Surgical Laser Basics: 5 Tips for the Novice User
The CO2 laser is the predominant surgical laser used for soft tissue surgery because of its unique interaction with tissue. CO2 lasers emit an invisible beam of laser light (10,600 nm) that is highly absorbed by water. The absorbed energy is converted into heat, cells are ruptured, tissue is vaporized, and most of the energy delivered to the tissue is released in a plume of steam and cellular remnants.1 The highly focused beam of a CO2 surgical laser is a versatile and precise “knife,” that can efficiently vaporize soft tissue while simultaneously sealing small blood vessels, lymphatic vessels, and nerve endings.<sup2,3 sup>
When properly used, a CO2 laser creates as little as 100 microns of collateral thermal change in tissue. Within this zone of thermal change lie the benefits of CO2 laser surgery. Sealed blood vessels reduce hemorrhage and increase visualization of the surgical field, sealed lymphatic vessels reduce postoperative edema and swelling, and sealed nerves lessen postoperative pain.<sup4-9 sup>
To maximize these benefits and achieve the best surgical outcome, the laser power (watts), spot size (diameter of the laser beam contacting the tissue in cm2), and delivery mode (continuous, single-pulse, multiple-pulse) must be set appropriately, and the surgeon must use appropriate technique.
1. Use a Sharp Laser Knife
Power density (ie, intensity of the laser beam applied to an area of tissue in watts/cm2) dictates how sharp the knife-like laser beam is. The higher the power density is, the sharper the laser knife and the more precise the incision. Power density can be altered by changing either the power or the spot size. A higher power density allows for faster hand speed, shorter time of tissue exposure to the laser energy, and reduced tissue damage.5,10
2. Be Quick
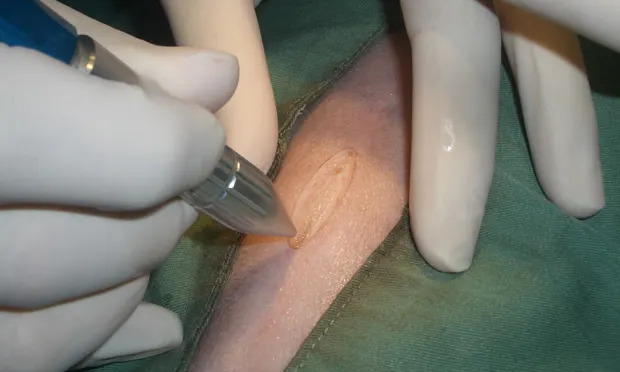
The best tissue effect results from exposing tissue to laser energy over the shortest length of time. Use a combination of power, spot size, delivery mode, and hand speed that allows full-thickness incisions to be made in a single pass (Figure 1).

A full-thickness, single-pass CO2 laser incision causes minimal thermal tissue change. Photo courtesy of Dr. Masahiro Seki
Do not saw through tissue with multiple partial-thickness cuts. Partial-thickness incisions result in repeated tissue exposure to the laser beam. Each exposure increases the width of the zone of collateral thermal change in the tissue and contributes to cumulative damage. Sawing through an incision with a CO2 laser can lead to burned tissue, carbon (char) formation, thermal necrosis, delayed healing, and possible dehiscence.<sup5,11 sup>

Hold the laser handpiece perpendicular to the tissue, and the correct distance from the tissue, to ensure a predictable spot size of laser light on the tissue. Photo courtesy of Dr. Paul J. Sessa
3. Be Focused
Minimize the spot size by directing the laser beam perpendicular to the tissue8 (Figure 2). Know the correct distance the delivery handpiece should be from the tissue (usually 1-3 mm) to deliver the desired spot size. Avoid backing away from the tissue and defocusing the laser beam unless the goal is to produce a low-temperature, non-evaporative thermal change within the tissue. Defocusing is not appropriate except for contraction of a tissue area for hemostasis of small vessels.4,10

Apply tension to tissue when incising and dissecting. Tissue under tension cuts more quickly, resulting in reduced collateral thermal change and better tissue effect. Photo courtesy of Dr. William E. Shultz
4. Apply Tension
Whether incising or dissecting, tissue needs to be under tension while being cut. Tension separates tissue as it is cut, exposing new tissue to the laser beam. Tissue cuts more quickly while under tension, resulting in less collateral thermal tissue change4,5,8 (Figure 3).
5. Use the Apps
Like apps on a mobile device, CO2 lasers have software programs. These programs adjust emission of the laser light. The laser light can be emitted continuously, as single pulses, or as a series of pulses. Using these apps can help the surgeon adjust tissue effect:
Continuous delivery: The laser energy is delivered as long as the foot switch is depressed. Continuous delivery is used for routine incisions and dissection where rapid vaporization of tissue is desired.
Single-pulse delivery: One timed pulse of laser energy is delivered when the foot switch is depressed. Single-pulse delivery produces a very brief (10-500 msec) pulse of laser light that can be used to precisely remove very small amounts of tissue. This can be useful when performing dissection in areas of critical anatomy.
Multiple-pulse delivery: A series of pulses of laser light are delivered whenever the foot switch is depressed.10 Each individual pulse maintains effective power density, but because of the pause between pulses, the rate of tissue removal is slower.12 Multiple-pulse delivery can be useful to achieve good tissue effect when precision requires a slower hand speed (eg, excision of a meibomian gland tumor).
Superpulse: Some CO2 lasers also give the option of delivering the laser beam in either superpulse (SP) or non-superpulse (NON SP) mode. SP mode produces a series of microseconds-long (<800 µsec) very high-energy (60-80 watts) pulses. The time between each high-energy pulse is longer than the time required for thermal relaxation (cooling) of the tissue. In SP mode, the average power delivered over a period of time is the power selected on the laser control panel.
In devices equipped with SP capability, SP can be turned on or off whether in continuous, single-pulse, or multiple-pulse delivery.
Excessive collateral tissue change and char formation occur when tissue absorbs heat faster than it can be released by conduction, convection, circulation, and evaporation. Superpulse can help limit collateral tissue change by allowing increased thermal relaxation of the tissue. Since hemostasis occurs in the zone of collateral tissue change, SP mode can interfere with hemostasis if the zone of reversible collateral tissue change becomes too narrow. Use NON SP mode in more vascular tissue where more hemostasis is needed and SP mode in less vascular tissue.
Closing Thoughts
The CO2 surgical laser is an easy tool to adopt in soft tissue surgery. To do so, beginners need to understand the basic concepts of CO2 laser–tissue interaction and are encouraged to attend an introductory CO2 laser workshop. They need to know their laser’s power capacity and how to adjust it, how the laser’s control panel affects delivery of the laser beam, and how the laser’s delivery handpiece is properly positioned in relationship to the tissue.
With that knowledge, beginners will be able to start using laser parameters recommended in introductory courses and by laser manufacturers to achieve good surgical outcomes. Starting with their first surgery, novices can contribute to those good outcomes by applying the tips mentioned here—be quick, be focused, apply tension, and use the apps!
Dr. John Godbold works full time with Stonehaven Veterinary Consulting to provide laser technology education to colleagues. Since 2001. Dr. Godbold has taught laser surgery to thousands of colleagues in over a dozen countries. His CO2 laser courses have been repeated 11 years at The NAVC Conference. Dr. Godbold published the internationally distributed CD ROM Atlas of CO2 Laser Surgery Procedures in 2002, with a new edition each year since. In high demand as a veterinary laser technology trainer, he has spoken at more than 500 workshops, wet-labs, and continuing education courses throughout the world.