How to Perform a Temporary Tracheostomy in Dogs
Alexandre Caron, DVM, MRCVS, DECVS, CHV Atlantia, Nantes, Frances
Indications
Temporary tracheostomy, which creates a bypass of the upper airway, is indicated for any medical condition that results in upper airway obstruction (eg, trauma,1,2 neoplasia,3 functional or conformational conditions as in brachycephalic patients or dogs with laryngeal paralysis).1,4-7 Temporary tracheostomy is rarely performed in a real emergency situation and endotracheal intubation will most often still be possible. Nevertheless, in cases where intubation is impossible, such as respiratory distress with complete pharyngeal obstruction that cannot be relieved (eg, phrayngeal neoplasia, pharyngeal foreign body) or locked-jaw syndrome, emergency tracheostomy can be required.
For some elective surgeries, the endotracheal tube may be in the surgeons field of work. Therefore, placement of a temporary tracheostomy tube for gas anesthesia maintenance can be performed to avoid presence of a tube in the surgical field. This would be the case for oral cavity surgeries requiring correct assessment of dental occlusion (eg, mandibular fracture repair).
Tube Selection
A tracheostomy tube should measure a length of approximately 6 or 7 tracheal rings and a maximum diameter of 50% of the diameter of the tracheal lumen at the level it is placed. Material should be autoclavable and non-irritating to the tracheal mucosa (eg, silicone, nylon, silver).7-10
Tracheostomy tubes come in different sizes, have single- or double- lumens, and are cuffed or cuffless. Single-lumen tubes must be removed and replaced entirely each time they need to be cleaned. With double-lumen tubes, the inner cannula alone can be removed for cleaning; this makes the repositioning procedure easier.10 However, because a larger outer diameter is required to achieve the same inner diameter as a single-lumen tube, it is less useful in cats and small dogs. Mucus may also accumulate at the extremity of the outer cannula, which necessitates its removal for cleaning.8
Cuffed tubes should be used only when mechanical ventilation is required.10 A high-volume, low-pressure cuff is preferable to reduce risk for tracheal pressure necrosis or stenosis.6-8
Related Article: The Art of Triage
Complications
Temporary tracheostomy is associated with a high complication rate.4,5 A recent study, focused on complications following tracheostomy tube placement (n = 42), reported an 86% (n = 36) complication rate with 10% (n = 4) of all dogs euthanized following occurrence of complications.5 Underlying disease was a major factor in survival with only 60% survival (n = 25) reported in this study, despite 81% of successful tube management in a majority of cases. Similar findings have been reported for cats.
After placement of a tracheostomy tube, the patient should be monitored closely for potentially life-threatening complications. Tube dislodgement affects 13% to 35% of patients that undergo tracheostomy, and obstruction affects 18% to 26%.5
Other possible complications include aspiration pneumonia, tracheal infection or necrosis, tracheal stenosis, pneumomediastinum, pneumothorax, and subcutaneous emphysema.5 During routine care, gagging, vomiting, and vagal reflex may also occur.8
Tracheal stenosis, the most significant long-term complication, will occur to some degree in all cases (25% loss of luminal area 2 months postremoval) but should not be clinically significant if proper technique has been employed.10 It can be circumferential if the tube was too large or the cuff overinflated. The type of tracheal incision (transverse vs others) does not seem to be correlated with risk for complications.6,8
Related Article: Laryngeal Paralysis Diagnosis
Routine Care
Depending on patient and condition, specific care to the tracheostomy tube may vary, especially in terms of frequency. Tube cleaning is required at least twice daily, with most patients requiring cleaning 4 times a day or more.6
Cats tend to require more frequent maintenance because of thicker mucus often reported in association with smaller tracheal diameter leading to quicker luminal obstruction.4,8
Maintenance involves removing and cleaning the tube, suctioning accumulated secretions in the tracheal lumen, cleaning the stoma, and maintaining appropriate humidity in the trachea and lower airways.8Airways should be kept humidified by nebulization or instillation of sterile saline into the tracheostomy tube (0.2 mL/kg). This should be performed hourly8and can help in suctioning secretions if performed a few minutes earlier.9
Maintenance care should include preoxygenation to limit risk for hypoxemia. Electrocardiographic monitoring is advised because vagal stimulation is reported in 10% of patients following tracheal stimulation during tube maintenance.5,6,8
The tracheostomy tube (or the inner cannula for double-lumen tube) should be removed, cleaned with sterile saline, and soaked in 2% chlorhexidine solution when required.6
While the tracheostomy tube is soaking, suctioning of the trachea is performed with a small sterile suction catheter; soft urinary catheters are often used. Once the catheter is in place in the lumen, suction can be initiated. Suction should not last longer than 10 to 12 seconds and can be repeated if necessary.6,8This procedure can also be performed through the tube. It is important to carefully monitor the patients response to this procedure.
The stoma should be inspected at least once a day for signs of infection and gently cleaned with sterile saline or dilute antiseptic solution.
The tracheostomy tube can be soaked in antiseptic solution, rinsed with sterile saline, and replaced. In case of accumulation of bronchial secretions, coupage can help clear lower airways.8
Removal
Removal of the tracheostomy tube can be performed as soon as the underlying condition does not require its use; this may be after hours or weeks. Some authors suggest occluding the tube before removal to assess the patients ability to breathe correctly. Occluding the tube usually does not allow for proper evaluation of upper airway patency because the presence of the tube itself in the tracheal lumen will lead to some respiratory distress, especially when large (partial obstruction) or cuffed tubes (partial to complete obstruction) have been placed.
The stoma will be left to heal by second intention, which should occur within 7-10 days.6,7,9,10
Related Article: Emergency Stabilization for Transport
Step-by-Step: Transverse Temporary Tracheostomy
Note: All patients have to be under general anesthesia for tracheostomy tube placement. An adequate pain-management plan, including opioids, should be in place.
What You Will Need
Self-retaining retractor (Gelpi retractors pictured)
Scalpel blade handle and scalpel blades (size depending on surgeons preference; pictured are size #10 and #11 scalpel blades for cutaneous and tracheal incisions, respectively)
Mayo scissors
Metzenbaum scissors
2 hemostatic forceps
Sterile swabs
Nonabsorbable large diameter monofilament suture (3.5 metric polyamide pictured)
Needle holders
Tracheostomy tube and securing string
Right-angle anaesthesia tubing connector
Surgical drape
Step 1: Approach
A ventral midline cutaneous 4-cm incision is made from slightly caudal to the cricoid cartilage (Figure 1A, curved lines) with a #10 scalpel blade (Figure 1B). After blunt subcutaneous dissection, the midline raphe between paired sternohyoideus muscles is bluntly dissected (Figures 1C and 1D). Sternohyoideus muscles are then retracted laterally with the use of self-retaining retractors (eg, Gelpi), exposing the ventral portion of the cranial aspect of the cervical part of the trachea (Figure 1E).

