Pseudomonas Otitis Externa/Media
Profile
DefinitionInflammation and infection of vertical and horizontal ear canal and middle ear (tympanic bulla) by Pseudomonas species bacteria.
Systems. Infection can cause otitis interna with loss of hearing/damage to vestibular system (neurologic signs). Pain can cause behavioral changes/difficulty eating or chewing, leading to weight loss/depression. Infection can invade surrounding soft tissue/bone causing cellulitis/para-aural abscess. Keratoconjunctivitis sicca and facial nerve paralysis can develop from otitis media.
Geographic Distribution. Worldwide. Gram-negative suppurative otitis may be more common in tropical climates.1
SignalmentSpecies. Dogs and rarely cats.
Breed predilection. Any breed, but more common in breeds with higher prevalence of such hereditary skin diseases as allergic and seborrheic dermatitis.
Age and Range. Can occur at any age in dogs with or without underlying skin disease as trigger. Young cats with ear polyps or older cats with ear tumors at greater risk.
Gender. No sex predilection.
CausesCauses of otitis externa/media are typically divided into 3 categories: predisposing, primary, and perpetuating factors (see box).
Primary causes: Diseases for which involvement of ear pinna/canal is a "target sign." Most common are hypersensitivity disorders, parasites, keratinization and glandular disorders, foreign bodies.
Predisposing causes: Conditions leading to changes in moisture, humidity, secretions, trapping debris in ear. Factors can exist solely or develop as result of primary disease (e.g., allergic otitis externa causing stenosis of canal). Most common predisposing causes are stenosis of ear canal, floppy ears, excessive hair in canal, excessive cerumen, trauma to canal (e.g., hair plucking, excessive cleaning), obstruction by tumors/polyps, maceration of canal by moisture (i.e., swimming), or granulation tissue.
_Perpetuating causes:_Most commonly microbial infections that require treatment while a primary ear disease and/or predisposing condition is addressed. If left untreated, ear disease will not resolve. Most common perpetuating cause is overcolonization of the canal with bacteria and/or yeast.
PathophysiologyOtitis media most commonly results from extension of otitis externa through the tympanic membrane. This membrane will heal and sequester bacteria and debris in the tympanic bullae. Some factors in Pseudomonas ear infections remain unknown. In author's experience, treatment-related causes of persistent infection include inadequate treatment of initial infection, lack of deep ear cleaning, subtherapeutic doses of fluoroquinolones, use of potent aminoglycoside or fluoroquinolone-glucocorticoid otic preparations as first-line treatments for non-gram-negative infections, and lack of follow-up care.
SignsHistory. Recurrent otitis externa, head shaking and scratching, odor, facial pyotraumatic lesions, aural hematoma, pain on opening mouth, reluctance to chew hard food or toys, yelping or avoiding petting on the head or ears, head tilt, behavioral changes (irritability, hiding), depression, loss of hearing, stridor.
Physical examination. Pain not pruritus common in gram-negative otitis externa/media. Pain on palpation/manipulation of pinna or canal, ulcerative lesions in canal, resisting having mouth opened, frantic head shaking, malodor, exudate in external canal or "fluid sound" when palpated, thickened canals/palpable obstructive soft tissue/calcification of ear canal, head tilt. Otitis media can be "silent;" with only presenting sign being a head tilt.
Diagnosis

Definitive diagnosis. Based on history, clinical signs, physical findings. Cytology may reveal neutrophilic exudate with/without rods. Bacterial culture isolates Pseudomonas. Otoscopic exam may reveal ruptured/defective tympanic membrane (TM) and is diagnostic for otitis media. Intact TM does not rule out otitis media.
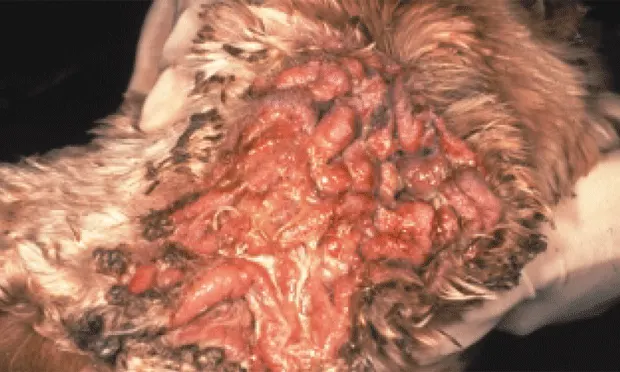
End-stage ear disease in a dog with primary seborrhea. Note the severe proliferation on inner pinna, opening to ear canal, and surrounding skin. Ear pinna and canal were calcified.
