Overview Understanding of Prostatic Disease
Autumn P. Davidson, DVM, MS, DACVIM, University of California, Davis
Profile
Definition
Prostatic disease is the most common disease of the male reproductive tract.
Diseases of the prostate include benign prostatic hyperplasia (BPH), cystic benign prostatic hyperplasia (CBPH), infectious prostatitis (IP), and prostatic neoplasia (PN).
Differentiating the prostatic conditions and determining whether conditions are benign or malignant can be clinically challenging.
Using multiple diagnostic modalities and serial evaluations can be helpful.
Signalment & Risk Factors
Prostatic disease is common in dogs but rare in cats.
BPH, CBPH, and IP are more common in intact dogs.
PN is more common in castrated dogs and typically affects dogs >10 years of age.
Causes
BPH occurs predictably in intact dogs >5 years of age because of the effect of androgen dihydrotestosterone on the prostatic parenchyma.
CBPH (hyperplasia with parenchymal cysts) occurs variably as dogs age.
IP occurs secondary to colonization of the normally sterile prostate, usually by an opportunistic organism (eg, Escherichia coli).
PN originates from basal cell (ductal or uroepithelial) lines and is not androgen mediated in dogs.
Pathophysiology
Dihydrotestosterone can cause symmetric, progressive, eccentric prostatic parenchymal hyperplasia, which can become cystic (CBPH).
The most common route of infection in IP is thought to be ascension of urethral flora, but hematogenous infection is possible.
Organisms most commonly isolated from an infected prostate are E coli and Staphylococcus, Streptococcus, and Mycoplasma spp.
Occasionally, Proteus and Pseudomonas spp or anaerobic organisms are isolated.
Mycotic prostatitis is uncommon and usually limited to endemic regions.
Acute infectious prostatitis (IP) is a serious disorder that can lead to sepsis and death.
Malignant transformation of prostate basal cell lines can cause PN.
Signs
Prostatic Hyperplasia
BPH and CBPH can occur with or without clinical signs.
Because prostatic enlargement in BPH patients is eccentric, urethral compression is unlikely in dogs.
Tenesmus secondary to colonic compression from prostatomegaly can be seen with advanced BPH.
The most common signs of BPH and CBPH are blood dripping from the urethra, hemospermia, and hematuria.
The prostate will not be painful on palpation but is usually prominent.
Fertility is not impaired, but attempts at cryopreservation can be compromised, as the presence of hemoglobin increases sperm cell membrane fragility during the freeze-and-thaw processes.
Compromised urine outflow, prostatic pain, or deterioration of semen quality should prompt closer evaluation for more serious prostatic disorders (eg, IP, PN).
Infectious Prostatitis
Bacterial infection of the prostate can be acute and fulminant or chronic and progressive. Prostatic abscessation can occur.
Dogs are typically febrile, anorexic, and lethargic.
Prostate evaluation is indicated in intact dogs presenting with these signs.
Ejaculation can be painful, and affected dogs may be reluctant to breed.
The prostate will be painful on palpation; sublumbar lymphadenomegaly can be present.
Recurrent urinary tract infection may imply chronic septic prostatitis in intact dogs.
Chronic septic prostatitis can also have minimal signs, with only deterioration of semen quality evident.
The prostate may be painful, firm, and irregular on palpation.
Prostatic Neoplasia
PN can cause chronic lumbosacral or abdominal pain, tenesmus, dysuria, and weakness.
PN is usually diagnosed late in its course, with local metastasis (sublumbar lymph nodes) already present.
Diagnosis
Definitive Diagnosis
Definitive diagnosis of any prostatic disorder requires histopathologic evaluation of prostatic tissue, but less invasive diagnostics may help differentiate the prostatic disorders.
Most useful are physical examination findings; abdominal ultrasonography; and laboratory studies of urine, semen, prostatic fluid, or prostatic tissue.

