Percutaneously Placed Gastrostomy Tubes: Prevention and Treatment
Endoscopic and nonendoscopic percutaneous implantation of gastrostomy tubes has greatly facilitated nutritional support for dogs and cats that are unable or unwilling to consume a sufficient amount of food. However, gastrostomy may have complications that may be immediate (associated with tube implantation) or delayed (occurring days to months after implantation). Although most complications are minor, some can be major or even life-threatening.

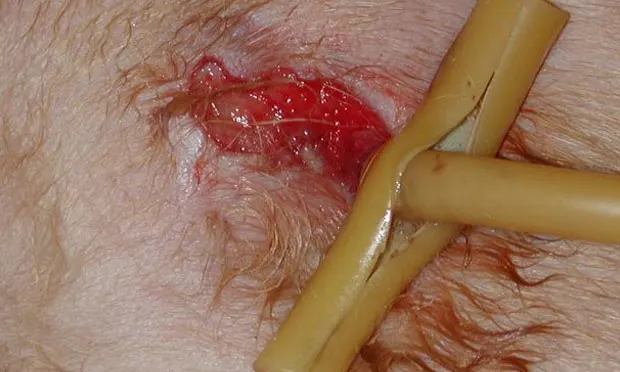
Types of ComplicationsImmediate complications include malpositioning of the tube, splenic entrapment, visceral perforation, pneumoperitoneum, and hemorrhage. Delayed complications may be associated with the gastrostomy tube or underlying disease. Delayed complications include vomiting or slow gastric emptying, difficulty infusing food through the tube, tube wear or removal, peristomal leakage of gastric contents, peristomal inflammation (See Figures 1, above, and 2), or transient fever. Life-threatening complications include hemorrhage or splenic laceration, aspiration pneumonia, and peritonitis. The more severe complications may require tube replacement and/or exploratory laparotomy.
Figure 1. Pressure necrosis cranial to gastrostomy site resulting from overtight outer flange and lack of daily attention to gastrostomy site (Courtesy of Dr. Susan Randell, University of Florida)
Figure 2. Draining tract (blue arrow) and abscess (red arrows) caudoventral to gastrostomy site
IncidenceAmong 54 dogs and cats in which percutaneous endoscopic gastrostomy (PEG) had been performed, Armstrong and Hardie reported immediate complications in 6% and delayed complications in 56%; however, only 18% had major complications and only two cats (4%) died.1 The most common problem was slow gastric emptying (35%). Ireland and colleagues reported complications in 67% of 21 cats with PEG tubes; two thirds of these complications were moderate and one third were minor.2 Vomiting and stomal infections were the most common complications. Bright and coworkers reported complications in 59% of 17 dogs and cats with PEG tubes but all were minor.3 Vomiting was the most common complication (24% of animals). Among 56 dogs with chronic renal failure, of which most (95%) had gastrostomy tubes placed endoscopically, Elliott and coworkers reported immediate complications in 23% of dogs and delayed complications around the stoma in 46%.4 Tube removal was common (20% of dogs), and one dog (2%) died from peritonitis. Tube removal was also common (28% to 30% of animals) in two other studies in dogs and cats.5,6
PEG versus PGSimilar complications occur with a similar frequency when percutaneous gastrostomy (PG) tubes are placed without an endoscope. Fulton and Dennis reported immediate complications in 5% and delayed complications in 60% of 20 dogs after a PG tube was inserted by using a flexible tube passed down into the stomach without an endoscope.7 Delayed gastric emptying (40%), vomiting (20%), and peristomal inflammation (25%) were the most common complications, whereas tube removal occurred in 8% of patients. Mauterer and colleagues reported delayed complications in 50% of eight cats with clinical disease in which a rigid device was used to place a PG tube without an endoscope.8 Clary and colleagues, however, reported an increased incidence of complications when placing a PG tube without an endoscope unless the stomach was inflated with gas before pushing the tube up against the abdominal wall.9
Tube TypeTraditionally, long, mushroom-tipped urologic catheters have been used to feed patients percutaneously, but low-form gastrostomy ports are being used increasingly either to replace longer tubes after a stoma has been established10 or for immediate single-step implantation.11 Complications were reported in all 13 cats implanted with a low-form port in a single step. Most of the complications were mild (cap removal, peristomal dermatitis, leakage, or granulation tissue), but 62% required protective bandaging to stop mutilation of the port and 38% required surgical intervention.11
Complications Following Tube RemovalSome authors have recommended that gastrostomy tubes remain in place for at least 5 days before removal.6,12 However, because malnourished patients take longer to heal, the tube should ideally be left in place for 10 to 14 days.8
Removal MethodTubes can be removed by applying gentle traction while the body wall is supported with fingers on either side of the gastrostomy site. The mushroom collapses, allowing the tube to be pulled out through the body wall. Some authors have supported the mushroom tip with a flange on the inside of the stomach to reduce the likelihood of tubes being pulled out.1,8 This internal flange is left behind in the stomach when the tube is removed by gentle traction and passes through the intestine into the feces. Alternatively, the tube may be cut at the level of the skin, leaving the mushroom tip in the stomach to be passed through the intestine.1,6 The internal flange and the mushroom tip did not cause problems in cats or 20- to 30-kg dogs when left in the stomach, although the mushroom tip remained in the stomach of one cat for 2 weeks after tube removal. Thus, there seems to be a small risk for the internal flange or mushroom to obstruct the intestine. The benefit of an internal flange is uncertain and may not outweigh this risk. Tube removal is a common complication in animals even when an internal flange is used to support the mushroom tip.1,8
