Myringotomy & Ear Disease Management
Louis N. Gotthelf, DVM, Animal Hospital of Montgomery & Montgomery Pet Skin and Ear Clinic; Montgomery, Alabama
Myringotomy serves the same purpose as the insertion of pressure equalization tubes into human eardrums (tympanic membranes): to relieve pressure on the eardrum, making the pressure inside and outside the bulla the same. Attention to clinical signs and patient history will alert the clinician to the need for myringotomy in the management of ear disease. Positive pressure within the tympanic bulla from exudates and secretions places excessive pressure on the eardrum. That pressure results in severe pain and decreased hearing caused by the presence of fluid in the bulla and the inability of the eardrum to vibrate. This pressure also increases the chances that the patient will have vestibular signs.
Myringotomy incision relieves the pressure on the eardrum and almost immediately reverses pain, improves hearing, and may reverse vestibular signs. If there is an infection within the bulla (otitis media), medications can be placed into the bulla through the myringotomy incision to topically treat the infection. Identification of an abnormal eardrum becomes much simpler with the availability of video otoscopy.
Indications
Patients with the following indications are candidates for myringotomy:
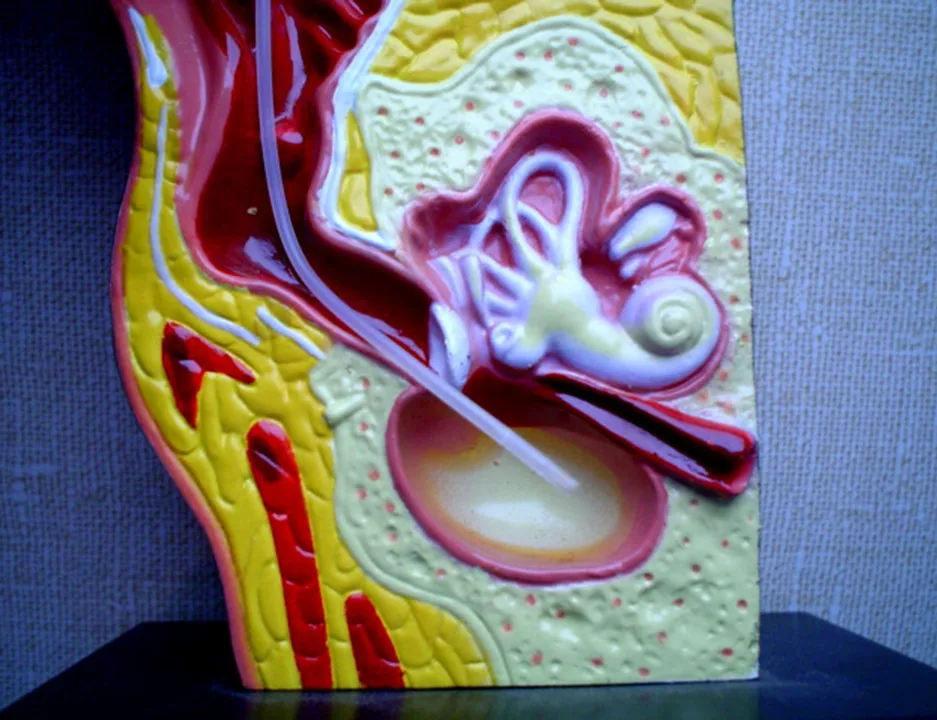
Bulging eardrum identified on otic examination (Figure 1)

FIGURE 1 Middle ear exudates fill tympanic bulla, putting painful pressure on the eardrum and causing it to bulge outward.
Visualization of fluids (eg, blood, pus, mucus, serum) behind the eardrum in the middle ear (Figure 2)

FIGURE 2 Left middle ear inflamed with exudate and blood behind eardrum (left). The normal right eardrum is shown for comparison (right).
Confirmation of solid or opaque mass filling the bulla (Figure 3)

FIGURE 3 This cat has a solid mass of tissue in the right middle ear. Myringotomy and cytology revealed lymphoma.
Chronic ear disease that has led to thickening and scarring of the eardrum (Figure 4)

FIGURE 4 Normal right eardrum (left). Fibrous connective tissue covering the left eardrum (tympanosclerosis) (right).
Middle ear disease can cause excessive scratching or head shaking in an effort to relieve pain from the pressure of exudates on an intact eardrum. Manipulation of the ear canal may result in vocalization and aggressive behavior as the patient responds to pain stimulation.
Neurologic signs may also indicate middle ear disease, as many nerves course in and around the middle ear. In addition, the round and oval windows provide entry of material from the tympanic bulla into the inner ear. Facial palsy, vestibular disease, and Horner syndrome can all result from otitis media and subsequent otitis interna. A prolapsed third eyelid warrants examination of the ipsilateral eardrum.
Patients with chronic, recurrent, or unresponsive otitis externa often suffer from concurrent otitis media. Radiography of the tympanic bullae may reveal thickening caused by inflammatory stimulation of the periosteal lining. Not all radiographs will reveal changes of bulla osteitis, even if it is present. Other imaging modalities (eg, CT, MRI) have superior sensitivity and the ability to visualize soft tissue within the bulla.
Myringotomy may be indicated if clinical and bulla imaging signs of otitis media are present despite having an intact eardrum.
Benefits
The principal benefit of opening the eardrum is to relieve severe pain caused by the pressure of built-up exudates associated with middle ear inflammation. Pain relief is almost instantaneous after the procedure. The mucoperiosteum (ie, eardrum lining) contains both a mucous membrane and a periosteal membrane intimately attached to one another. Middle ear inflammation results in copious mucus secretion from the goblet cells and pus production. The bulla has poor drainage through the tiny auditory tube and, therefore, pressure increases on the eardrum.
Another benefit is reestablishment of air pressure changes within the bulla compared with atmospheric pressure. The eardrum may be sucked inward or bulged outward, depending on pressure changes within the bulla.
Eardrum incision also serves as topical treatment of middle ear disease. Insertion of a polypropylene or red rubber tube into the bulla allows flushing of exudate and suctioning and removal of flushing.
Step-by-Step: Myringotomy
What You Will Need
Spinal needle
Buck ear curette
5-Fr polypropylene catheter cut to 60° angle
CO2 or diode laser
3-mL syringe
Cotton-tipped applicator
Aerobic culturette swabs