Typical ultrasonographic finding with BPH. Transverse image (ventral at top of image) of an intact canine prostate with multiple wagon-wheel striations radiating from the urethra to the capsule.
Prostatic Hyperplasia
Characteristic appearance of BPH and CBPH on ultrasonography includes symmetric parenchymal striation with increased echogenicity and variable hypoechoic-to-anechoic intraparenchymal cystic structures (Figures 1 and 2).
Other than the appearance of hemospermia, semen quality is unaffected.
Cytology of a prostatic fine-needle aspirate, prostatic cyst aspirate, or prostatic biopsy specimen for histopathology can help confirm diagnosis if ultrasonography is not characteristic.

CBPH sagittal view (ventral is top of image, cranial is left) of a canine prostate with small anechoic parenchymal cysts.
Infectious Prostatitis
Septic prostatitis is best diagnosed by abdominal ultrasonography with guided fine-needle aspirates for cytologic examination and culture, giving specific attention to cystic structures within the parenchyma.
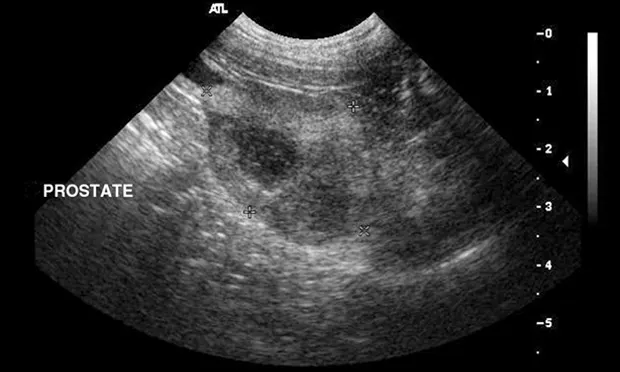
Ultrasonographic findings are nonspecific but typically will be of mixed echotexture with hyperechoic areas reflecting fibrosis (Figure 3).
Diagnosis of chronic septic prostatitis requires cytologic and microbiologic examination of urine and prostatic tissue.
Culture of the prostatic fluid or third portion of ejaculate can be problematic.
Dogs with prostatic pain may be reluctant to ejaculate.
Contamination of the ejaculate with normal urethral flora can occur during ejaculation.
Examination of semen will typically reveal suppurative inflammation, hemospermia, necrospermia, and decreased volume.
Because prostatic fluid normally refluxes into the urinary bladder, urinary tract infection is usually present in IP patients.
Pyuria and bacteriuria should always prompt evaluation of the prostate in any intact dog, as IP can occur with septic orchitis and epididymitis.

Prostatitis with abscess. Sagittal view of an intact canine prostate (cursors); a hypoechoic nodule is visible within the parenchyma. The parenchymal echo texture is mixed.
Prostatic Neoplasia
Diagnosis of PN can be supported by intraprostatic mineralization and complex parenchymal changes on ultrasonography (Figure 4).
Prostatic fine-needle aspiration or biopsy can be confirmatory.
Concern about seeding the abdomen during transabdominal tissue sampling of prostatic neoplasia is valid but less problematic than with urinary bladder neoplasia.
Malignancies of the prostate have a poorer prognosis as compared with malignancies of the urinary bladder.
Multiple prostatic pathologies can be present in any patient (Figure 5).

Sagittal view of a prostate in a castrated dog. Prostatic mineralization suggests neoplasia.