PreventionCase SelectionMany complications can be prevented with careful case selection. Gastrostomy tubes should only be placed percutaneously in animals that are not expected to consume a sufficient amount of food for a minimum of 10 days and that have not eaten for 12 to 24 hours. Animals should also have a functional intestinal tract and be able to tolerate general anesthesia. Gastrostomy tubes are more difficult to place percutaneously in obese animals or animals with ascites, and blind endoscopic placement devices may be limited to use in animals weighing less than 15 kg.8
Stoma CareMeticulous care of the stoma site is essential to minimize the risk for peristomal inflammation and infection. Daily cleaning and application of an antiseptic ointment at the site is empirically recommended. A meta-analysis in humans found that prophylactic administration of a single intravenous dose of broad-spectrum antibiotic 30 minutes before PG tube placement reduced the relative risk for peristomal wound infection by 75%.13 Thus, a single intravenous dose of cefazolin given 30 minutes before PG tube placement is recommended.
Traction / MovementExcessive traction should not be applied to the PG tube. In humans, many complications, such as gastrointestinal bleeding, peristomal leakage and inflammation, and tube extrusion, have been attributed to application of excessive traction on the PG tube.14 In dogs, early PG tract formation did not depend on proximity of the stomach to the abdominal wall.15 Complete tract formation occurred within a week when a 3-cm gap was left between the stomach and abdominal wall. To-and-fro motion prevented early tract formation when the tube was not fixed externally, which suggests that movement of the tube should be minimized.15 After gastrostomy placement, therefore, no blanching of the gastric mucosa should be visible with the endoscope around the mushroom, which suggests excessive traction on the tube. The position of the external flange should be marked to allow subsequent determination of whether any inward migration of the tube has occurred; however, the flange may need to be moved outward after a day or two to allow for tissue swelling. One paper reported using a Chinese finger suture around the tube to fix the tube in position.1 Rotating the tube is not recommended.
Tube Composition / TypeNeither the composition nor the type of catheter affected the incidence of early stomal complications in dogs; however, latex catheters lasted three times longer.4 Tract formation occurred rapidly irrespective of catheter composition.15 Premature tube removal is a greater concern. The tube should, therefore, always be covered with an elastic stockinette bandage and the pet should wear an Elizabethan collar if necessary. Confinement for 7 days in well-nourished animals and for 14 days in malnourished animals is recommended after gastrostomy until a permanent adhesion between stomach and body wall has formed.8,15
FeedingsVomiting can often be prevented if food is introduced gradually, and small meals are given frequently. No food should be offered for 12 to 24 hours to allow fibrin deposition around the stoma site. Food should be infused slowly over at least 1 minute to allow for gastric relaxation, and should be stopped at the first sign of salivation or retching. Only 25% to 50% maintenance energy requirements, divided into four to six meals, should be offered on the first day. Maximum stomach capacities are quite high,12 however; and much larger volumes may be infused if the size of each meal is increased slowly.
Infusion of foods through a gastrostomy tube is usually fairly easy in small dogs and cats. The tube should initially be flushed with water. Warmed gruel and semisolid foods thus can usually pass easily down large 18- to 24-French gastrostomy tubes. Gruel should be sieved, medications should be crushed to remove any large particles, and tubes should be flushed with water after use. A column of water left within the tube may also reduce the risk for blockage. Pet foods containing increased insoluble fiber should be avoided because they tend to be viscous unless mixed with large amounts of water. Tubes may be shortened to facilitate infusion. Nevertheless, providing enough food to support a large-breed dog via a gastrostomy tube is an onerous task unless a mechanical pump is used to facilitate the process.
TreatmentHemorrhage / PerforationMost immediate complications, such as severe hemorrhage or perforation of an organ, are life-threatening and require immediate exploratory surgery. Gastric hemorrhage rarely causes clinical signs, however, and usually resolves with conservative therapy.
PeritonitisBecause it is life-threatening, peritonitis secondary to displacement of the catheter tip out of the stomach should be ruled out. If there is any doubt, plain radiographs or ultrasonography may show evidence of free fluid or air in the abdomen. Peritoneal fluid may be aspirated for cytologic studies. Radiographs obtained after an aqueous contrast agent, such as iohexol, has been infused through the tube can show tube location and whether there is a leak (Figures 3 to 5).

