Mesenchymal Stem Cell Therapy
Nicole S. Amato, DVM, DACVS (Small Animal), Massachusetts Veterinary Referral Hospital, Woburn, Massachusetts
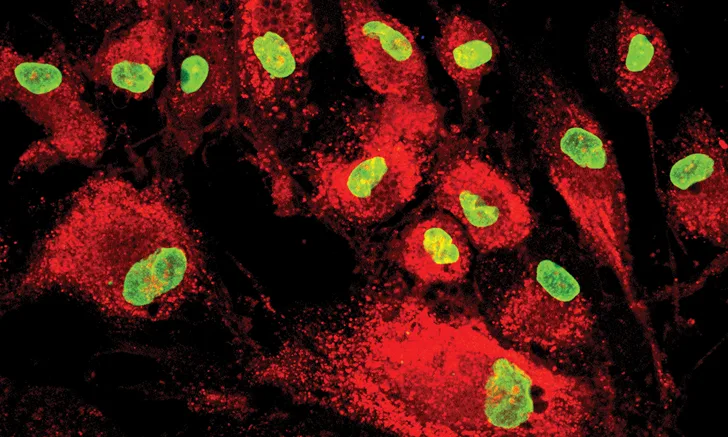
Mesenchymal stem cells with fluorescent molecules
Mesenchymal stem cell therapy (MSCT) involves use of adult-derived mesenchymal stem cells to potentially restore health and proper function to damaged or diseased cells, tissue, and/or organs. MSCT has been widely researched in human medicine and used to treat osteoarthritis (OA), tendinopathies, and sports-related injuries, inspiring veterinary research to evaluate this modality in dogs. Research supporting MSCT in veterinary musculoskeletal disease management is still minimal.
There are 2 types of mammalian stem cells: those of embryonic origin and those derived from adult tissue.1 Embryonic stem cells are totipotent and capable of differentiating into any cell type, whereas adult-derived stem cells are multipotent and capable of differentiating into more than one but not all cell types. Derived from a mesodermal lineage, adult-derived stem cells (ie, mesenchymal stem cells) exist naturally as a reserve in muscle, fat, cartilage, bone and bone marrow, and tissue that make up the circulatory, urinary, and reproductive systems.1-3 In their natural state, activated mesenchymal stem cells undergo cell division to give rise to other cells that eventually function in a fully differentiated state,1,2 replacing dead cells in the process of tissue renewal.4 Mesenchymal stem cells may also mobilize and proliferate in response to injury or pathologic conditions, theoretically creating a basis for therapeutic application.4,5
The International Society for Cellular Therapy has proposed a set of minimum criteria to qualify a cell as a therapeutic mesenchymal stem cell. The cell must be able to exhibit plastic adherence, possess specific sets of cell surface markers while lacking others, and be capable of differentiating into adipocytes, chondrocytes, and osteoblasts in vitro.6 Although these criteria are universal, there has been no standardization of terminology; thus, various terms (eg, stem cell, mesenchymal stem cell, mesenchymal stromal cell) are commonly used interchangeably, which can be confusing when navigating the literature and clinical studies. The International Society for Cellular Therapy has proposed the term mesenchymal stromal cell be used in reference to tissue harvested from bone marrow and fat and processed for MSCT use,7 based on the contention that these ex vivo isolated cells are a heterogeneous population of fibroblast-like cells that can self-renew and differentiate in culture but may not meet all criteria to be defined as true stem cells.7,8 Thus, the term stromal cell has been adopted for the products most commonly used in regenerative medicine.7,8 For the purposes of this article, the term mesenchymal stromal cell (MSC) will be used.
MSCs for Therapeutic Use
Adult-derived MSCs for therapeutic use can be subdivided into autologous (ie, those derived from the same animal), allogenic (ie, those derived from a different animal of the same species), and xenogenic (ie, those derived from an animal of a different species). Most research in dogs has been focused on adult-derived autologous MSCs,3 although investigation of the use of allogenic and xenogenic cells is underway.9,10
Adult-derived MSCs for therapeutic use are thought to assist in tissue regeneration and repair through angiogenesis enhancement, inflammation reduction, immune modulation, fibrosis inhibition, and the recruitment, survival, and proliferation of local stem cells at the site of injury.4,5,10 Although much regarding MSCs is known from in vitro and in vivo investigation, a complete understanding of how these cells function in vivo in any species once administered is not known.
There are several sources of therapeutic MSCs (eg, bone marrow, adipose tissue, umbilical cord tissue, amniotic fluid, dental pulp, peripheral blood, skeletal muscle).1-5 Common sources in veterinary orthopedics are bone marrow and adipose tissue; however, the processing of this tissue to isolate MSCs varies, and no cell source or isolation method has been established to be superior over the other.
