Placement of Central Venous Catheters
Matthew W. Beal, DVM, Diplomate ACVECC, Michigan State University
Vascular access serves as the lifeline to critically ill small animal patients, allowing for delivery of life-saving fluids, blood products, and drugs while simultaneously guiding the resuscitation effort by providing data on arterial and venous pressures.1, 2
Uses & Indications
By definition, the tip of a CVC terminates in the cranial or caudal vena cava. Most CVCs are placed in the cranial vena cava via the jugular vein; however, PICCs may be placed into the central circulation via a peripheral vein. Central venous catheters have many advantages over the more widely used over-the-needle peripheral venous catheters, including the ability to monitor CVP; infuse hyperosmolar or irritant solutions, such as total parenteral nutrition; and reliably and atraumatically retrieve diagnostic blood samples, as is often necessary in critically ill or diabetic patients.
To monitor CVP, the tip of the CVC should terminate in the thoracic vena cava of dogs and the thoracic or abdominal vena cava of cats.3 Many CVCs have multiple lumens, allowing delivery of several incompatible solutions concurrently or facilitating monitoring of CVP while several types of fluids are being administered. The author considers the multilumen CVC a key tool that facilitates both monitoring and management of critically ill dogs and cats.
Contraindications & Precautions
General contraindications to placement of a CVC via the jugular, maxillary, or femoral vein include presence of a significant hemostatic abnormality, such as severe thrombocytopenia (< 20,000/µl), known severe thrombocytopathia, coagulopathy, or overt bleeding tendencies. They are also contraindicated in patients with disease processes suspected to be associated with hypercoagulable states, such as immune-mediated hemolytic anemia or protein-losing nephropathy, because of concerns about cranial vena cava thrombosis and pulmonary thromboembolism.4,5 A CVC placed in the jugular or maxillary vein is also contraindicated in patients with traumatic brain injury because of the potential decrease in cerebral venous drainage that may occur during manipulation of the veins of the neck. Most CVCs tend to be long in length and relatively narrow in diameter, making rapid infusion of large amounts of fluid or blood products difficult.
Equipment
Central venous catheters come in many varieties, including over-the-needle catheters, through-the-needle catheters, and those placed using the Seldinger technique.6 Over-the-needle catheters tend to be stiff and prone to kinking when used as CVCs, whereas through-the-needle catheters are usually the single-lumen variety, which create a vascular defect slightly larger than the catheter itself. Many through-the-needle catheters are difficult to secure. The Seldinger technique facilitates cannulation of a vascular structure using a small-gauge catheter or needle, allowing introduction of a flexible guidewire and subsequently a catheter. It has also been used to catheterize other vascular structures and the peritoneal, pleural, and pericardial cavities.
Catheter Selection and Preparation for Jugular Vein Placement
The length should be such that the tip of the catheter lies within the thoracic vena cava at approximately the level of the 2nd rib space. Measuring the distance between the middle of the jugular vein and the 2nd rib space helps in selecting a catheter of appropriate length. The author generally chooses 4-French catheters for very small dogs and cats (< 7 lb), 5.5-French catheters for animals between 7 and 25 pounds, and 7-French catheters for animals heavier than 25 pounds. All lumens of the CVC, and the over-the-needle catheter or introduction needle, should be filled with heparinized 0.9% saline (1 U/ml).
Step-by-Step: How to Place a Central Venous Catheter (Seldinger Technique)
The following step-by-step procedure discusses placement of a two-lumen, 7-French, 20-cm CVC (Arrow International, Reading, PA) via the right jugular vein in a dog. In the following series of images, the patient is always positioned in left lateral recumbency and the head is always to the right of the image.
What You Will Need
Materials to create a sterile field (clippers, antiseptic preparation solution)
Drape (usually included with central venous catheter kit)
Central venous catheter kit (most kits include all necessary materials for placement) (Arrow International; Reading, PA)
Sterile gloves
Barrier gown, towel, mask
Heparinized 0.9% saline solution (1 U/ml)
Bandages
Step 1
Position patient in lateral recumbency and clip from mid-mandible to second sternebra and dorsal midline to the opposite jugular vein. To assess appropriate field preparation, be sure that no hair from the unclipped area can be folded within 5 cm of the proposed insertion site. Prepare the clipped area using alternating chlorhexidine-based scrub solution and alcohol as for surgery. Use sterile gloves during catheter placement. Use of barrier gown and surgical mask further minimizes risk of contamination.
Procedure Pearl
The multilumen CVC is a key tool that facilitates both monitoring and management of critically ill dogs and cats.

