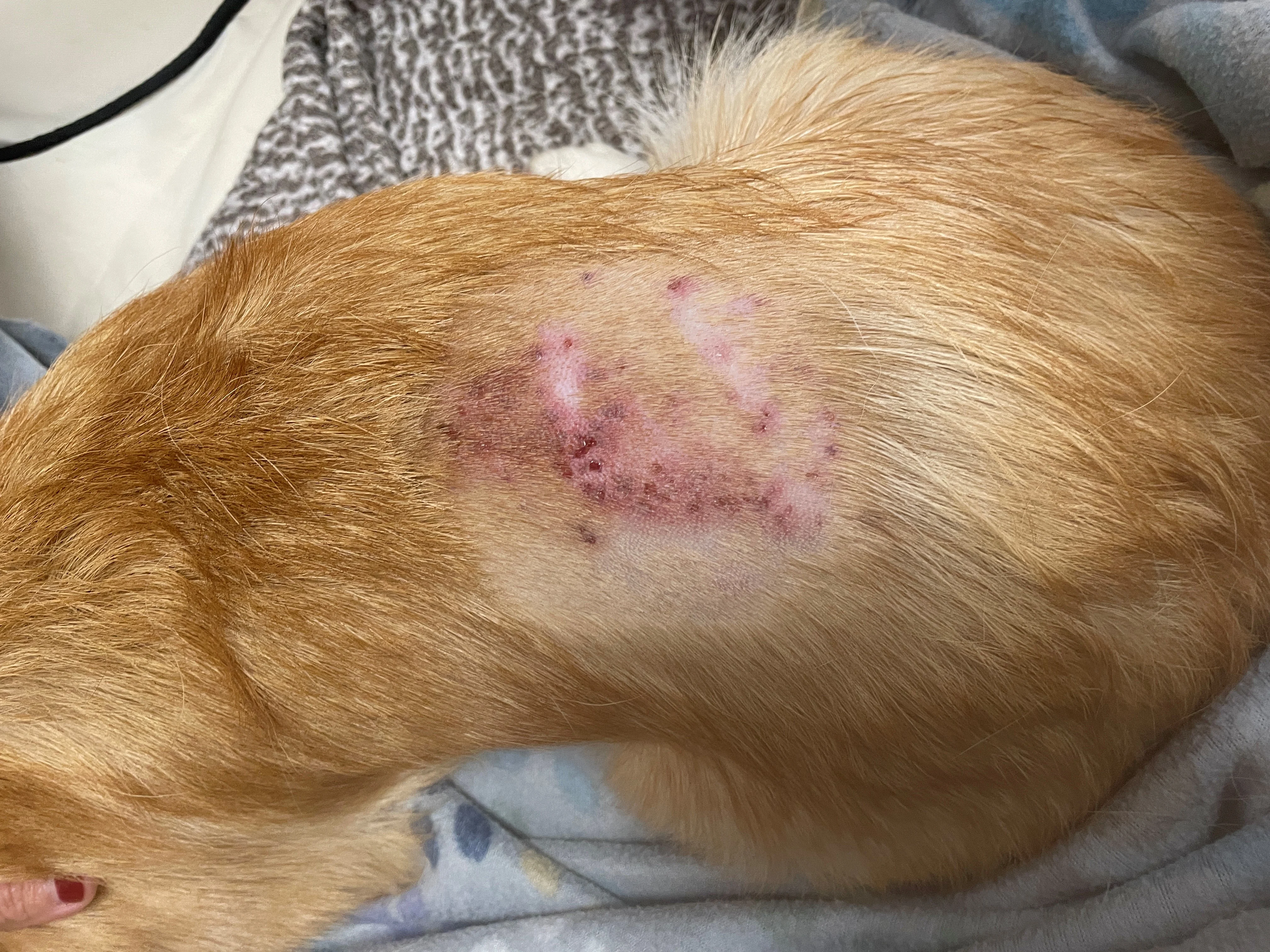
Inflamed skin with multiple draining tracts along the dorsum
Ella, a 13-month-old intact female Pembroke Welsh corgi, was presented for a 3-day history of progressive lethargy and decreased appetite. Four days prior to presentation, Ella was started on fish oil supplements for excessive shedding and had been groomed and bathed at a self-service dog wash facility, where the shampoos and conditioners were diluted with tap water.
