Modified Perineal Urethrostomy for Obstructed Goats
Karen M. Tobias, DVM, MS, DACVS, University of Tennessee
Sarel R. van Amstel, BVSc, Dip MedVet, M MedVet, DACVIM, University of Tennessee

Diet and anatomy predispose male goats and other small ruminants to obstructive urolithiasis. Uroliths, commonly containing phosphate secondary to high-grain or concentrated diets, often become lodged in the distal sigmoid flexure or the urethral process (ie, vermiform appendage) where the urethra narrows.
Clinical signs of obstructive urolithiasis include stranguria, urine dribbling, and evident discomfort (eg, restlessness, tail twitching, vocalization, colicky behavior). If the bladder or urethra ruptures, the animal may become anorectic and lethargic and develop abdominal distention or subcutaneous urine accumulation, respectively. Goats with obstructive urolithiasis can eventually become dehydrated or may develop azotemia and acid–base and/or electrolyte imbalances (eg, hyperkalemia). Death can result from untreated metabolic derangements. Stabilization with IV fluids is critical for correcting metabolic abnormalities, especially before inducing anesthesia.
If obstruction is suspected, the hairs around the prepuce should be examined for blood clots, crystals, and small stones. Abnormalities of the urethra or bladder may be detected by digital rectal examination, and free fluid in the abdomen can be detected on ultrasound imaging. If urine is obtained by abdominocentesis, the creatinine concentration will be 1.5 to 2 times that of peripheral blood.
For full penile examination, the goat should be sedated with acepromazine at 0.05 to 0.1 mg/kg IV or IM or diazepam at 0.1 mg/kg IV. The goat should be placed in a seated position with its peri-neum on the ground and forelimbs elevated for exteriorization of the penis. If the urethral process is present, it can be amputated with scissors or scalpel, possibly providing temporary relief of distal obstructions. A urethral diverticulum at the level of the ischial arch can impede retrograde catheterization of the urinary bladder; therefore, urethral flushing is not routine.
Surgical Options
If obstruction cannot be relieved by urethral process amputation or fluid administration, options include tube cystostomy, urethrotomy, urethrostomy, or bladder marsupialization.
