Diagnosis of Mycobacterial Infections in Cats
This case illustrates the first known diagnosis of Mycobacterium farcinogenes in an 8-year-old spayed domestic shorthair cat.
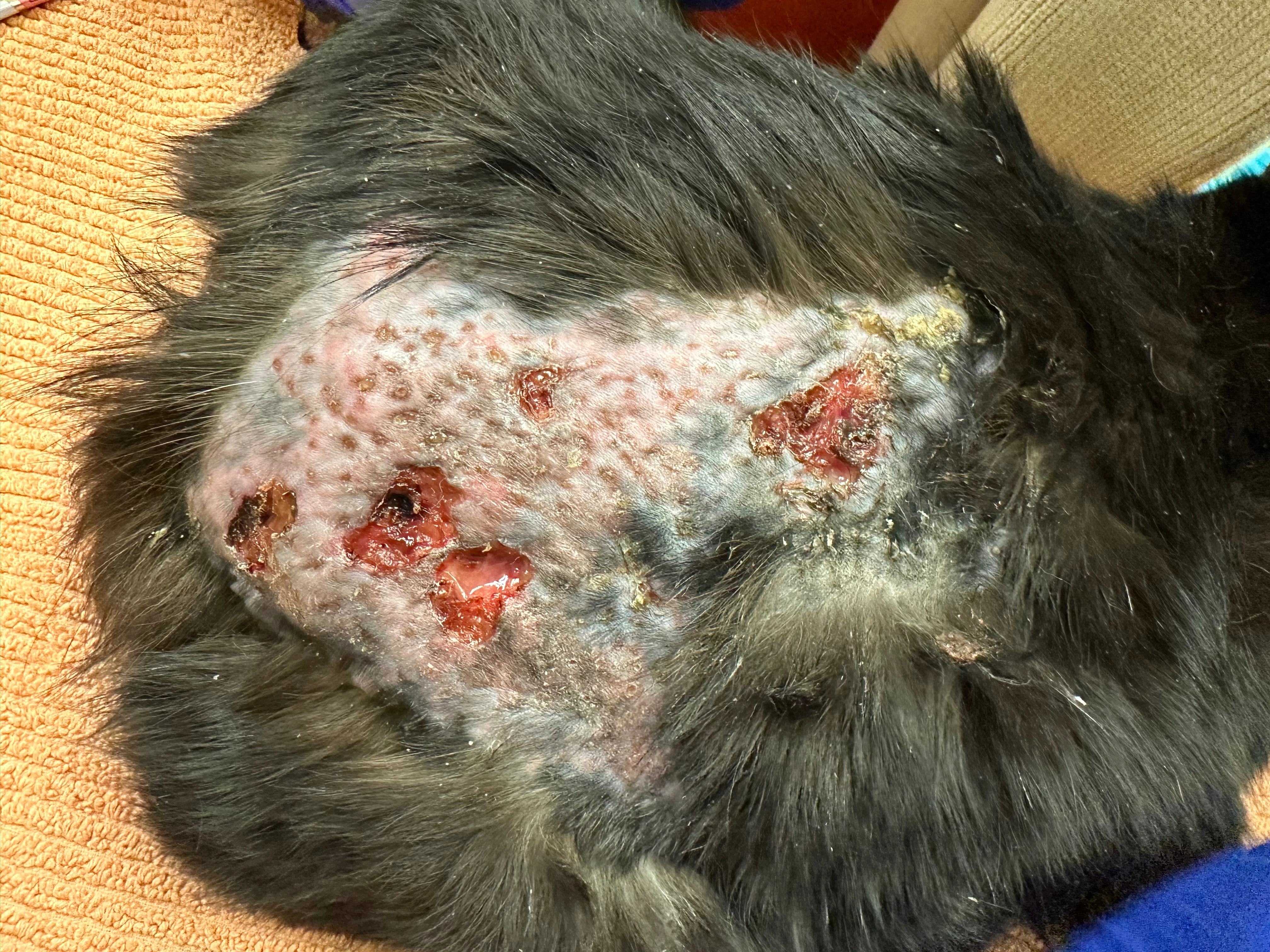
Granulomatous panniculitis can appear as subcutaneous nodules with multiple draining tracts and large areas of ulcerated, nonhealing tissue. Mycobacterial panniculitis refers to the clinical syndrome characterized by chronic infection of the subcutis and skin of cats by nontuberculous mycobacteria and is most commonly associated with rapid-growing species (eg, Mycobacterium fortuitum, Mycobacterium smegmatis, other rapid-growing Mycobacterium spp).
Diagnosis of mycobacterial panniculitis is often challenging, and mycobacterial tissue culture should be performed in all nonhealing cases of granulomatous panniculitis that do not respond to empiric antimicrobial therapy. Histopathology of the skin biopsy usually shows pyogranulomatous inflammation, and acid-fast stains may aid in diagnosis; however, many of these cases can be negative even on special stains.
Treatment of Mycobacterial Infections in Cats
Diagnosis of mycobacterial infections is key for determining appropriate treatment, which involves antimicrobial therapy for several months (continuing at least 2 months after resolution of clinical signs) in most cases. Combination antimicrobial therapy is likely needed, as administration of >1 drug generally increases the chance for clinical resolution and decreases potential development of antimicrobial resistance. The drug combination usually consists of 3 of the following antimicrobials: fluoroquinolones (eg, pradofloxacin), azithromycin, rifampicin, or doxycycline (possibly); however, fluoroquinolones generally have poorer efficacy for some Mycobacterium spp, and culture with susceptibility testing should be performed to identify which antimicrobials should be used for treatment.1-4 For resistant and extensive disease, additional combinations (including ethambutol, clofazimine, or amikacin) can be considered but should be based on susceptibility testing.
Surgical excision of small cutaneous lesions can be considered in some patients, but debulking of larger lesions risks wound dehiscence and local recurrence of infection and should only be performed once the patient has received appropriate antimicrobial therapy for several weeks to months.