Submandibular Lymphadenopathy: The Cytologist’s Challenge
Amy L. Weeden, DVM, University of Florida
Heather L. Wamsley, DVM, PhD, DACVP, University of Florida
This case series highlights specific considerations that must be kept in mind during cytodiagnosis of submandibular lymph node aspirates.
Aspirate cytology of submandibular lymph nodes is commonly used to screen for multiple causes of peripheral lymphadenomegaly. Submandibular lymph nodes are often among the first evaluated by clinicians because they are readily accessible and easily sampled. This case series highlights specific considerations that must be kept in mind during cytodiagnosis of submandibular lymph node aspirates.
Related Article: Lymph Node Cytology
Case 1: Rhinitis

Figure 1. A mixed lymphoid population is noted on a white background with many blue, round cytoplasmic fragments and RBCs. Small lymphocytes (green arrows), intermediate lymphocytes (black arrows), and plasma cells (red stars) are present. (Wright-Giemsa stained lymph node aspirate, 500×, bar = 10 µm)
A 9-year-old spayed domestic short-haired cat was presented for rhinitis with ulceration of the mouth and nares. Physical examination showed moderate enlargement of the submandibular lymph nodes with no additional lymph node enlargement. A sample was obtained on fine-needle aspiration (FNA) (Figure 1).
Ask Yourself
What size lymphocyte predominates?
Why are the lymph nodes enlarged?
Diagnosis
Reactive Lymphoid Hyperplasia, Presumably Secondary to Viral Rhinitis & Stomatitis
Interpretation & Discussion
Reactive lymphoid hyperplasia is frequently observed in submandibular lymph nodes because they drain the oral and nasal cavities and part of the ear. These areas are common sources of antigenic stimulation that results from periodontal disease, otitis, and rhinitis.

Figure 2. A reactive lymphoid population is present. Small lymphocytes predominate (red arrows). Intermediate lymphocytes are increased (black arrow). A plasma cell (red star), lymphoblast (green arrow), and a highly granulated mast cell (green star) are also shown. (Wright-Giemsa, 500×, bar = 10 µm)
Normal lymph nodes are composed of 80%–90% small lymphocytes, and small lymphocytes typically predominate in hyperplastic nodes. Hyperplastic lymph nodes contain increased intermediate lymphocytes, plasma cells, lymphoblasts, and sometimes other inflammatory cells (eg, neutrophils, macrophages, eosinophils). Although increased, the lymphoblast percentage in hyperplastic lymph nodes is usually less than 10% to 20% of all lymphoid cells.
When lymph node enlargement secondary to reactive lymphoid hyperplasia is observed, a thorough search for a source of antigenic stimulation should follow. When multiple lymph nodes are affected, systemic causes of antigenic stimulation should be considered.
When a single node or regional nodes are affected, anatomic sites drained by the node or nodes should be evaluated. In this case, the reactive lymphoid hyperplasia was related to the patient’s upper respiratory disease, which likely had a viral cause.
Case 2: Rhinitis

Figure 3. Representative field of a submandibular lymph node FNA (Wright-Giemsa, 500×, bar = 10 µm)

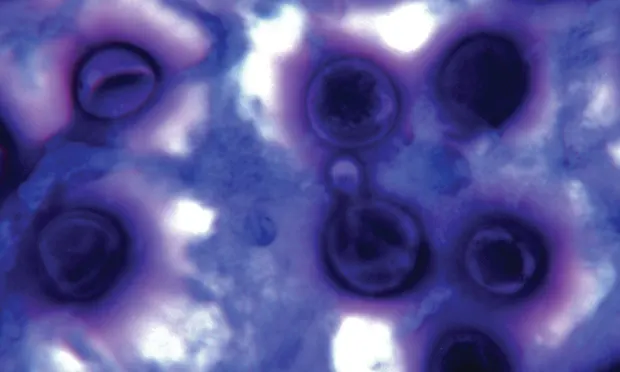
Figure 4. Higher magnification of Cryptococcus species. Note the narrow-based budding near the center of the image (thin arrow). A single organism with a non-staining capsule is shown at the arrowhead. (Wright-Giemsa stained lymph node aspirate, 1000×)
A 6-year-old, castrated domestic short-haired cat was presented with left-sided nasal discharge unresponsive to therapy with antibiotics or corticosteroids. The submandibular lymph nodes were enlarged bilaterally, and samples were obtained on FNA (Figure 3).
Ask Yourself
Is a lymphoid population present?
What is the cause of this cat’s rhinitis?
Diagnosis
Disseminated Cryptococcal Infection
Interpretation & Discussion
This patient’s intranasal disease would have been inaccessible for diagnostic sampling without sedation or anesthesia. Because of discomfort caused by the primary disease, a deep swab of the nasal discharge was not possible. However, aspiration of the submandibular lymph node was tolerated. Submandibular lymph node cytology yielded an etiologic diagnosis for the rhinitis through inexpensive and minimally invasive means.
Case 3: Pigmented Oral Mass