Tube cystostomy is often a short-term recommendation to allow urethral healing or resolution of any swelling after a urolith has been passed; complications include ongoing obstruction, peritonitis, urethral rupture, catheter dislodgement, or adhesions. Bladder marsupialization can cause incontinence, potentially resulting in body odor, urine scald, and frustrated owners. Other complications include ascending urinary tract infection and bladder mucosal prolapse. Prepubic urethrostomy reroutes the urethral opening cranial to the brim of the pubis; it is rarely used in goats because of difficulty, anatomic angle limitations, and risk for recurrent cystitis or further stricture. Traditional perineal urethrotomy and urethrostomy are considered salvage techniques, as stricture and recurrence of signs have been reported 8 months after surgery in 45% to 78% of goats.1,2
Related Article: Urinary Obstruction: Treatment Measures
Related Article: Emergency Management of Urethral Obstruction in Male Cats
Modified Proximal Perineal Urethrostomy
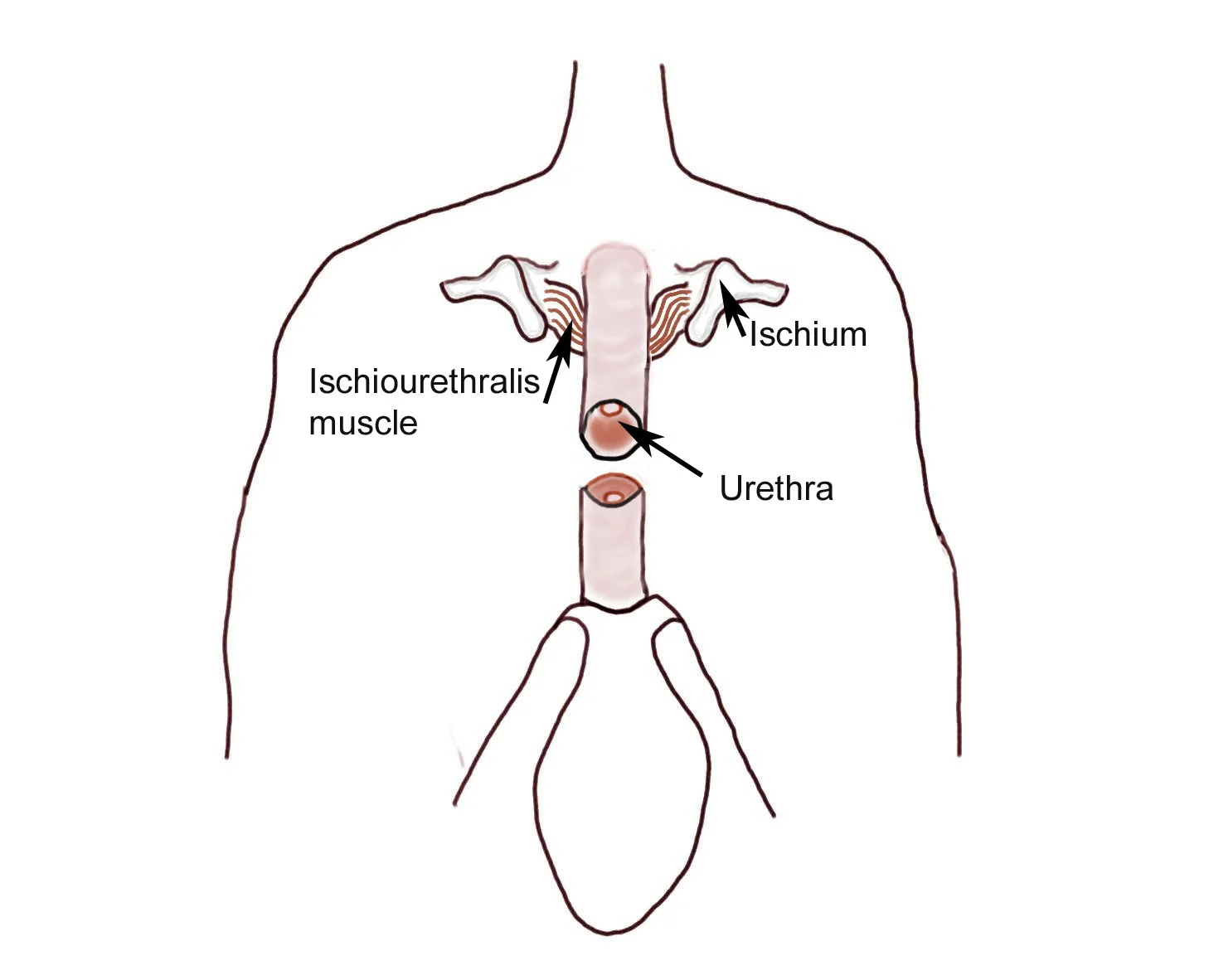
Stricture occurrence can be reduced by transecting attachments of the penile body (differentiated from the penile tip) to the ischium and pubis and carefully apposing urethral mucosa to the skin. Transecting the ischiourethralis muscles and ventral penile ligament can improve penile mobility, provide more length for urethrostomy, straighten the penile body, and facilitate urethral catheterization by narrowing the opening of the urethral diverticulum. It may also reduce tension on the urethrocutaneous anastomosis. The anastomosis can be performed with absorbable monofilament suture.
Modified proximal perineal urethrostomy is the authors’ routine when goats not intended for breeding have urethral obstruction that cannot be resolved easily. Although the authors have not seen postsurgical strictures, the procedure may present other complications. Modified proximal perineal urethrostomy is more difficult in goats than in cats: penile attachments are thick and firm, and some tissues must be transected blindly, potentially leading to hemorrhage. Veterinarians unaccustomed to performing surgery on goats should practice on a goat cadaver before attempting this procedure.