Prostatic adenocarcinoma. Sagittal image of an intact canine prostate showing characteristic BPH striations ventrally, but hypoechoic nodules (cursors) present within the dorsal parenchyma. Nonhomogenous prostatic parenchymal appearance should prompt evaluation with a biopsy.
Treatment
Prostatic Hyperplasia
Castration is curative in both BPH and CBPH patients.
Antiandrogen Therapy
In breeding dogs, medical antiandrogen therapy is an option if defecation is difficult.
Alternatively, medical antiandrogen therapy can be used until semen cryopreservation can be accomplished, after which castration can be curative.
Antiandrogen therapy using the 5α-reductase inhibitor finasteride is a potentially effective option.
Conversion of testosterone to dihydrotestosterone can be inhibited in the prostate, causing reduction in prostatic and parenchymal cyst size beginning in 1–8 weeks.
The canine antiandrogen dose can be extrapolated from the human dose of finasteride; 1.25–5 mg/dog PO q24h; higher doses (0.10–0.20 mg/kg PO q24h) have been evaluated without problems.
Libido and semen quality are not compromised, but the prostatic fluid component of the ejaculate is markedly diminished.
The presence of intraparenchymal cysts in CBPH patients might increase the potential for prostatic abscessation and can be an indication for antiandrogen therapy.
Other Medical Therapies
Alternative medical therapies (eg, estrogenic or progestational compounds) are not advised because of their negative effects on circulating testosterone concentration and spermatogenesis and induction of prostatic metaplasia (estrogen), potential for myelosuppression (estrogen), insulin and glucose dysregulation (progesterone), and mammary neoplasia (estrogen).
Finasteride is not licensed for use in dogs but is commonly used in specialty reproductive practice.
Infectious Prostatitis
Treatment must be prompt and aggressive.
Fluid therapy is necessary to correct dehydration and shock.
Large prostatic abscesses are treated most effectively by surgical drainage and omentalization.
Abscesses may also be drained by fine-needle aspiration under ultrasound guidance.
Acute Infectious Prostatitis
Pending the results of culture and susceptibility testing, treatment with a fluoroquinolone and potentiated amoxicillin should be initiated.
Antibiotic penetration in acute IP patients is not as problematic as in patients with a normal prostate; in acute IP, inflammation alters the blood–prostate barrier, allowing most antibiotics to penetrate.
A negative culture of urine or prostatic fluid should be obtained after therapy has been initiated to confirm effectiveness.
Antibiotic treatment for acute prostatitis should be continued for ≥4 weeks.
Urine or prostatic fluid should be recultured 1 week after antibiotic therapy is discontinued and again 2–4 weeks later to confirm infection has resolved.
Castration should be considered.
Medical testosterone reduction with finasteride is an acceptable alternative if the dog stabilizes rapidly and is to be used for breeding.
Chronic Infectious Prostatitis
Chronic IP may be difficult to clear, because the blood–prostate barrier is quite effective in preventing many drugs from penetrating into the prostatic parenchyma.
In patients with chronic IP, only highly lipophilic agents (eg, erythromycin, clindamycin, trimethoprim–sulfonamide, chloramphenicol, carbenicillin, enrofloxacin, ciprofloxacin) can cross into the prostate.
Antibiotic therapy should be based on culture and susceptibility results from urine and prostatic tissue.
Treatment should be continued for ≥4 weeks.
To identify resistance to antibiotics or persistent infection, cultures should be repeated during and for several months after antibiotic therapy is discontinued.
Castration improves the response to treatment of chronic bacterial prostatitis.
Surgical castration may be postponed until urine or prostatic culture is negative while the patient is receiving antibiotic therapy to avoid creating a sequestration of infectious material in an involuting gland.
Prostatic Neoplasia
PN is not responsive to antiandrogen therapy.
Prostatectomy is complicated by urinary incontinence and is rarely curative because of local metastatic disease.
Chemotherapy of various prostatic tumors can be palliative; consultation with an oncologist is advised once a histopathologic diagnosis with staging is obtained.
Efficacy of COX-2 inhibition with piroxicam at 0.3 mg/kg PO q24h when used with gastric protectant misoprostol at 1–3 µg/kg PO q8h or IV chemotherapy (eg, doxorubicin, mitoxantrone, carboplatin) has not been determined.
Palliative radiotherapy can provide short-term relief of obstructive disease.
In General
Prognoses can be:
BPH: good for fertility, benign
CBPH: good for fertility, benign unless secondary infection occurs
IP: guarded to fair for fertility if managed aggressively
Prostatic neoplasia: poor for fertility, a malignant disease
Cost of palliative radiation: $$$$–$$$$$
Cost Key
$ = up to $100
$$ = $101–$250
$$$ = $251–$500
$$$$ = $501–$1000
$$$$$ = more than $1000
Editor's note: This article was originally published in January 2014 as "Prostatic Disease"