Figure 5. Two representative 500× fields from the submandibular FNA are pictured. (Wright-Giemsa; bar = 10 µm)
A 10-year-old golden retriever was presented for halitosis. Oral examination showed an irregular, pigmented, right mandibular gingival mass. The ipsilateral submandibular lymph node was also enlarged, and a sample was obtained on FNA (Figure 5).
Ask Yourself
Is a lymphoid population present?
What criteria of malignancy or atypical features are present?
Do granules in the cytoplasm aid in cell identification?
Diagnosis
Metastatic Poorly Pigmented Melanoma

Figure 6. Lymph node. The cells are pleomorphic and some contain fine, black or green-black melanin. Malignant features include binucleation (arrow), nuclei that crowd each other (red star), a mitotic figure (black star), and large or irregular nucleoli. A large melanin-filled macrophage (melanophage) is present in the upper right (arrowhead). Note the globular nature of the pigment, which helps differentiate this cell from the melanocytes. Given the pigmented mass in the oral cavity, these findings are consistent with metastatic melanoma, which has invaded and replaced the lymphoid tissue. (Wright-Giemsa, 500×, bar = 10 µm)
Interpretation & Discussion
Obtaining diagnostic material from the oral cavity of an awake, alert patient is difficult. In this patient, clinical suspicion for melanoma was high, so efficient diagnosis and timely treatment was important. A minimally invasive and rapid way to obtain diagnostic material is through aspiration of the draining lymph node.
Neoplastic melanocytes in the submandibular lymph node aspirate supported that the pigmented gingival mass was metastatic and predicted the identity of the primary mass. Oral melanomas usually metastasize quickly. The submandibular lymph nodes are an early site for metastatic spread of these neoplasms. Because the submandibular lymph nodes drain the oral cavity, the lack of lymphoid cells in the aspirate is consistent with replacement of normal lymphoid tissue by neoplastic melanocytes that spread from the pigmented gingival mass to the submandibular node (Figure 6). Thoracic radiographs could screen for further metastatic spread. Histopathology could be used to further confirm the identity of the pigmented gingival mass and confirm that the submandibular tissue aspirated is a lymph node replaced by neoplastic cells, rather than a primary neoplasm.
When staging facial neoplasms, submandibular lymph nodes are commonly evaluated cytologically or histopathologically. Microscopic evaluation should be performed even when lymph nodes are not enlarged, as metastatic disease may be present in normally sized nodes.1
Case 4: Enlarged Submandibular Lymph Nodes Observed During An Annual Wellness Examination

Figure 7. A small sheet of epithelial cells is present with abundant foamy cytoplasm. The round nuclei are uniform in size. Some contain a small, round nucleolus. The nucleus:cytoplasm ratio is low. Note the linear arrangement of the RBCs in the background. This effect is called windrowing and is seen in aspirates with a viscous fluid background. (Wright-Giemsa, 500×, bar = 10 µm)
A 5-year-old spayed Chihuahua was presented for wellness evaluation. Mild dental disease and enlarged submandibular lymph nodes were observed. No other abnormalities were noted. Samples were obtained on FNA (Figure 7).
Ask Yourself
Is the sample representative of lymph nodes?
What is the source of the cells in this aspirate?
Diagnosis
Inadvertent Aspiration of Normal Salivary Gland
Interpretation & Discussion
When attempting aspiration of the submandibular lymph node, sampling of only the salivary gland or both the salivary gland and lymph node, because of their close proximity, may occur. To interpret the findings from such samples, one must have knowledge of normal salivary gland cytology.
The windrowing effect described in Figure 7 is consistent with aspiration of mucinous salivary secretions. The benign appearance of the foamy secretory cells (ie, abundant cytoplasm, low nucleus:cytoplasm ratio, uniform nuclear size and appearance) and cohesive arrangement in a sheet is consistent with normal salivary gland.
The small size of the patient made isolation of the lymph node difficult and resulted in aspiration of the salivary gland. Repeat FNA revealed reactive lymphoid hyperplasia, which was a response to the patient’s dental disease.
Case 5: Enlarged Peripheral Lymph Nodes