Modified proximal perineal urethrostomy does not prevent urolithiasis; goats can still be obstructed by large calculi if appropriate dietary and medical management is not instituted. Patients may develop urine scald if the urethrostomy diverts urine toward the hocks.
Step-by-Step: Modified Perineal Urethrostomy for Goats
What You Will Need
Standard soft tissue surgery pack, including:
Debakey thumb forceps
Metzenbaum scissors
Periosteal elevators or cartilage scissors
Malleable retractors
8 or 10 French red rubber catheter
2-0 and 3-0 or 4-0 absorbable monofilament suture
Tenotomy or iris scissors
Skin suture
Step 1
Position the goat in sternal recumbency in a perineal position with hindlimbs hanging over the end of a padded surgery table. Place additional roll towels under the cranial thorax and neck to keep the patient’s head upright. Place a purse-string suture in the anus before proceeding with final preparations. Drape the patient so the ischial tuberosities (indicated by hemostats) are in the center of the field and the anus is covered.

Step 2
Starting at the level of the ischial tuberosities, incise the skin ventrally along the perineal midline for 6–8 cm. Identify the penile body by digital palpation and, with blunt and sharp dissection, free it from surrounding tissues to the level of the ischium. Transect the retractor penis muscles if present. When possible, separate the dorsal artery of the penis from the penile body and retract it cranially.
Author Insight
Raising the table to level the surgeon’s line of vision with the perineal region can prevent inadvertent transection of the penile body too far proximally.

