Postanesthesia Regurgitation in a Dog
A 13-year-old spayed female Labrador retriever was presented for evaluation of persistent regurgitation.
History
The dog was previously healthy, with no history of gastrointestinal illness. She had undergone routine periodontal treatment and multiple dermal mass excisions while under general anesthesia and upon discharge was prescribed deracoxib, clindamycin, and metronidazole.
Within a few days, she began having multiple episodes of regurgitation per day. She lost 9 pounds in the 3 weeks after the procedures and could not hold down food or water despite having a good appetite and no evidence of dysphagia.
Physical Examination
Routine physical examination revealed nuclear sclerosis in both eyes, a grade 3/6 left systolic murmur, and a body condition score of 4/9.
Figure 1. Lateral cervical radiograph showing a focal area of proximal esophageal dilation (arrow).
Diagnostics
Two-view thoracic radiographs revealed a focal area of proximal esophageal dilation (Figure 1).
ASK YOURSELF...
What typical clinical signs can you use to differentiate regurgitation from true vomiting?
What are the differential diagnoses consistent with this patient's signs and radiographic findings?
What diagnostic test(s) would provide the best information?
What are some potential treatment options for your differential diagnoses?
Diagnosis:
Proximal esophageal stricture, possibly secondary to either esophagitis caused by gastric acid reflux while under general anesthesia or pill-induced inflammation.
Figure 2. Esophagram revealing narrowing of the esophageal diameter at the level of C2, with esophageal dilation cranial to the narrowed area.
Further Diagnostics
Barium contrast esophagraphy under fluoroscopy was performed: The patient was placed in right lateral recumbency and barium sulfate was administered orally. Swallowing was normal with liquid barium. An abrupt narrowing of the esophageal diameter was seen at the level of C2, with esophageal dilation cranial to the narrowed area (Figure 2). No abnormalities were noted in the mid or caudal esophagus.
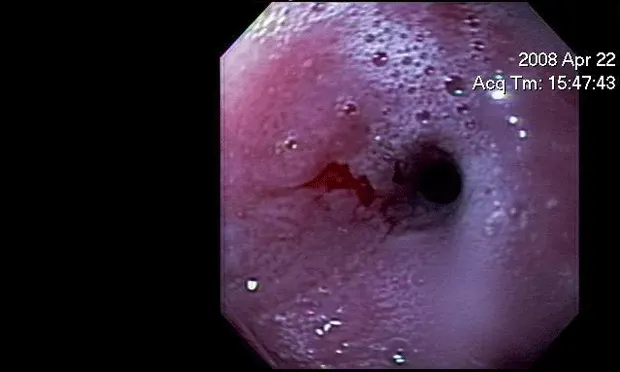
Esophagoscopy was then performed by using a 9.5-mm flexible video gastroscope. There was a focal esophageal stricture approximately 10 cm caudal to the upper esophageal sphincter (Figure 3). The esophageal diameter at the level of the stricture was 5 mm, and the endoscope could not be passed further.
Figure 3. Esophageal stricture before balloon dilatation
The surrounding esophageal mucosa was markedly thickened and irregular, and multiple partial-thickness biopsy specimens were procured. Histopathologic findings were consistent with severe ulcerative neutrophilic and eosinophilic esophagitis.
Differential Diagnoses
Focal esophageal obstruction can be due to many causes, including intraluminal foreign bodies, intramural stricture formation, primary esophageal neoplasia, or periesophageal causes (eg, inflammation, hilar lymphadenopathy, adjacent neoplasia, severe cardiomegaly, or vascular ring anomalies).
Esophageal Strictures
These strictures result from abnormal production of fibrous tissue stimulated by the extension of esophageal erosions into the esophageal musculature. They are most commonly caused by reflux esophagitis (usually while the patient is under general anesthesia) and are less commonly due to esophageal foreign bodies. Strictures have also been reported after the administration of drugs, including tetracyclines, nonsteroidal antiinflammatory drugs, and aspirin. Usual clinical signs are persistent regurgitation with an excellent appetite.
Treatment
Treatment involves managing the underlying esophagitis and dilatation of the stricture. Esophagitis is managed by administering drugs (such as cisapride or metoclopramide) to increase lower esophageal tone and prevent further reflux; additional medications (such as a histamine H2-receptor antagonist or a proton-pump inhibitor) can be given to decrease gastric acid production in order to prevent further acid injury if reflux does occur.
Stricture dilatation is accomplished with balloon catheters or bougienage, generally guided by endoscopy (or, less commonly, fluoroscopy). Some patients require multiple dilatations to prevent recurrence. There is evidence that intramural injection of triamcinolone can minimize the incidence of subsequent strictures. Salvage procedures include the placement of an intraluminal stent or surgical resection.
Figure 4. Esophageal stricture after balloon dilatation. Note mucosal tear at the previous stricture site (arrow).
In this case, triamcinolone, a synthetic corticosteroid, was injected into the submucosal tissue at 4 sites around the stricture site. Using a guidewire, a 14-mm esophageal dilatation balloon was placed through the stricture. The balloon was inflated to 40 psi, and inflation was maintained for 1 minute. The balloon was then deflated, and the 9.5-mm video gastroscope could be passed through the stricture. There was a linear partial-thickness tear at the stricture site (Figure 4). A 20-French percutaneous endoscopic gastrostomy tube was then placed in the body of the stomach.
Outcome
The dog had 2 subsequent esophageal balloon dilatations to open the esophageal stricture to a diameter of 25 mm. Additional medical therapy included sucralfate (1 g PO Q 8 H) and omeprazole (20 mg PO Q 24 H) for approximately 5 weeks. The percutaneous endoscopic gastrostomy tube was removed approximately 1 month after placement. All clinical signs resolved and the dog is eating solid food, with no further regurgitation noted.
CAUTIONS
Barium aspiration is a potential complication of barium contrast esophagraphy; care should be taken to minimize this risk.
The esophagus can be a difficult area from which to obtain diagnostic biopsy samples and there is a risk of perforation, especially if the esophageal tissue is abnormal.
DID YOU ANSWER ...
Regurgitation is a passive process with few prodromal signs. It involves minimal abdominal effort and no repetitive abdominal contractions. True vomiting is the active ejection of gastric contents. It is associated with contractions of the abdominal and diaphragmatic muscles, and is usually preceded by signs of nausea, such as hypersalivation and retching. Both vomiting and regurgitation can occur immediately after eating or may not happen for several hours.
Megaesophagus, esophagitis, esophageal foreign body, esophageal neoplasia, stricture, diverticulum, vascular ring anomaly, hiatal hernias, esophageal motility disorder (rule out idiopathic disease, hypothyroidism, hypoadrenocorticism, lead toxicity, neuropathy, myopathy, junctionopathy).
Esophagraphy, (ideally imaged with fluoroscopy), esophagoscopy, and testing for myopathies or neuropathies (the latter 2 if a motility disorder is being considered)
Initially, esophageal balloon dilatation or bougienage, elevated feedings, and medical therapy for esophagitis. If treatment fails, consider esophageal stenting or surgical resection.