Culture-Expanded & Noncultured Products
MSCs can be divided into culture-expanded and noncultured models.1-5
Culture-Expanded
Culture-expanded models involve harvesting tissue (eg, bone marrow, fat), then isolating, processing, and expanding the stromal cells using culture techniques.11 An expanded product contains more stromal cells than the original sample, creating a more homogeneous population for administration.11 In the literature, cultured products are commonly referred to as bone marrow MSCs (BM MSCs) and adipose tissue-derived or adipose-derived MSCs (AD MSCs), among others.
Noncultured
Noncultured models involve harvesting and processing fat or bone marrow so the existing cells become concentrated but not expanded. This more heterogenic product is a combination of MSCs and other cellular components (eg, mononuclear cells normally found in these tissue types).11 Although cultured products may seem more desirable due to the larger number of purified cells in the final product, the harvested sample in cultured products takes 3 to 6 weeks to process before it can be administered.12 Thus, noncultured products may be more convenient for clinical scenarios and are described below.
Bone marrow aspirate concentrate (BMAC) is a concentrated—but not cultured—heterogeneous population of cells derived from a traditional bone marrow aspirate. As compared with a traditional bone marrow aspirate, BMAC has a higher population of MSCs but not as many as the culture-expanded forms previously described.12 A benefit of BMAC is the provision of other cell populations, growth factors, and fibrin, which may aid in the healing process and provide a scaffold for cells and other substances at the treatment site.12,13 Adipose-derived stromal vascular fraction cells—not to be confused with the culture-expanded AD MSCs—are an alternative to BMAC and are harvested from fat and processed without cultured cellular expansion.14,15 The result is a heterogeneous product of MSCs that likely contain a milieu of other cells in its stroma.14-16
Bone Marrow MSCs vs Adipose-Derived MSCs
Studies comparing the effectiveness of BM MSCs with AD MSCs in the treatment of orthopedic conditions in dogs or comparing cultured with noncultured products are lacking. However, there has been some investigation into the basic differences between BM MSCs and AD MSCs, such as cell proliferation, stem cell marker expression, and lineage-specific differentiation potential.11,14,17 Although BM MSCs and AD MSCs resemble each other morphologically and in expression of markers, they display differences in proliferation rate and differentiation potential into chondrogenic and osteogenic directions. In a study comparing AD MSCs with BM MSCs, AD MSCs exhibited faster population doubling but weaker differentiation into chondrogenic and osteogenic directions.11 In addition, greater numbers of MSCs have been found in adipose tissue,18,19 but it is not known if the number of MSCs in a sample is clinically significant.18
Although the clinical meaning of these differences and the clear advantages or disadvantages to either tissue source for MSCT are unclear, AD MSCs may offer a potential advantage due to ease of harvesting. Although bone marrow aspiration is a relatively routine procedure, fat can generally be found in abundant quantities in most patients and can be harvested through a surgical procedure that may be less invasive and painful as compared with bone marrow harvesting. Further research is needed to determine which approach, if either, offers greater benefits regarding efficacy and safety or conditions that may potentially be targeted by this therapy.
Clinical Impact
MSCT has been investigated and used clinically in dogs to treat OA,20-30 ligament injuries (eg, partial cranial cruciate ligament tears),31-36 and tendinopathies (eg, supraspinatus tendinopathy).37
Chondrocytes are easily damaged and heal poorly due to their low mitotic ability and due to their lack of blood and lack of lymphatic and nerve supply,38 making them an ideal therapeutic target for MSCT in dogs and humans.5 Several studies have investigated the use of AD MSCs for the treatment of naturally occurring OA affecting the canine hip, elbow, and shoulder joint.20-30 Most of these studies were well-designed, placebo-controlled, blinded, and randomized; many demonstrated reduction in pain on manipulation and range of motion20,21 and improvement in owner satisfaction20,21,25 and in subjective grading scale and objective lameness measurements.24,27,29 It is unclear whether the beneficial effects seen in these studies were due to the anti-inflammatory effects of MSCs, the repair or regeneration of articular cartilage, or a combination of these mechanisms.33,34
The investigation of MSCT in the treatment of other small animal orthopedic conditions (eg, cranial cruciate ligament tears) has been fueled by in vivo studies that have shown the potential for MSCs to engraft into the cranial cruciate ligament, meniscus, and cartilage.32,35,36 Although data are sparse, there is some clinical evidence suggesting that MSCs may be able to augment healing of early partial tears prior to development of mechanical instability, offering a potential nonsurgical solution.31
Use of culture-expanded BM MSCs in the treatment of tendon injuries has been investigated in experimental studies of horses and laboratory animals; MSCs were implanted in surgically or collagenase-induced tendon lesions and had positive effects on tissue organization, composition, and mechanics of these structures.37-40 In a veterinary clinical study, a combination of AD MSCs and platelet-rich plasma was used to treat supraspinatus tendinopathy in 55 dogs, 61.8% of which failed to respond to NSAIDs and 45.5% of which failed to respond to rehabilitation therapy.41 Improvements in objective gait analysis, lameness, and diagnostic ultrasonography results (ie, improved fiber pattern and tendon size) showed that AD MSCs combined with platelet-rich plasma may show promise in the treatment of this condition in dogs.41 Additional studies are needed to better evaluate MSCT in the treatment of this and other tendon injuries in dogs.
