Pneumomediastinum: From Diagnosis to Prognosis
John Gagnepain, DVM, University of Florida
Gareth J. Buckley, VetMB, MRCVS, DACVECC, DECVECC, University of Florida
Pneumomediastinum is the presence of free gas in the mediastinum, which is the space between the pleural cavities that contains the trachea and mainstem bronchi, esophagus, heart, vena cavae, and aorta. Other smaller structures (eg, vagus nerve, lymph nodes, vessels of the head, thoracic duct) also run through this region.
Pneumomediastinum can be secondary to defects in the oropharynx, trachea, mainstem bronchi, lungs, esophagus, cervical fascial planes, or retroperitoneum. Trauma, infection, iatrogenic injuries (eg, intubation), migrating foreign bodies, emphysema, and neoplasia can lead to pneumomediastinum.1-4 Pneumomediastinum can subsequently progress to subcutaneous emphysema due to communication of the mediastinum with cervical fascial planes via the thoracic inlet.5
Clinical Signs
Patients with pneumomediastinum are typically presented for witnessed trauma, dyspnea, or subcutaneous emphysema. Increased lung sounds may be present on thoracic auscultation, or lung sounds may be quiet if concurrent pneumothorax is present. Trauma is a common cause of pneumomediastinum; therefore, a complete physical examination should be conducted and a thorough patient history (eg, recent anesthesia, especially in cats) obtained.
Diagnosis
A pneumomediastinum diagnosis is made via thoracic radiography (Figures 1 and 2). Air in the mediastinum outlines the cranial vena cava, dorsal and ventral tracheal walls, esophagus, and aorta. Gas may be present in the retroperitoneal space, cervical fascial planes, and subcutaneous space.2 If an obvious cause of pneumomediastinum is not apparent and the patient is stable, an oropharyngeal examination may be performed with the patient under sedation. Fluoroscopy with iodinated water-soluble contrast or endoscopy can be used to evaluate for esophageal lesions. Airway integrity may be assessed via endoscopy, although small lesions in the trachea may be missed. Advanced imaging (eg, CT) can be helpful in identifying the underlying lesion.

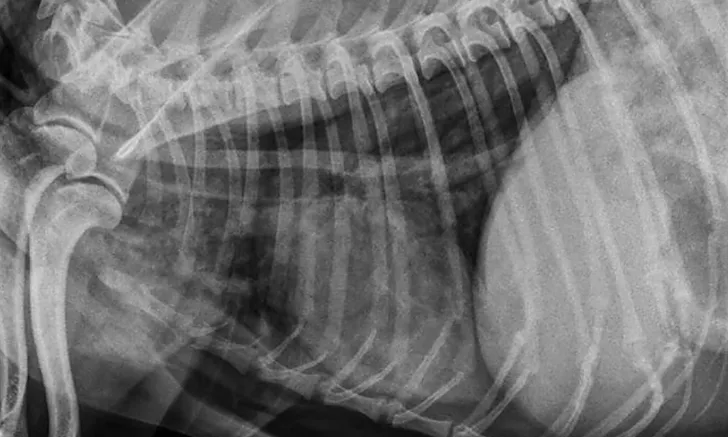
FIGURE 1
Ventrodorsal view of a patient with severe pneumomediastinum and severe subcutaneous emphysema secondary to a tracheal tear
Treatment
Strict cage rest and hospitalization to monitor for respiratory distress are recommended. Pneumomediastinum may progress to pneumothorax; in such cases, relieving pneumothorax via thoracocentesis is a priority.4 Thoracostomy tubes may be required in cases with significant recurrent pneumothorax. Subcutaneous emphysema should be aspirated only if it is causing discomfort. Analgesia should be provided for patients with trauma or other sources of pain. Oxygen therapy can speed up resolution of pneumomediastinum and subcutaneous emphysema by displacing nitrogen.
Prognosis
Many patients with pneumomediastinum recover over several (≤10-14) days as the defect heals and the air is resorbed. Exploratory surgery to repair tears is likely indicated in cases that progress despite conservative management, in which very large tears that are unlikely to heal on their own are identified, or in which obvious mediastinitis is present. In these patients, the prognosis is more guarded.5
Editor's note: This article was originally published in May 2017 as "Pneumomediastinum"