Step 3
Transect the penile body at the caudal aspect of the proximal end of the sigmoid flexure, about 4–8 cm distal to the caudal edge of the pubis.
Author Insight
Although it is known as the dorsal artery of the penis, at this level the artery is actually cranial or ventral to the penile body.
Step 4
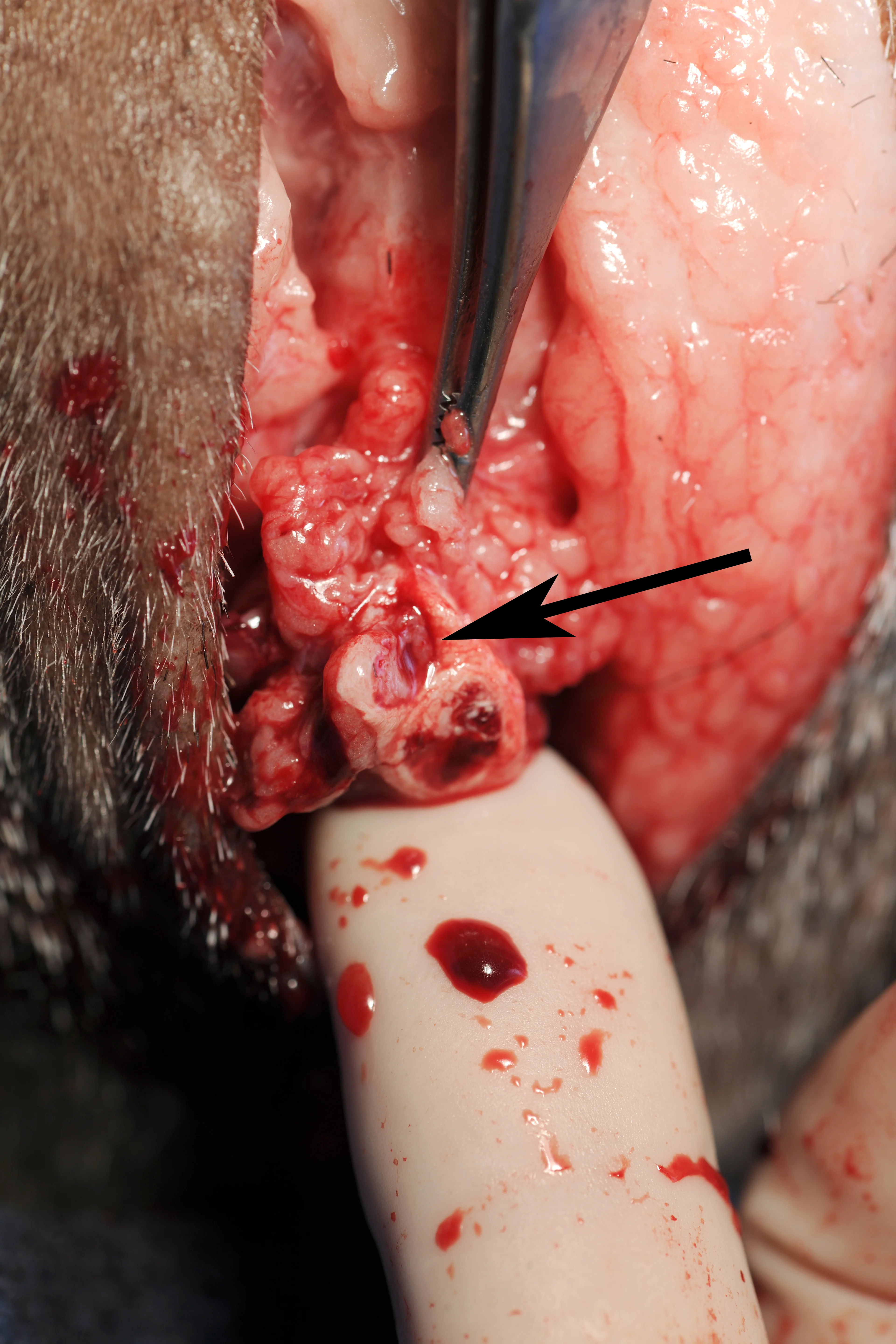
Identify the urethra (arrow) on the dorsal surface of the transected penile body. If the proximal or distal segment of the penile body is bleeding, oversew the segment end with absorbable monofilament or directly ligate any vessels.
Author Insight
If oversewing the proximal segment, pass a urethral catheter to avoid including the urethra in any sutures.
Step 5
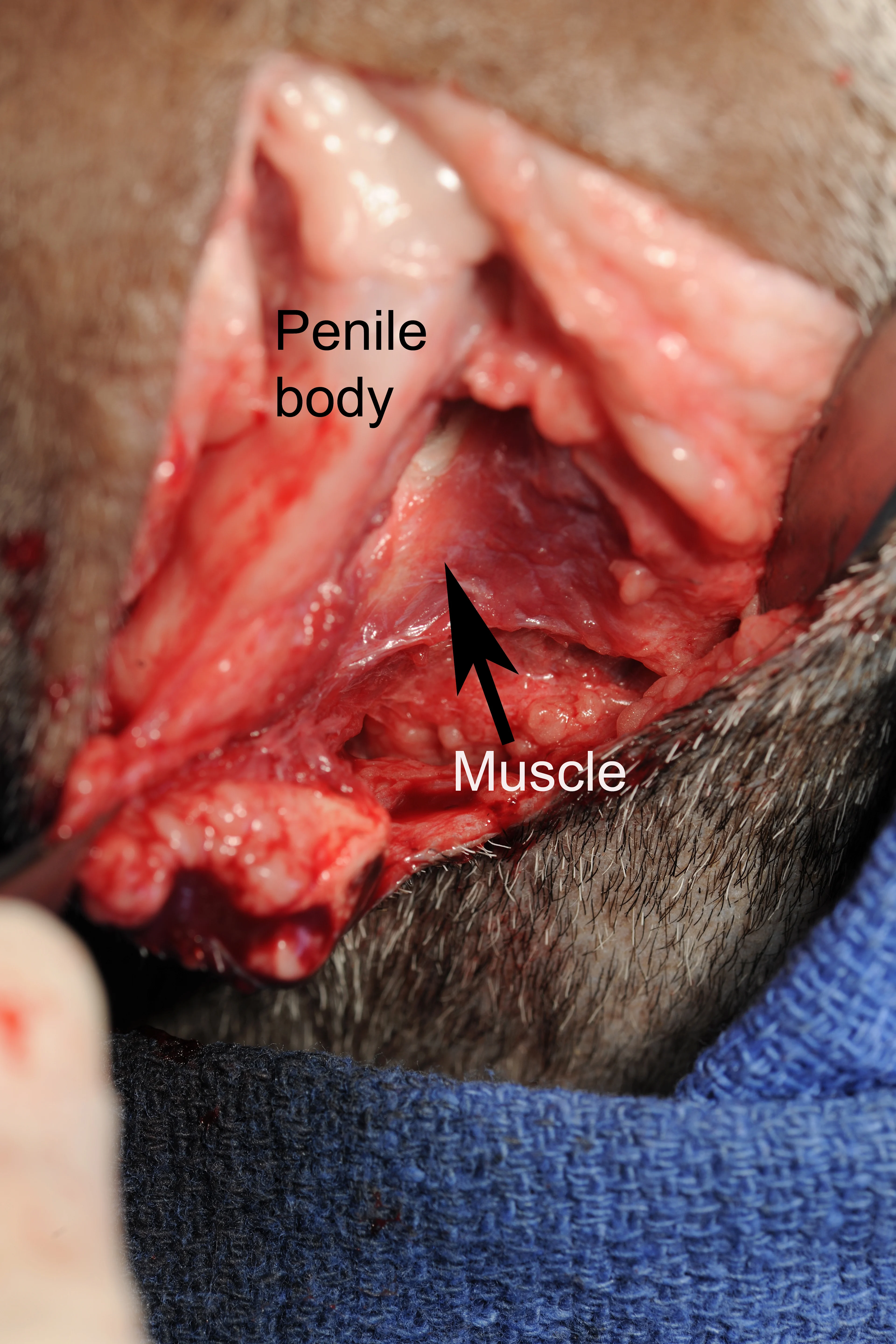
Retract the penile body to one side while an assistant uses a malleable retractor to retract the skin to the opposite side. Identify the ischiocavernosus muscle (A, arrow) and transect with scissors (B). Repeat the process on the opposite side.
Author Insight
To facilitate manipulation of the proximal penile segment, the tunica albuginea can be grasped with tissue forceps.

Step 6
Retract the penile body dorsally and use a periosteal elevator, cartilage scissors, or blade to carefully separate any remaining attachments between the penile body and pelvis. Use intermittent digital palpation to identify remaining tissues and verify that the ventral 180° section of the penile body has been freed.

Step 7
Retract the penile body ventrally and use Metzenbaum scissors to incise 2 cm on the dorsal midline of the urethra.
