Surgical Treatment of Periapical Mandibular Abscess in Rabbits
Vittorio Capello, DVM, Clinica Veterinaria S Siro, Clinica Veterinaria Gran Sasso, Milan, Italy
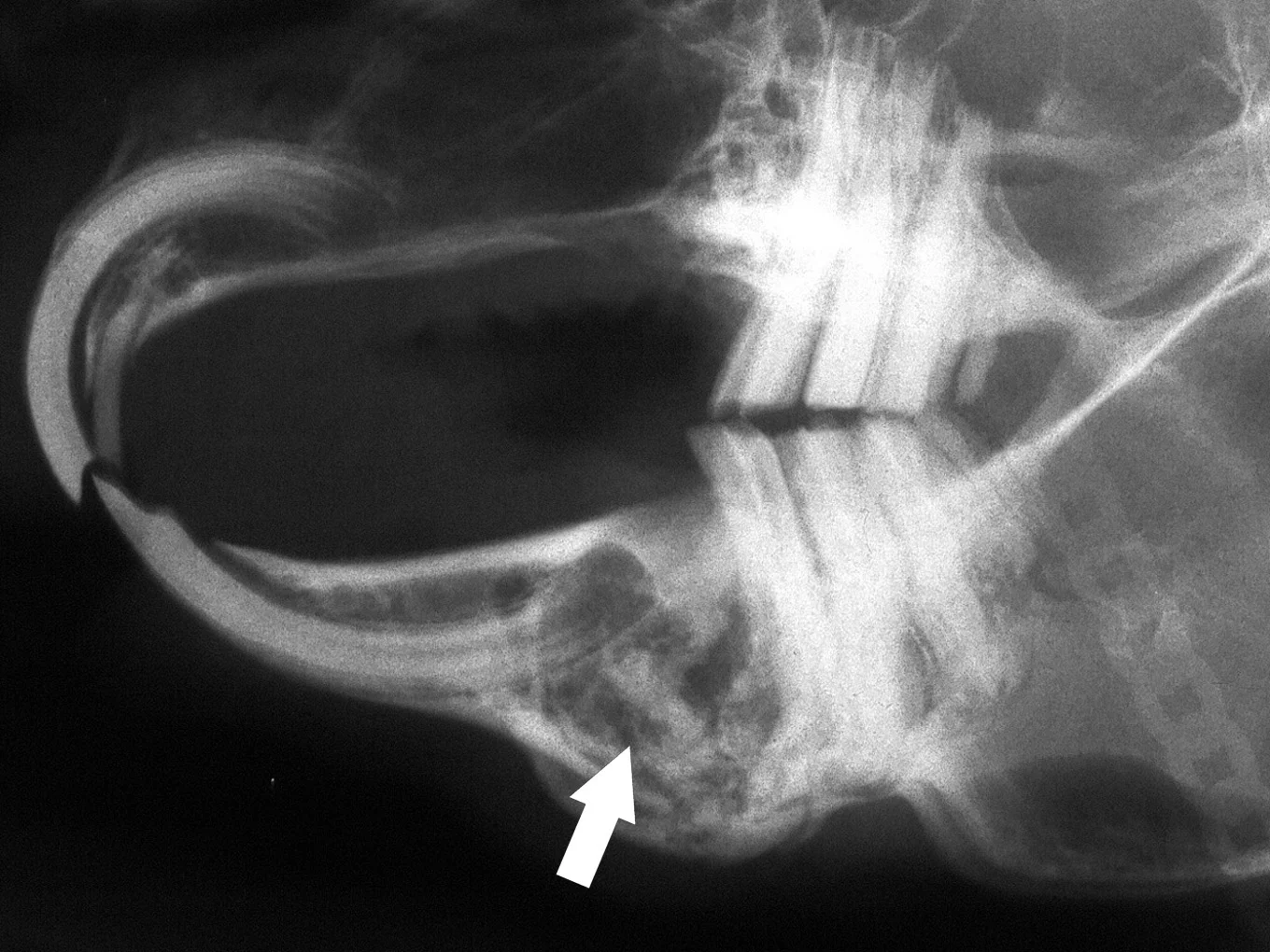
Formation of dental-related abscesses is common in pet rabbits. Most facial abscesses are a sequela to acquired dental disease, particularly dental disease as a result of metabolic bone disease or tooth fracture. Frequently, they develop from periapical infection of mandibular cheek teeth and typically involve both hard and soft tissues. Therefore, common radiographic abnormalities include a fragment of a mandibular cheek tooth associated with mandibular osteomyelitis. The cheek tooth fragment is usually visible in a circular radiolucent lesion that contains purulent material (Figure A).
The abscess develops gradually and can become very large relative to the size of the patient. In rabbits and rodents, abscesses are usually not painful, do not affect prehension of food and chewing, and do not cause hyperthermia. They are surrounded by a very thick capsular wall and usually contain white, dense, creamy purulent material. Facial abscesses rarely respond to antibiotic therapy alone. Treatment must include surgical intervention, and aggressive debridement is generally recommended.
A number of techniques have been proposed, including simple flushing after incision and/or introduction of antibiotic-impregnated polymethylmethacrylate beads. In the author's experience, the highest rate of success is achieved with:• Surgical excision and debridement of the entire abscess, including the capsule• Extraction of affected tooth/teeth• Debridement of the infected/necrotic bone• Marsupialization of the soft tissues• Frequent postoperative flushing and debridement of the site• Application of antiseptics, antibiotics, and/or products to promote healing into the surgical site until complete healing occurs by secondary intention.
Patients should be evaluated and selected carefully before performing surgery. A complete and accurate diagnosis based on clinical and radiographic findings is critical to determine prognosis. Of equal importance is the level of expected owner compliance, as these patients will require frequent postsurgical examinations (in some cases for the rest of the patient's life) and moderately intensive home care. Owners should also be informed that, after this procedure, the rabbit may be temporarily unappealing cosmetically.
Poor owner compliance may result in disappointing overall outcomes. It should be taken into consideration that in cases of very severe dental disease, complications, or poor prognosis, euthanasia may be the most appropriate and humane choice for the welfare of the patient.
Step-by-Step: How to Treat Periapical Mandibular Abscess in Rabbits
Step 1
Place the anesthetized rabbit in lateral or dorsal recumbency, depending on the site of infection. Shave and aseptically prepare the area. The rabbit is shown here with anesthetic face mask in place.