Figures 3a & 3b. Pre- and postcontrast ventrodorsal radiograph of a cat with low-form gastrostomy tube showing normal positioning of tube in stomach and normal gastrogram without leakage into the peritoneum (Courtesy of Dr. Susan Randell)

Figures 3a & 3b. Pre- and postcontrast ventrodorsal radiograph of a cat with low-form gastrostomy tube showing normal positioning of tube in stomach and normal gastrogram without leakage into the peritoneum (Courtesy of Dr. Susan Randell)

Figures 4a & 4b. Ventrodorsal and lateral radiographs of percutaneously placed gastrostomy tube showing that the intraabdominal portion of the tube is not contained within the stomach. A number of small, irregularly shaped air bubbles are visible in this region (arrows). There is a mild decrease in midabdominal peritoneal detail that may be caused by the overlying wet hair or peritoneal fluid. (Courtesy of Dr. Eric Ferrell, University of Florida)
Figures 4a & 4b. Ventrodorsal and lateral radiographs of percutaneously placed gastrostomy tube showing that the intraabdominal portion of the tube is not contained within the stomach. A number of small, irregularly shaped air bubbles are visible in this region (arrows). There is a mild decrease in midabdominal peritoneal detail that may be caused by the overlying wet hair or peritoneal fluid. (Courtesy of Dr. Eric Ferrell, University of Florida)
Figures 5a & 5b. Lateral and ventrodorsal radiographs of low-form gastrostomy tube after infusion of 10 ml of iohexol. The tube is outside the abdominal wall, and contrast is dissecting subcutaneously. (Courtesy of Dr. Eric Ferrell, University of Florida)
Figures 5a & 5b. Lateral and ventrodorsal radiographs of low-form gastrostomy tube after infusion of 10 ml of iohexol. The tube is outside the abdominal wall, and contrast is dissecting subcutaneously. (Courtesy of Dr. Eric Ferrell, University of Florida)

Figure 6. Crack in low-form gastrostomy tube (Courtesy of Dr. Kirsten Cooke, University of Florida)
VomitingVomiting usually resolves with a reduced quantity of food and increased meal frequency. Vomiting may also occur if there is delayed gastric emptying. The amount of residual food can be determined by applying negative pressure to a syringe attached to the gastrostomy tube. A residual volume of more than 2 ml/kg suggests poor gastric emptying. Prokinetic agents, such as metoclopramide (0.2 to 0.4 mg/kg Q 8 H PO or SQ or 1 to 2 mg/kg daily continuously IV), cisapride (0.1 to 1.0 mg/kg PO Q 8 H), ranitidine (1.0 to 2.0 mg/kg PO Q 12 H ), nizatidine (2.5 to 5.0 mg/kg PO daily), or erythromycin (0.5 to 1.0 mg/kg PO or IV Q 8 H), should then be administered. Liquid and low-fat foods empty more rapidly from the stomach, and gastric emptying may also improve with plasma infusion in hypoproteinemic patients. If vomiting persists, then peritonitis secondary to tube-tip displacement should be ruled out; otherwise, the underlying disease process may be responsible. In these cases, the disease should be treated and nausea should be addressed with antiemetics, such as metoclopramide or ondansetron.
Tube Blockage / DisplacementTube displacement should also be considered when the amount of pressure required to force food through the lumen of the tube increases. Tube blockage is rare, except in narrow bore tubes. Radiography after infusion of contrast agent into the tube should clarify whether a tube is blocked or whether the tip has become displaced. Tubes can usually be unblocked with carbonated cola drinks, a slurry of pancreatic enzyme powder in water, or a declogging device.16