Author Insight
The ischia of the male goat are angled acutely. The surgeon should frequently palpate the area for orientation. At this stage, it can be easy to slip below the ischium and pubis; dissection ventral to the pelvis can dramatically increase hemorrhage.

Step 8
Suture the spatulated end of the urethra to the perineal skin with absorbable monofilament suture, starting dorsally. First, place a simple interrupted suture from the dorsolateral mucosa to the dorsolateral skin (A). Place a second suture similarly on the contralateral side. Place 1 or 2 interrupted sutures from the most dorsal extent of the urethral mucosa to the skin dorsolaterally (B).
Author Insight
The dorsal interrupted sutures can be preplaced and secured with hemostats to evaluate the position of the urethrostomy before sutures are tied.


Step 9
Once the dorsal sutures are placed and tied, suture the urethral mucosa to the skin on each side in a continuous pattern. Close any remaining skin incision routinely. If significant postoperative hemorrhage occurs, place a Foley catheter through the urethrostomy and into the bladder before applying a pressure bandage to the perineal area.
Author Insight
Once the dorsal sutures are in place, the bladder should be easily catheterized through the urethrostomy site. If it is not, pelvic attachments may remain, curving the penile body downward and allowing the catheter to divert dorsally into the urethral diverticulum.


Step 10
Ensure healthy urination through a healed urethrostomy site.