FIGURE 1A
A ventral midline cutaneous 4-cm incision is made from slightly caudal to the cricoid cartilage (curved lines).
Step 2: Loops of Suture Placement
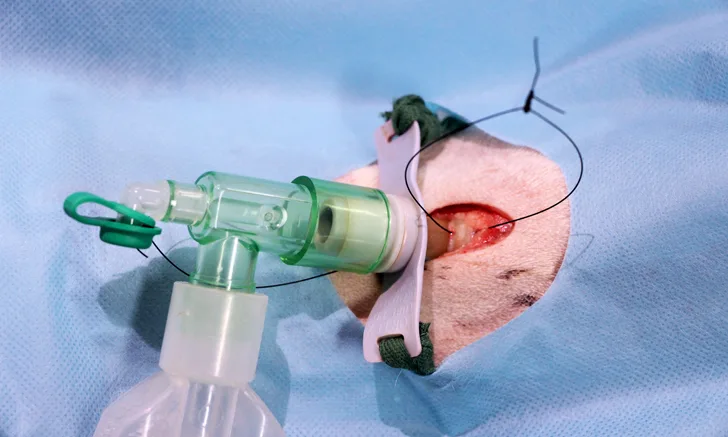
Tracheal rings 3, 4, and 5 are identified, and 1 of the 2 spaces between those rings is chosen for temporary tracheostomy tube placement. A loop of nonabsorbable suture of large diameter (3.5 metric polyamide is used here) is placed around the tracheal rings cranial and caudal to the chosen site. Loops should be wide and appropriately tied to remain in place as long as the tube is (Figure 2).


Step 3: Tracheal Incision
Gentle traction is applied by the assistant on both suture loops while a transverse incision is made with a #11 scalpel blade in the annular ligament between the 2 retracted tracheal rings (Figure 3). The incision should not be wider than 50% of the circumference of the trachea at this level. Care should be taken not to damage the underlying endotracheal tube (and its cuff).


Step 4: Tracheostomy Tube Placement
Gentle traction is maintained on the 2 suture loops. In this case, an endotracheal tube has been placed and has to be identified (Figure 4A) before progressive removal by the anesthetist (Figures 4B and 4C). This procedure should be performed under direct visual control of the primary surgeon. Once the endotracheal tube has been withdrawn with the tip just cranial to the tracheostomy site, the tracheostomy tube can be gently inserted into the trachea (Figures 4D and 4E). If blood or mucus has accumulated in the lumen, it can be gently suctioned. Tension on suture loops can be released.

FIGURE 4A
Gentle traction is maintained on the 2 suture loops. In this case, an endotracheal tube has been placed and has to be identified.
Step 5: Anesthesia Gas Inflow Maintenance
Once the tracheostomy tube has been introduced, the anesthetist can remove the endotracheal tube and disconnect the gas flow tubing system. The surgeon, assistant surgeon, or anesthetist should take the sterile right-angle connector and plug it into the gas flow tubing system. Gas inflow can then be restored by connecting the right angle connector directly to the tracheostomy tube.
Author Insight
Because the tube is not secured in position at this stage, it is important not to dislodge it by inadvertently pulling on the gas flow tubing system. Therefore, the assistant should hold it in place and/or the anesthetist can hold the gas flow tubing system under the surgical drapes (Figure 5).

Step 6: Securing the Tracheostomy Tube
Two strings are attached on each side of the tracheostomy tube and passed through the surgical draping window toward the dorsal aspect of the neck (Figure 6). The anesthetist or the assistant takes the 2 strings and ties them together dorsally with just enough tension to maintain it in place.

Step 7: Closure
No closure is usually required. Muscular, subcutaneous, and cutaneous tissues can be left to heal by second intention. It is often necessary to place a few cutaneous suture(s) caudal to the tracheostomy site to appose skin adjacent to the stoma (Figure 7A).


Author Insight
When the sterile procedure is finished, a band of white tape is placed at the end of each suture loop. Both loops should be identified (pictured, up for the cranial and down for the caudal) to clearly indicate which direction it should be pulled to open the tracheostomy wound for removal or replacement of the tube (Figure 7B). Keep in mind that asurgeon will not always be available when inadvertent tube removal occurs, and the entire team should be able to quickly replace a tracheostomy tube in case of emergency.
Editor’s note: This article was originally published in April 2016 as “Temporary Tracheostomy in Dogs.”