Physical Examination
Ella appeared anxious on physical examination. She had mild hyperthermia (103.1°F [39.5°C]), intermittent tachycardia (>120 bpm) during handling, copious shedding, and scattered papules, pustules, nodules, and erythema on her ventrum. Thoracic auscultation and other vital parameters were within normal limits. She had no neurologic deficits but exhibited severe pain on palpation and manipulation of the neck, as well as moderate pain on palpation of the thoracic and lumbar spine.
Differential Diagnosis
The presumed diagnosis based on Ella's age, fever, and severe neck pain was acute steroid-responsive meningitis-arteritis, an immune-mediated inflammation of the meninges and associated arteries typically seen in dogs 6 to 18 months of age.1,2 Diagnosis was based on clinical signs of pyrexia, lethargy, profound cervical pain, and hyperesthesia along the vertebral column.
A CSF tap was planned; increased protein concentration and marked neutrophilic pleocytosis in the CSF would support the presumed diagnosis.1,2 Hydromorphone (0.05 mg/kg IM) and medetomidine-vatinoxan hydrochloride (0.2 mg medetomidine/m2 IM) were administered in preparation for the CSF tap. Anesthesia was induced with propofol (2.2 mg/kg IV) and maintained with isoflurane in oxygen. With the dog under anesthesia, the skin was examined more closely, and scabs were noted on the dorsal midline of the midlumbar region. The hair was clipped, and severe erythema and draining tracts were noted on the skin (Figure 1). A dermatology consult was requested. Postgrooming furunculosis was suspected based on fever, pain, characteristic skin lesions, and recent history of grooming.
Inflamed skin with multiple draining tracts along the dorsum
Diagnostics
Impression smears for cytology and swabs for bacterial culture were collected from draining tracts on the back and papules and pustules on the inner thighs. Ella was reactive during skin sample collection despite administration of analgesic medication, suggesting pain associated with furunculosis. Cytology confirmed pyogranulomatous inflammation with eosinophils and rare rod-shaped bacteria consistent with postgrooming furunculosis.3 Bacterial culture revealed a moderate number of Pseudomonas aeruginosa colonies susceptible to amikacin, ceftazidime, gentamicin, imipenem, and piperacillin/tazobactam. Minimum inhibitory concentrations for marbofloxacin and enrofloxacin were both reported as 0.5 µg/mL; however, susceptibility could not be interpreted because of a lack of available canine standards for skin and soft tissue infections with P aeruginosa. Break point susceptibilities may vary with species and infection location.4 In cats, the minimum inhibitory concentration for P aeruginosa soft tissue infections susceptible to enrofloxacin is ≤0.5 µg/mL.4
CBC and serum chemistry profile revealed leukocytosis with a mature neutrophilia, lymphocytosis, monocytosis, hypoalbuminemia, hypocalcemia, hypochloremia, increased C-reactive protein, and decreased iron (Table). Rare, granulated lymphocytes and mild echinocytosis were noted. Clinical pathology abnormalities were attributed to skin infection and inflammation.
Table: Selected Abnormal Values From CBC & Serum Chemistry Profile Results
Postgrooming furunculosis was confirmed.
Diagnosis: Postgrooming Furunculosis
Treatment & Management
Treatment of postgrooming furunculosis should consist of ≥4 weeks of systemic antibiotics.3,5 When rods are present, an oral fluoroquinolone is typically initiated while culture and susceptibility results are pending.3,5 If cocci are present, clindamycin or cephalexin may be a better first-line option. Depending on severity and type of clinical signs, affected patients may also require analgesics, anti-inflammatory drugs, topical antimicrobial drugs, and/or medicated shampoos.3
Marbofloxacin (5 mg/kg PO every 24 hours for 4 weeks) was administered in conjunction with prednisone (0.9 mg/kg PO every 24 hours for 7 days, then every 48 hours for 10 days) due to the severity of inflammation and discomfort. Response to marbofloxacin was considered favorable, with lesions dramatically improved at rechecks 1 and 3 days after treatment was initiated. Because of the concurrent prednisone administration, analgesia was provided with acetaminophen (6.8 mg/kg PO)/codeine (1.4 mg/kg PO) and gabapentin (9.1 mg/kg PO) every 8 to 12 hours as needed. Patients not receiving glucocorticoids can be treated with NSAIDs. Topical treatments were not recommended due to signs of severe pain with manipulation. The owner discarded all of the dog's bathing and grooming products in case of possible contamination and source of skin trauma, respectively.