Diagnostic imaging. Radiographs/computed tomography (CT) can be used to diagnose otitis media. Fluid/soft tissue density/bone changes in bullae, soft tissue in external canal compatible with proliferative otitis or soft tissue mass, calcification of bullae/external ear cartilage (i.e., "end-stage ear disease") or soft tissue all suggest otitis media. Large retrospective studies comparing sensitivity/specificity/cost-benefit ratio of these tests in early/chronic otitis media are lacking. In the most widely cited study comparing CT and radiography, 14 dogs with chronic otitis underwent CT and radiographic scans before surgery.4 Twenty seven bullae were surgically explored; 18 were abnormal, and 9 were normal. CT correctly identified 15/18 bullae and radiographs identified 12/18 bullae. All (9/9) normal bullae were identified by radiographs and 8/9 normal bullae were correctly identified via CT. Neither modality detected early otitis media without osseous changes. CT was more sensitive than radiographs in this study, but authors concluded the relative value of the two was similar and the data did not justify routine CT to screen for otitis media.
Laboratory FindingsBacterial isolates reveal Pseudomonas. Concurrent infections with yeast (Malassezia), cocci (Staphylococcus or Streptococcus), or other rods (Escherichia coli or Proteus, Pseudomonas, Klebsiella, and Bacillus species) may be found. Optimum therapy based on cytology studies and culture of external ear canal/tympanic bulla specimens.
Treatment
Medical management. Sedation or general anesthesia is required for deep ear cleaning. Use copious warm sterile saline for lavage of external ear canal and surgical suction to remove debris/exudate. Ear canal/tympanic membrane should be repeatedly examined during process. Perform myringotomy to remove exudate. After myringotomy, instill enrofloxacin-dimethyl sulfoxide-fluocinolone solution into tympanic bulla to decrease inflammation/deliver high concentrations of fluoroquinolone. Systemic antimicrobial treatment may be needed for minimum 8 to 12 weeks. Give oral prednisone to decrease inflammation, exudation, and stenosis. These steps provide significant pain relief. Repeated myringotomy or ear lavage may be necessary during this period. Start concurrent topical therapy once pain has subsided (see Tx at a Glance).
Surgical management. Myringotomy helps resolve otitis media; exudate from tympanic bulla (TB) is drained via small stab incision between 5 and 7 o'clock in tympanic membrane, and TB is flushed with warm sterile saline. Immediate surgical indications include severe calcification of canals on palpation/radiographs ("end-stage ears"), obstruction by soft tissue mass/proliferative otitis unresponsive to glucocorticoids, no response to aggressive medical management. Radiographs or CT should be done before surgery to determine need for total ear canal ablation/bulla osteotomy.
Medications
Systemic therapy. Administer maximum dose antibiotics for 4 to 8 weeks; chronic cases may need >12 weeks to resolve. Cytology/culture may indicate need for concurrent systemic antifungal for 30 days. Give concurrent oral prednisone 1 mg/kg sid for 15 days; then 1 mg/kg every other day for 15 days. Prednisone is important to treatment regimen, as it decreases inflammation/secretions and reduces pain.
Topical therapy. Begin topical therapy once pain has subsided. Clean ears daily. Instill Tris buffered EDTA 2 to 3 ml/ear 5 min before use of topical antimicrobial. Apply concurrent topical antimicrobial twice daily. Do not use aminoglycoside if tympanic membrane is ruptured. Do not use silver sulfadiazine in conjunction with Tris buffered EDTA as EDTA inactivates silver sulfadiazine.
For pain. Give butorphanol 0.3 to 0.6 mg/kg IM 20 min before ear lavage. Give butorphanol 0.5 mg/kg PO sid to bid for first 5 to 7 days in severe cases; owners should administer 20 min before manipulating ear. Avoid aspirin or nonsteroidal analgesics in patients receiving glucocorticoids. Fentanyl patch is an option. Analgesics can usually be discontinued once patient is eating and/or owner can manipulate the ear canal. It is important that glucocorticoids be continued as they provide best long-term pain relief during initial treatment. Butorphanol is short-acting and meant for pain management during and immediately after manipulating ear.
Follow-Up
Monitor every 2 to 4 weeks. Therapy in improving patients should continue for total of 8 to 12 weeks. Relapse may indicate resistance to antibiotics; bacterial culture should be repeated. Patients with chronic/recurrent disease should be evaluated for underlying condition.
In General
Relative Cost*(severe Pseudomonas infection; chronic otitis media with stenosis of ear canal)Initial evaluation: $1000 to $1200: Office call, in-house cytologic studies, bilateral ear cultures, preanesthetic blood work, sedation/general anesthesia, myringotomy and middle ear irrigation, CT, 1 to 2 days hospitalization, medications, topical therapy, and pain medication for 10-kg dog.