Step 2
Make a skin incision over the mass, taking care not to incise the capsule and to avoid entering the underlying abscess.
Procedure Pearl
A transparent drape (preferably adhesive) facilitates the view of the orientation of the head and anesthetic monitoring.

Step 3
Dissect free subcutaneous and muscle layers to expose as much of the abscess capsule as possible.

Step 4
When most of the capsule has been dissected free, incise its junction with the mandibular bone using a scalpel blade or pointed scissors. In cases of periapical mandibular abscesses, the wall of the mass is typically composed of thick connective tissue and thin cortical bone, which prevents removal of the entire capsule in one piece. The remaining part of the capsule can be carefully debrided later, using a curette. In case of mandibular abscesses that do not affect the apex, actually about half of the abscess wall is the capsule, and the other half is "carved" into the bone (which will be debrided).

Step 5
After the incision, carefully dissect free and remove the lateral wall of the abscess.

Step 6
Remove the purulent material using a Volkmann spoon or cotton swabs, and flush the bone cavity.
Procedure Pearl
When incising the skin over the mass, the surgeon should take care not to incise the capsule and disrupt the underlying abscess.
Procedure Pearl
Samples for culture and sensitivity should be collected from the capsule wall, as the purulent material itself is usually sterile.

Step 7
Debride the bone cavity thoroughly using a bone curette to remove the remaining debris and purulent material. Debride the infected or necrotic cortical bone to the point of bleeding using a small pair of rongeurs or needle holders. Keep in mind that this step alone will not be enough to resolve osteomyelitis. Failure to remove all of the infected or necrotic cortical bone results in a high rate of treatment failure.

Step 8
When debridement is complete, the involved cheek tooth/teeth or their fragments can be seen directly from the osteotomy site. A Crossley's luxator for cheek teeth or a hypodermic needle may be used gently to free the attachment of the tooth fragment to the bone.

Step 9
Extract the involved tooth/teeth using small extraction forceps or a needle holder (A). The teeth or fragments are sometimes deformed and may be attached to a fragment of necrotic osteomyelitic alveolar bone (B). The diseased overgrown premolar and molar teeth extracted from sites of abscessations have a typical"L-shaped" deformity of the apex (C).
Procedure Pearl
During the delicate extraction phase, it is important to prevent accidental fracture of the mandible, which is more likely when bone osteolysis due to bone infection is severe.

A
Step 10
Debride once again and thoroughly flush the bone cavity with saline. After surgical debridement of the osteomyelitic site, the bone appearing at the bottom of the cavity is actually the lateral side of the medial cortex of the mandible.

Step 11
Perform marsupialization of the soft tissues around the surgical site using 3-0 suture material, which will allow the postoperative flushing and debridement that is critical for healing by secondary intention. In the author's experience, this procedure highly reduces the risk of recurrence. The method requires a longer and more difficult posttreatment period; however, the ability to access the surgical site directly makes this method preferable to implantation of antibiotic-impregnated beads or other similar techniques.

Step 12
Owners should be prepared for the typically unattractive postoperative appearance of marsupialization of soft tissues (A). The postoperative radiograph shows a wide radiolucent area corresponding to the debrided bone site, and the tooth fragment is no longer visible (B).

A
Step 13
Sutures are usually removed from the marsupialization site 10 to 12 days postoperatively. After 2 weeks, the bone cavity is filling with new connective tissue and other deep soft tissues are healing, reducing the size of the fistula (A). In about another week, the overlying skin will be completely healed (B). Longer term follow-up (6 to 8 weeks after surgery) includes radiographic evaluation to demonstrate remodeling and apposition of new bone in previous sites of osteomyelitis.

A
Postoperative Care
Postoperative care following marsupialization includes daily flushing, frequent debridement of hard and soft tissues, local application of an antimicrobial ointment, and administration of systemic antibiotics and analgesics. Anorexic rabbits must be encouraged to eat as soon as possible after surgery. Commercial hand-feeding products, such as Oxbow Critical Care (Oxbow Enterprises; www.oxbowhay.com) are excellent for this purpose. Adjunct fluid therapy may be necessary.
Some owners may be able to perform part of the postoperative care at home. Rabbits can usually be adequately and safely restrained and local therapy performed without sedation. The use of an Elizabethan collar to protect the surgical site is seldom necessary. Frequent recheck examinations are mandatory for a successful outcome and should be discussed with the owner prior to surgery.