Figure 8. Representative field of an FNA from a submandibular lymph node (Wright-Giemsa, 500×, bar = 10 µm)
A 10-year-old spayed terrier crossbreed was presented for evaluation of enlarged lymph nodes. Physical examination disclosed generalized peripheral lymphadenopathy. No other abnormalities were noted.
The submandibular lymph nodes were most severely affected, and aspirates at multiple sites were obtained (Figure 8).
Ask Yourself
What is the predominant lymphoid cell?
What is the cytodiagnosis?
Diagnosis
Lymphoma
Interpretation & Discussion
When evaluating submandibular lymph nodes for lymphoma, exercise caution. Inadvertent sampling of the salivary gland is a potential pitfall associated with sampling of submandibular lymph nodes, as was noted in Case 4. Also, antigenic stimulation of the submandibular lymph nodes is nearly constant, as these nodes drain the oral cavity, nasal cavity, and part of the ear, as seen in Case 1. Increased lymphoblasts are seen in aspirates from hyperplastic lymph nodes and lymph nodes with lymphoma.

Figure 9. Higher magnification of the lymphoblasts. Note the larger size and paler chromatin compared with the small lymphocyte in the field (arrow). A large nucleolus is present in the cell at the top right. A lysed cell is present at the bottom (red star). Use caution not to interpret lysed cells when evaluating lymph nodes. Free nuclei from lysed cells swell and may mimic lymphoblasts due to larger size, paler chromatin, and nucleoli made prominent due to technical artifact. The lack of a defined cytoplasmic or nuclear border distinguishes lysed cells from intact ones. (Wright-Giemsa, 1000×)
Concern for lymphoma should be raised when over 30% of the lymphoid population consists of lymphoblasts. Accordingly, cytologic diagnosis of lymphoma is based on observing greater than 50% lymphoblasts and is readily performed when lymphoblasts approach 80% to 90% of the cells, as in this case. Difficulty in definitive lymphoma diagnosis arises when the lymphoblast percentage is closer to the gray zone cut-off of 30%.
In aspirates from chronically antigenically stimulated, hyperplastic submandibular lymph nodes, it is possible to find areas on the slide where the number of lymphoblasts approaches the gray zone. In such instances, the possibility for lymphoma becomes a concern, but the potential that the lymphoblasts are increased simply because of antigenic stimulation is also likely.
In this patient, diagnostic confidence may be gained by concurrent evaluation of aspirates from additional lymph nodes to determine if they have greater than 50% lymphoblasts. Molecular diagnostics such as PCR may also be useful, but these require additional time and financial investment.
Imaging and minimum database testing were performed for staging in this case. There were no additional significant findings. Additional popliteal lymph node FNAs were performed and yielded findings similar to those shown in Figures 8 and 9. Lymphoma was confirmed in this case by the predominance of monomorphic lymphoblasts in this and other lymph node aspirates.
Conclusion
Minimally invasive submandibular lymph node aspirates can be used as a sentinel for oral or intranasal disease as diagnostics tests of these anatomic sites are, in general, poorly tolerated without heavy sedation or anesthesia of small animal patients. Submandibular lymph nodes are easily accessible and often sampled to screen for infection, inflammation, antigenic stimulation, and metastatic neoplasia.
Related Article: Lymph Nodes: How to Obtain Excellent Specimens
There are downsides associated with submandibular lymph node aspirates. Incidental salivary gland sampling is possible, and lymphoblasts are typically mildly to moderately increased, which can confound lymphoma diagnosis. When a patient has multiple enlarged lymph nodes, it is prudent to sample other nodes concurrently, such as the prescapular or popliteal lymph nodes, to avoid potential pitfalls associated with submandibular lymph node aspirates.
FNA = fine-needle aspiration