorption in Dogs
Jan Bellows, DVM, FAVD, DAVDC, DABVP, All Pets Dental, Weston, Florida
Tooth resorption is common in cats and, because of increased use of intraoral radiology, is clinically emerging in dogs. Recognition and treatment of tooth resorption in dogs is essential. Anatomically, the buccal surfaces of the mandibular premolars are most commonly affected. In some cases, the overlying gingiva appears hyperplastic and inflamed, but in others there is no visible abnormality to indicate pathology.
Tooth resorption can be classified by the extent of lesion progression, radiographic appearance, anatomic location, and cause. For treatment planning, it is important to know if the resorption is internal or external and, if external, whether the lesion has extended to the oral cavity.
1. Classification by Extent
Stage 1: Minimal hard tissue (cementum or cementum and enamel) loss.
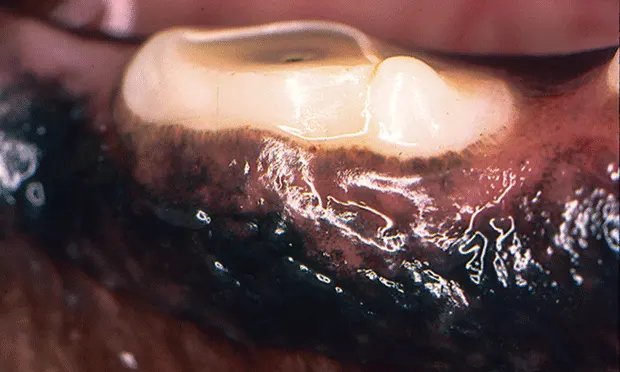
Stage 2: Moderate hard tissue loss (with loss of dentin not extending into pulp cavity) (See Figures 1A, 1B, and 1C).
Stage 3: Deep hard tissue loss (extending into pulp cavity). Most of the tooth retains integrity.
Stage 4: Extensive hard tissue loss. Most of the tooth loses integrity. In stage 4A (See Figure 1D), the crown and root are equally affected; in stage 4B (See Figure 1E), the crown is more severely affected than the root; in stage 4C (See Figure 1F), the root is more severely affected than the crown.
Stage 5: Remnants of hard tissue are visible only as irregular radiopacities, and gingival covering is complete.

Clinical appearance of tooth resorption extending into the oral cavity.

Intraoral radiograph revealing extent of external tooth resorption.

Extracted tooth.

Mandibular second molar affected by stage 4A tooth resorption.

Mandibular first molar affected by stage 4B tooth resorption.

Mandibular fourth premolar affected by stage 4C tooth resorption.
2. Classification by Radiographic Appearance
Type 1: There is alveolar bone loss adjacent to well-defined areas of tooth resorption. The lesion appears radiographically discrete and unaffected areas of the root appear normal. Normal periodontal ligament space is maintained at other areas of the tooth (See Figure 2A). If the lesion extends into the oral cavity, the tooth should be extracted.
Type 2: There is loss of periodontal ligament space and lamina dura from fusion of tooth root and alveolar bone (ie, dentoalveolar ankylosis). The resorbing tooth structure may appear less radiopaque than the unaffected tooth (ie, replacement resorption). If the lesion extends into the oral cavity (See Figure 2B), using a high-speed water-cooled handpiece the crown can be reduced in height below the gingiva before closure.
Type 3: Features of both type 1 and 2 are present (See Figure 2C). If the lesion extends into the oral cavity, the tooth should be extracted.

Type 1 resorption. Arrows point to distal root resorption lacuna with discernible periodontal ligament space.

Type 2 resorption in the deciduous mandibular fourth premolar with exposure to oral cavity; extraction is indicated.

Type 3 resorption of the mandibular fourth premolar. The distal root shows decreased radiopacity (type 2) while the mesial root opacity appears normal.
3. Classification by Physiological Process: Internal Tooth Resorption
Internal surface resorption (See Figure 3A), is characterized by an oval-shaped enlargement in the apical third of the root canal, interpreted as a sign of active revascularization and considered a self-limiting process that results from mild traumatic injuries.
Internal replacement resorption is characterized by an irregular enlargement with a tunnel-like appearance adjacent to the resorbed root canal. The lesion is typically located on the coronal fragment of root fractures. It is not considered a progressive condition, and no specific treatment is indicated.
Internal inflammatory resorption (See Figures 3B and 3C) ischaracterized by an oval-shaped enlargement typically found in the coronal third of the tooth and results from active inflammation secondary to trauma. Treatment options are either extraction or root canal therapy, if the lesion has not progressed to perforation of the root.

Mandibular first molar distal root with evidence of internal resorption and periodontal disease (arrows).

Pulp exposure secondary to chronic tennis ball abrasion.

Internal resorption of the mesial and distal roots.
Classification by Cause
External inflammatory resorption of cementum and dentin is caused by inflammation in the adjacent periodontal ligament. Two common sources are inflammation from marginal periodontitis and apical or radicular periodontitis from inflammatory mediators produced by endodontic pathology that exit the tooth through apical or lateral canals. Bone resorption often occurs adjacent to root resorption. Resorption may also be caused by pressure on the periodontal ligament and cementum from an expansile mass or cyst or impacted tooth.
4. Classification by Physiological Process: External Tooth Resorption
External surface resorption affects the cementum and dentin and is not always visible on radiographs. Lesions are typically located laterally along root margins. The periodontal ligament space and lamina dura are not affected. No clinical signs are associated.
External replacement resorption (See Figure 4) appears as decreased periodontal ligament space with partial replacement of root tissues by the surrounding alveolar bone. It is associated with injuries that lead to necrosis of the periodontal ligament fibers and is thought to be progressive.
External inflammatory resorption occurs secondary to local inflammatory conditions (eg, endodontic or periodontal disease). Endodontically compromised teeth are considered to have some external inflammatory resorption. Treatment is targeted at the underlying disease process.

Maxillary third premolar affected by external replacement resorption.
5. Classification by Anatomic Location
In external resorption, tooth roots resorb from the outside toward the inside secondary to periodontal disorders or because of endodontic pathology, with inflammatory mediators exiting apical foramina or lateral canals to affect the periodontium. In less common internal resorption, part of the root resorbs from the inside. Internal root resorption is related to granulomatous pulpitis and can occur anywhere in the pulp cavity.
Radiographically, when external resorption is apically located, the apex may appear shortened, blunted, square, ragged, or irregular. Internal resorption is radiographically diagnosed as increased radiolucent area(s) within the pulp cavity.