At-home management for 8 to 12 weeks: additional $600 to $800 Systemic antibiotics, topical medications.
Medical management (chronic cases): additional $500 to $800: All of above plus general anesthesia, repeated myringotomy, and antimicrobial therapy for additional 6 to 8 weeks. Surgical cost for total ear canal ablation: $1000 to $1800 per earPreoperative assessment, general anesthesia, CT, surgical procedure, biopsy, culture of exudate, postoperative intensive care, pain medication, postoperative care and medications.
PrognosisVariable depending on severity, sensitivity of organism, extent of soft tissue/bone involvement. Inadequate systemic therapy, subtherapeutic doses of antibiotics, failure to remove exudate from tympanic bulla, and lack of concurrent compatible topical therapy are most common reasons for failure. Total ear canal ablation is associated with good to excellent prognosis for resolving chronic infection.
Future ConsiderationsAnticipate studies comparing serum vs. tissue concentrations of fluoroquinolone antibiotics for treating otitis media. In addition, anticipate prospective and retrospective studies comparing the diagnostic and cost-benefit ratios of radiography, CT, and magnetic resonance imaging.
KEY POINTS: CAUSES OF GRAM-NEGATIVE OTITIS
Some aspect of all causes (primary, predisposing, perpetuating) may be at play.
Any condition altering anatomy/ physiology of canal can lead to otitis externa/media.
High cerumen production, moisture, humidity, temperature; decreased/failed epithelial migration; obstructive lesions; microbial overgrowth are essential "root pathophysiology" of all cases, regardless of underlying cause.
Most common "triggers" of acute suppurative otitis externa in 550 dogs were otic foreign body, grooming, bathing.2 A study of 752 dogs with otitis revealed unilateral, painful, suppurative otitis is often not associated with identifiable underlying skin disease.3
"Trigger" of chronic unilateral Pseudomonas infection often is transient, although otitis may persist due to inadequate treatment.
KEY POINTS: DIAGNOSIS
Early cases of otitis media may not be detected by imaging.
Imaging can miss 17% to 33% of otitis media compared with surgical diagnosis; fewer cases missed with CT.
Advantage of CT is ability to take sequential images and digitally remove extraneous structures, allowing visualization of inner/middle ear.
CT not specific for particular disease but useful in confirming location/extent of lesion, providing anatomic information for surgery/biopsy sites.
Surgery may ultimately be required for diagnosis.
TX ... at a glance
Ear Cleaning
Sedation or general anesthesia
IM butorphanol 0.3-0.6 mg/kg 20 min before lavage/myringotomy
Collect cytologic and bacterial cultures
If ceruminolytic agent is used, copiously flush ear
Lavage ear canal with warm sterile saline; suction fluid/debris
Perform myringotomy
Collect cytologic/culture specimens from tympanic bulla
Flush bulla with copious saline (> 200 ml)
Instill bulla with 1-2 ml of 1 ml enrofloxacin injectable and 8 ml dimethyl sulfoxide-fluocinolone
Adjuvant Topical Therapy
Any topical agent is potentially ototoxic!
Premedicate with butorphanol 0.5 mg/kg, 20 min before home cleaning; clean ears daily
Instill 2-3 ml Tris buffered EDTA into ears after cleaning and 5 min before topical therapy
Apply topical product with known spectrum of activity against Pseudomonas (e.g., enrofloxacin, polymixin B, silver sulfadiazine, ticarcillin, marbofloxacin, ciprofloxacin) twice daily
Do not use aminoglycoside-containing products if TM ruptured; pending healing use 1:10 dilution silver sulfadiazine (1-2 ml/ear bid)
Do not use Tris buffered EDTA in combination with silver sulfadiazine
Systemic Therapy
Should be based on results of culture/sensitivity tests; maximum dose therapy (e.g., enrofloxacin 20 mg/kg PO sid, marbofloxacin 5.5 mg/kg PO sid, ciprofloxacin 20 mg/kg PO sid). (Note: In vitro sensitivity may show resistance; however, these doses can exceed the MIC but require 10-12 weeks of treatment)
Ketoconazole or itraconazole 5-10 mg/kg PO sid for 30 d if yeast seen on cytology/culture
Prednisone 1 mg/kg PO sid for 15 d and then every other day for 15 d
Patient Monitoring
Examine every 2-4 wk; every 2 wk optimum
Repeat bacterial cultures/ myringotomy as needed
Monitor patient for concurrent yeast/staphylococcal infections; treat appropriate to cytologic/ culture results
Watch for contact reactions and overaggressive cleaning by clients
Lack of response after 8-12 wk aggressive therapy: consider total ear canal ablation/bulla osteotomy