Respiratory Distress: Diagnosis & Treatment at a Glance
DX AT A GLANCE
Upper Airway Obstruction
Clinical Signs: Inspiratory dyspnea, stridor
Differentials: Laryngeal paralysis, extrathoracic tracheal collapse, compressive masses, foreign bodies, brachycephalic syndrome
Lower Airway Obstruction
Clinical Signs: Expiratory dyspnea with auscultable expiratory wheezes
Differentials: Bronchoconstriction/spasms, bronchial wall inflammation (feline asthma, chronic bronchitis), intraluminal exudative/mucoid debris, intrathoracic tracheal collapse & bronchomalacia, bronchial compression secondary to left atrial enlargement
Thoracic Wall Disorders
Clinical Signs: Paradoxical respiration with the affected area of the thorax collapsing inward on inspiration & forced outward on expiration
Differentials: Flail chest, “sucking” chest wounds
Pleural Space Disorders
Clinical Signs: Rapid, shallow breathing patterns with inspiratory distress
Differentials: Pleural effusion, pneumothorax
Pulmonary Parenchymal Disorders
Clinical Signs: Inspiratory & expiratory difficulty; presence of heart murmurs, gallops, or arrhythmias may suggest underlying heart disease
Differentials: Pneumonia, edema (cardiogenic or noncardiogenic), pulmonary contusions, interstitial lung disease, neoplastic or fungal infiltration
Pulmonary Vascular Disorders
Clinical Signs: Hemoptysis, coughing, dyspnea, syncope; split heart sounds possible if concurrent pulmonary hypertension
Differentials: Pulmonary thrombo-embolism, heartworm disease
Severe Abdominal Distension
Clinical Signs: Inspiratory distress typically characterized by slow, exaggerated pattern
Differentials: Ascites, gastric dilatation-volvulus, organomegaly, pregnancy
TX AT A GLANCE
Upper Airway Obstruction
Sedation with acepromazine (eg, 0.025–0.2 mg/kg IV or IM) or butorphanol (eg, 0.1–0.4 mg/kg IV or IM)
Intubation, tracheostomy, etc if patent airway cannot be maintained
Glucocorticoids (eg, dexamethasone, 0.1–0.25 mg/kg IV) to reduce laryngeal & pharyngeal inflammation & edema
Active cooling for hyperthermic patients
Lower Airway Obstruction
Bronchodilators (eg, terbutaline, 0.01 mg/kg IM) to relieve bronchospasm
Glucocorticoids (eg, dexamethasone, 0.1–0.25 mg/kg IV or IM) for acute asthma in cats
Thoracic Wall Disorders
Parenteral opioids in combination with local anesthetics; NSAIDs may be used if no contraindications
Stabilization of flail segment to improve ventilation & facilitate evaluation & treatment; can impede inspiratory effort
Intermittent thoracocentesis to relieve concurrent pneumo/hemothorax
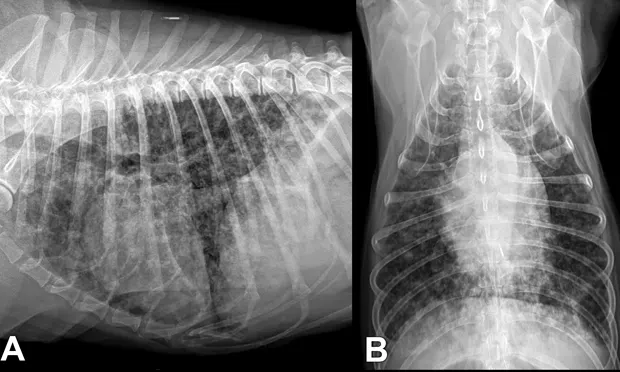
Pulmonary Parenchymal Disorders
Empirical therapy in extremely unstable patients
Thoracic radiographs for definitive diagnosis and treatment
Broad-spectrum antibiotics (eg, ampicillin, 22 mg/kg IV Q 8 H; enrofloxacin, 10–20 mg/kg IV Q 24 H for dogs & 5 mg/kg IV Q 24 H for cats), if pneumonia suspected
Loop diuretic (furosemide, initially 2–6 mg/kg IV or IM) at repeated dosing intervals for cardiogenic pulmonary edema
Supportive care, oxygen supplementation, and mechanical ventilation for noncardiogenic pulmonary edema
Pulmonary Vascular Disorders
Anticoagulants, antiplatelet medications, thrombolytics
Bronchodilators (eg, theophylline, 10 mg/kg PO Q 12 H)
Pulmonary arterial vasodilators (eg, sildenafil, 1 mg/kg PO Q 8–12 H; pimobendan, 0.25 mg/kg PO Q 8–12 H) for concurrent pulmonary hypertension