MSC PROCUREMENT, PROCESSING, & ADMINISTRATION
Although all types of MSCs can be sent to laboratories for processing and culture-expanding procedures, centrifuges that can process both adipose-derived stromal vascular fraction cells and BMACs are available to allow for more convenient processing and administration and to avoid delays between procedures. Laboratories are available to provide culture-expanded products. It is unknown if a single injection or a series of injections over time is needed to optimize therapeutic benefit.
Procurement
Patients should be sedated or anesthetized, and a fat retrieval procedure or bone marrow aspiration should be performed. In dogs, bone marrow is most easily obtained from the proximal humerus, tibia, ilium, or femur. Adipose tissue can be harvested from the axillary or inguinal region or where fat is abundant.
Processing
For noncultured products, samples should be processed onsite in a specially designed centrifuge or sent to a laboratory for concentration and separation of the mononuclear layer. For culture-expanded products, a further step is performed for cell expansion in a laboratory.
Administration
Administration is most commonly performed locally to target tissue (eg, intralesionally into tendons, ligaments, or joints). The method of administration depends on the target tissue. Tendon therapy generally requires ultrasonography guidance under heavy sedation or anesthesia, whereas the treatment of OA or cranial cruciate ligament injuries only requires a joint injection under sedation.
Recovery
Most patients recover as outpatients following administration. The author recommends treating patients postinjection with parenterally administered opioids (eg, buprenorphine [0.01-0.015 mg/kg IV or SC]) or oral analgesics (eg, gabapentin [5-10 mg/kg PO]). It is unknown whether administration of NSAIDs after MSCT therapy is detrimental to efficacy. After the procedure, most patients are enrolled in a physical rehabilitation program to further treat the underlying condition being targeted.
Advantages
Although the advantages of MSCT have yet to be fully elucidated, a possible advantage of MSCT is its potential in the management of OA. OA affects an estimated 20% of the canine population42 and can be challenging to manage, particularly in patients refractory to traditional medical management (eg, weight control, physical rehabilitation, nutraceuticals, NSAIDs, intra-articular therapies).43-45 MSCT may prove to be an alternative to managing signs in clinically affected dogs.
MSCT is relatively easy to carry out in a small animal practice, owing largely to its point-of-care qualities. With a multitude of products available, preparation, processing, and administration can be performed in a properly equipped veterinary practice as opposed to a referral laboratory or research facility (see MSC Procurement, Processing, & Administration).
Disadvantages
The clinical use of MSCT is still new, and there is little information available to help guide treatment plans, develop treatment protocols, and predict patient outcomes. It is also unclear how MSCs function physiologically to provide clinical benefit to patients and how efficacious MSCT is in the treatment of different disorders and injuries, as many studies on MSCT have used different types of MSC products and vehicles of administration (eg, hyaluronic acid, platelet-rich plasma, saline).20-22,25,27,29 Experimental studies have suggested that these factors can influence clinical outcome due to cell–vehicle interaction.28
In addition, there are few comparative studies (eg, those comparing intra-articular MSCT with the current standards of care [eg, physical therapy, NSAIDs, nutraceuticals, intra-articular injections of corticosteroids, hyaluronic acid, platelet-rich plasma] in the treatment of conditions such as OA). In addition to these investigative and clinical disadvantages, MSC use in veterinary medicine can be cost-prohibitive.
OPEN QUESTIONS
Following are open questions to consider regarding areas of MSCT where data are lacking.
Does a specific tissue source offer an advantage over the other (adipose tissue vs bone marrow)? Does the tissue source chosen depend on the target tissue or disease process being treated?
What is the concentration or number of stem cells needed to allow for regeneration or repair of damaged tissue? Is treatment success or failure dose-dependent? Is the concentration disease-dependent?
How do age and health of the patient affect the outcome or success of treatment? How do pre-existing disease(s), comorbidities, or certain medications (eg, NSAIDs, steroids) affect treatment protocols?
What is the best delivery method of stem cells? Should administration always be locally to a target tissue (eg, joint, tendon), or is there a benefit to intravenous administration?
How many treatments are necessary to produce a clinical effect? Is this disease-dependent or universal?
Conclusion
Despite a lack of comprehensive evidence for the use of MSCT (see Open Questions), its clinical use in veterinary orthopedics is growing. Clinicians must be aware of the known data and have an open discussion with owners to set realistic expectations and inform them that, although MSCT offers clinical promise, it is largely experimental. MSCT may prove beneficial in the treatment of orthopedic-related injuries and conditions, but further investigation into its potential and benefits is needed.
AD MSC = adipose-derived mesenchymal stromal cell, BM MSC = bone marrow mesenchymal stromal cell, BMAC = bone marrow aspirate concentrate, MSC = mesenchymal stromal cell, MSCT = mesenchymal stem cell therapy, OA = osteoarthritis