Treatment at a Glance
Oral analgesic medication should be provided as needed.
An oral antimicrobial should be chosen based on cytology. Final drug selection should be based on culture and susceptibility results and response to treatment.
Topical treatments should be avoided while the patient is painful.
Open grooming products and paraphernalia should be discarded.
Prognosis & Outcome
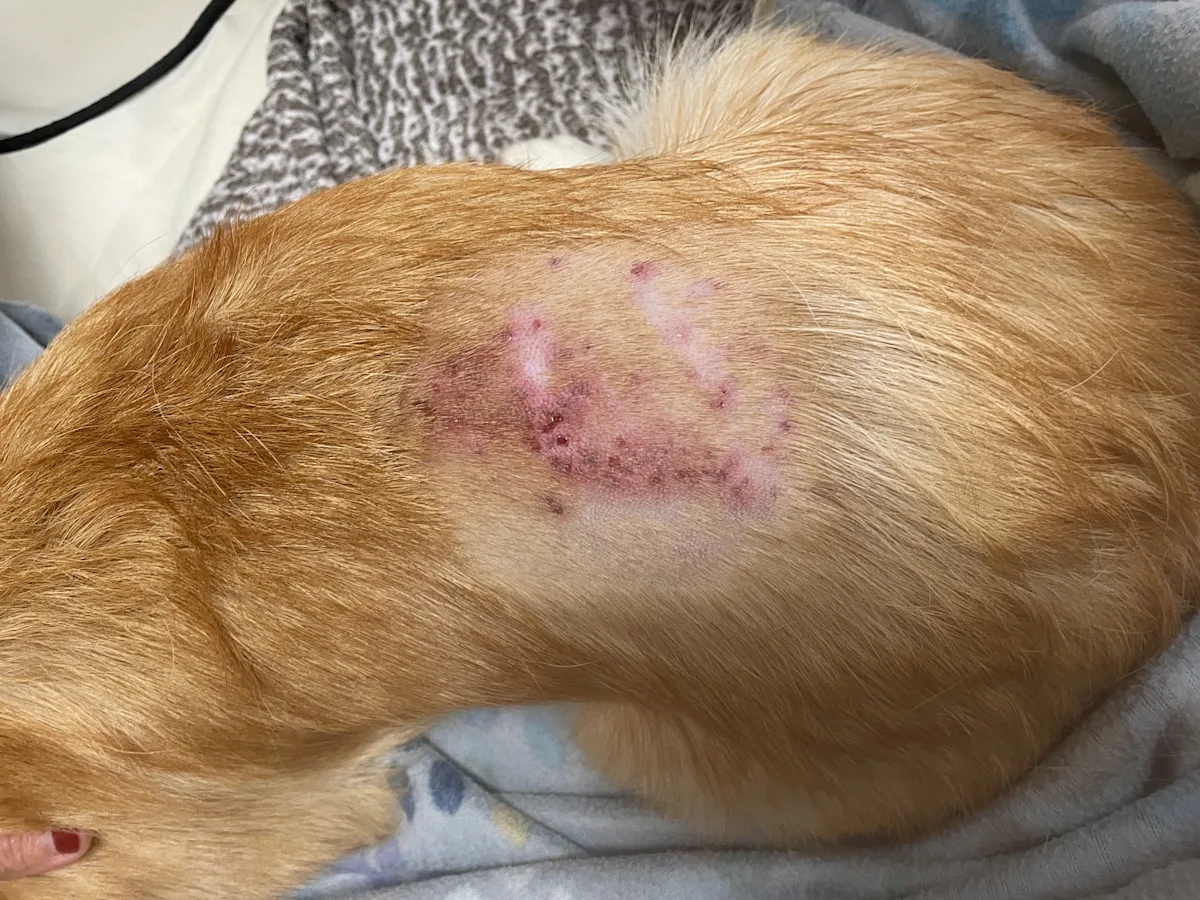
Ella appeared more comfortable, skin erythema dramatically decreased, and drainage from dorsal lesions stopped within 24 hours of initiation of treatment. Behavior and appetite began to improve after 3 days. Draining tracts improved and Ella appeared more energetic after one week (Figure 2). Behavior and appetite returned to normal and skin lesions were healed after 2 weeks (Figure 3).