Additional Equipment
Video otoscope or operating head otoscope
Device to flush/suction bulla:
60-mL syringe
Irrigation/suction pump (Earigator, otopet-usa.com)
Flush solution (0.9% NaCl)
Step 1
Prepare the patient by inducing a deep level of anesthesia (intubation), followed by deep ear cleaning and suctioning to remove fluid from the eardrum surface in the horizontal ear canal.

For the myringotomy incision: The pars flaccida should be in the dorsal position at 12 o’clock. For the left eardrum, incise the pars tensa at the 5 o’clock position opposite to the manubrium of the malleus; for the right ear, incise the pars tensa at the 7 o’clock position opposite and ventral to the manubrium of the malleus.
Author Insight
The myringotomy incision site is on the ventral part of the opposite side of the eardrum as the malleus. However, disease often obscures normal anatomy.
Step 2
Insert the incising instrument to the proper position. The pointed tip of the cut catheter should be placed at the eardrum.

Step 3
Quickly punch through the eardrum to make the incision. A swift insertion through the membrane may result in a “pop” as the catheter pierces the membrane. Middle ear exudates are often forced out after the incision. Some bloody mucus may exit the incision.

If not using a video otoscope to make the incision, insert the tip of the catheter into the otoscope and guide it ventrally toward the eardrum. Once the eardrum can be seen clearly, quickly advance the catheter into the bulla at the most ventral position.
Regardless of whether the incision is made with a video or surgical otoscope, any bleeding indicates that it was not made in the proper position. Damage to either the pars flaccida or the malleus bone results in bleeding, which can slow healing.
Laser myringotomy is usually reserved for cases with pronounced eardrum thickening that prevents a polypropylene catheter incision. When using a CO2 laser, position the laser tip at the appropriate location opposite and ventral to the malleus. Using a 500-msec time and 4-watt power setting, a single laser pulse will make a circular opening in the eardrum. If the incision is not large or deep enough, another single pulse may be used adjacent to the first opening. A diode laser tip has to touch the eardrum as the energy is supplied to cut through the eardrum.
Step 4
With the catheter method, insert and advance the catheter as deep as it will go. With the spinal needle or the curette method, make the incision and withdraw.
Step 5
Insert an open-ended catheter into the bulla. If using a surgical otoscope head, poor visualization can make threading a catheter through the myringotomy incision difficult.
Author Insight
Access to the material produced in the tympanic cavity allows bacterial culture and antibiotic sensitivity testing of this material as well as cytologic analysis of the exudate.
Step 6
To sample the bulla, withdraw any fluid in the bulla through the catheter using a 5-mL syringe. Some fluid will reach the syringe, but in some cases there will be scant fluid filling the lumen of the catheter. Withdraw the catheter from the bulla and apply the contents to the cotton-tipped applicator (for cytologic examination) and to the culturette (for bacterial culture).
Step 7
To flush the bulla, insert an open-ended catheter until it hits bone. Flushing fluid (either 0.9% saline solution or tap water) overflows into the external ear canal, from which it is then suctioned out. Irrigate the bulla through high pressure with a 60-mL syringe or a mechanical irrigator, observing for material flushed out of the incision. Suction fluid from the bulla, and repeat flush and suction until flushing solution exits the incision without any material. Suction as much fluid as possible from the bulla.

Step 8
For bulla infusion, topical treatment of the lining of the bulla includes aqueous nonototoxic drugs. The bulla volume should be no more than 1 mL, so infusion of more than the bulla volume will either drain through the auditory tube into the throat or fill the lower portion of the horizontal ear canal. Minimal drainage from tympanic bulla when in sternal position allows medicine to be retained for several days.
In dogs, antibiotics (ciprofloxacin injection or ophthalmic, enrofloxacin injection, tobramycin ophthalmic, ticarcillin injection, ceftazidime injection) can safely be infused into the bulla, overflowing into the horizontal ear canal. In cats, aqueous steroids (fluocinolone/DMSO or dexamethasone sodium phosphate, 4 mg/mL) can safely be infused into the tympanic bulla.
Step 9
Germinal epithelial cells arising from the area of the malleus will slide across the incision to heal. Healing in the eardrums may be blocked as a result of increased secretions and pressure within the bulla, preventing a seal and allowing secretions to escape.
Lower pressure accompanies decreased bulla secretions, allowing healing to proceed; after secretions cease, incision healing is complete within 10 to 14 days.

Author Insight
Once the bulla surface is clean and dry, appropriate topical medication may be infused into the bulla cavity to cover the inflamed mucoperiosteal membrane.