Step 2
The jugular vein lies between the caudal ramus of the mandible (identified by finger in image) and the thoracic inlet. Place an impermeable drape with a fenestration approximately 3- to 5-cm in diameter over the jugular vein, one third of the distance between the caudal ramus of the mandible and the thoracic inlet.
Procedure Pearl
The CVC allows the clinician to measure CVP, to infuse hyperosmolar or irritant solutions (such as total parenteral nutrition), and to reliably and atraumatically retrieve blood samples.

Step 3
An assistant should occlude the jugular vein at the thoracic inlet to identify its course. The assistant then releases pressure on the jugular vein, so you can tent the skin over the jugular vein and make a 3- to 4-mm incision in the skin using a no. 11 scalpel blade. Point the cutting edge of the blade away from the patient to minimize the risk for injuring underlying vasculature. This small defect eliminates tissue drag and is known as the percutaneous facilitative approach.7 This step is a variation on the original Seldinger technique, in which the skin incision is made after step 6.

Step 4
Reocclude the jugular vein at the thoracic inlet and place a thin-walled introducer needle (A) or an over-the-needle catheter (B) into the jugular vein. Most CVC kits contain both an over-the-needle catheter and an introducer needle of appropriate size to accommodate the J-tipped spring guidewire. Attach a syringe filled with heparinized 0.9% saline to the end of the introducer needle (A) or over-the-needle catheter to minimize the risk for air embolus. Intermittent aspiration of this syringe during placement will signify that the jugular vein has been penetrated when a flash of blood is seen in the hub of the needle.
Procedure Pearl
The tip of the CVC placed for monitoring CVP should terminate in the thoracic vena cava of dogs and the thoracic or abdominal vena cava of cats.


Step 5
Insert the J-tipped spring guidewire into the introducer needle or over-the-needle catheter. When the wire passes out of the lumen of the introducer needle or over-the-needle catheter and into the jugular vein, the J-tip will activate, minimizing risk to the vasculature or the heart if the wire comes into contact with it. Note the length of the wire and be sure to advance it only to the level of the cranial vena cava (approximately the 2nd rib space).


Step 6
Remove the introducer needle or over-the-needle catheter over the J-tipped spring guidewire. At this stage, only the J-tipped spring guidewire is left in the vessel.

Step 7
Insert the vessel dilator over the J-tipped spring guidewire and into the jugular vein. The dilator creates a larger defect in the subcutaneous tissues and vein, allowing the catheter to enter smoothly. Remove the dilator. At this stage, again only the J-tipped spring guidewire should be left in the vessel (as seen in step 6). Some bleeding may be noted at this time. Apply mild direct pressure at the insertion site to mitigate hematoma formation.


Step 8
Advance the catheter filled with heparinized 0.9% saline over the J-tipped spring guidewire.

Step 9
Grasp the end of the J-tipped spring guidewire (arrow), which prevents loss of the wire within the patient, and then advance the catheter into the jugular vein.

Step 10
Remove the J-tipped spring guidewire from the catheter, leaving the catheter within the jugular vein.

Step 11
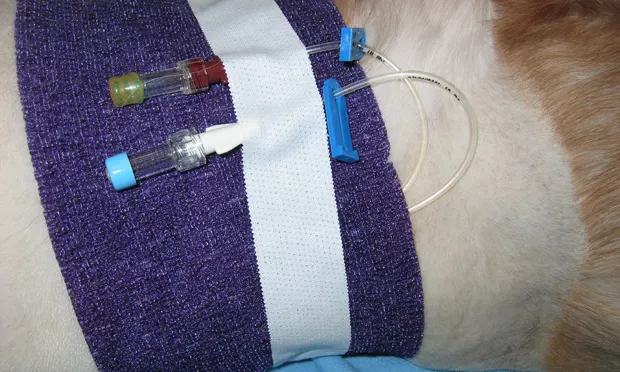
Suture the catheter in place at three anchor points. The "collar" of the catheter should be sutured in line with the jugular vein.

Step 12
Apply a sterile dressing to the insertion site. Evaluate the dressing and the site daily for redness, swelling, or discharge, and change the dressing daily. Most CVCs can remain in place for up to 1 to 2 weeks as long as no indications for removal exist (e.g., redness, swelling, or discharge at the insertion site; cessation of ability to reliably sample from the catheter; jugular vein thrombosis).

Step 13
Thoracic radiography may be used to assess the location of the tip of the catheter. (Note: This image is not from the same patient as in previous images but illustrates proper site of placement).

Step 14
If a fever or other signs of infection of unexplained origin develop, the catheter should be considered as a likely cause and removed and cultured.
Procedure Pearl
General contraindications to the placement of a CVC via the jugular, maxillary, or femoral vein include presence of a significant hemostatic abnormality.