Resolved inflammation and healing of skin lesions one week after initiation of treatment

Ella 2 weeks after initiation of treatment
Discussion
Postgrooming furunculosis is a subgroup of deep pyoderma that typically occurs 24 to 72 hours after bathing or grooming and is acute, fulminant, and markedly painful.3,5-7 Severe pain may be present along the neck or back and can be mistaken for neurologic disease. Erythematous, nodular, or draining skin lesions along the dorsal midline not initially visible through a thick haircoat may also be present.3,5,6 Diagnosis is usually based on patient history, clinical signs, and evidence of pyogranulomatous inflammation (with or without eosinophils and bacteria) on cytology or histology.3,7 Culture of skin lesions is recommended. P aeruginosa is most commonly isolated, but Klebsiella spp, Staphylococcus spp, Serratia spp, and Burkholderia spp infections have also been reported.5
Postgrooming furunculosis is uncommon or possibly underreported, and breeds with short, thick, and firm haircoats may be predisposed.5,7,8 The condition is suspected to result from mechanical trauma to hair follicles during vigorous grooming; subsequent bathing with contaminated water or bath products can result in inflammation and infection.3,6 Condition severity has been associated with degree of trauma (eg, plucking out hair [ie, stripping], which causes greater injury to hair follicles than routine grooming).5,7,8 Likelihood of contamination of bathing products in self-service bathing facilities is the same as shampoo bottles in the home but is more common when bathing products have been diluted with tap water.7,8
Dogs with postgrooming furunculosis can develop erythema, swelling, pustules, papules, hemorrhagic bullae, and/or furuncles that may ulcerate and drain.3,5,7 The site typically affected first and most severely is the dorsal midline, with erythema and pinpoint, painful draining tracts.3 Systemic signs include lethargy, decreased appetite, fever, and intense pain on palpation of affected areas.5 Depending on the severity and extent of skin lesions, patients can become septic due to delayed medical intervention.9
Until susceptibility results are available for dogs with furunculosis, empirical treatment with marbofloxacin (2.75-5.5 mg/kg PO every 24 hours) or enrofloxacin (10-20 mg/kg PO every 24 hours) should be initiated if rods are present on cytology, and cephalexin (15-30 mg/kg PO every 12 hours) or clindamycin (5.5-10 mg/kg PO every 12 hours) should be started empirically if cocci are present. Recheck within the first 3 to 7 days of treatment is recommended to confirm response to treatment, particularly because P aeruginosa isolates can become resistant to antimicrobials within 3 to 4 days.10 Multispecies bacterial infections have been reported.3 Clipping of the fur and topical treatments may exacerbate pain and/or skin trauma.5
Most dogs with postgrooming furunculosis show improvement in behavior, appetite, and fever within 48 hours of administration of antimicrobials. Prognosis is typically excellent unless sepsis develops.3,10 Open grooming products and used paraphernalia should be discarded and a gentler brushing technique used.
Prevention includes gentle grooming and avoidance of contaminated products and contact with stagnant or nonchlorinated water.3,5,6 Grooming products should not be diluted with tap water, as this may be a risk factor for contamination with Pseudomonas spp. A recent study reported significant association between Pseudomonas spp contamination and dilution of shampoos and conditioners.8
Take-Home Messages
Severe pain, lethargy, and appetite loss 24 to 48 hours after grooming, plucking out hair (ie, stripping), or bathing may signal postgrooming furunculosis.
Initial skin lesions on affected dogs are most commonly erythematous and painful, with pinpoint draining tracts along the dorsal midline.
Infection is most commonly caused by P aeruginosa; however, culture and susceptibility testing are recommended.
Initial treatment in patients with Pseudomonas spp or another gram-negative bacterial species infection suspected based on cytology can include a systemic fluoroquinolone (pending culture and susceptibility results) and analgesics. Response should be seen within 24 to 48 hours.
Severely affected dogs may develop sepsis; therefore, this condition can be a true dermatologic emergency.
Grooming products should never be diluted with stagnant or nonchlorinated water. Used or potentially contaminated products should be discarded following diagnosis of postgrooming furunculosis.
Listen to The Podcast
Dr. Tobias joined the podcast to dig deeper into this case and offer tips for diagnosis and treatment.