Image Gallery: Eosinophilic Keratitis in Cats
Georgina M. Newbold, DVM, DACVO, The Ohio State University
Diane Van Horn Hendrix, DVM, DACVO, University of Tennessee, Knoxville
Overview
Eosinophilic keratitis (EK; also called proliferative keratoconjunctivitis) is a poorly understood disease. Although its clinical behavior and signs are unique to cats, cytologically similar conditions have been reported in horses1 and rabbits.2
In general, EK is thought to be an immune-mediated disease. It has been tenuously linked to feline herpesvirus 1 (FHV-1), although the causal mechanism has not been elucidated and studies are conflicting.3-7
There is no reported sex predilection; median age at diagnosis in one study was 5 years.8
Clinical Behavior
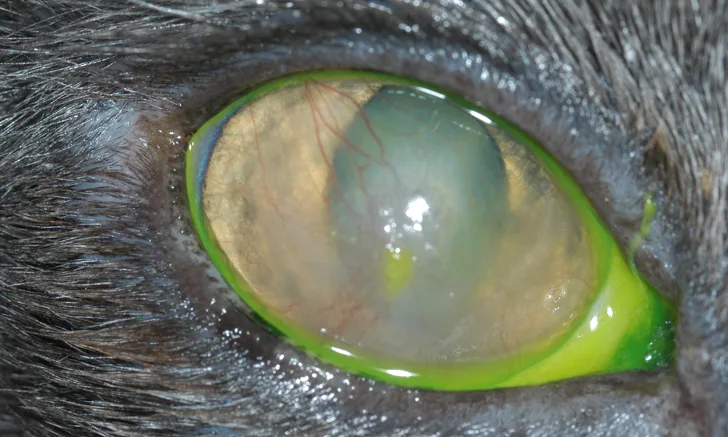
EK most often appears as an irregular, raised, white-to-pinkish plaque with focal corneal vascularization, typically starting at the dorsotemporal quadrant of the cornea.
The entire cornea can become affected with clinical progression. The conjunctiva may or may not be involved, and the disease can be unilateral or bilateral.
Vision can be affected later in the course of disease, as the dense corneal opacities can interfere with the visual axis.
Diagnosis
Differentials for EK can include chronic ulcerative keratitis or granulation tissue secondary to ulcerative disease.
In other species (eg, horses, cattle), squamous cell carcinoma (SCC) may have a somewhat similar raised or proliferative appearance.9
Corneal SCC has not been reported in cats and should not be considered as a top differential.
Diagnosis involves cytologic evaluation of corneal scrapings using a cytobrush, Kimura spatula, or blunt end of a scalpel blade to gently gather cells from the corneal surface after application of a topical anesthetic agent (eg, proparacaine 0.5%).
Cytologic evaluation can reveal inflammatory cells, including eosinophils, mast cells, plasma cells, lymphocytes, and neutrophils.
If even a single eosinophil is visualized, treatment for EK is indicated.
Pathogenesis & Treatment
The specific etiology and pathogenesis of EK is unknown; however, it has been theorized that signs result from a delayed hypersensitivity reaction to an unknown stimulus.10
The response to immunomodulatory therapy supports this theory.
EK responds to treatments similar to those used for other immune-mediated diseases; immunomodulatory therapy is the mainstay in EK management. Topical corticosteroids are essential to control clinical signs; lifelong therapy is often necessary to prevent recurrence.
Initial therapy typically includes topical prednisolone acetate 1% at 1 drop q6h, tapering by 1 daily drop (or 25% reduction) q1-2wk until adequate maintenance of 1 drop q24-48h is achieved. Therapeutic response is shown via resolution of the corneal plaque and disappearance of corneal vascularization.
Some patients may require more frequent long-term treatment, but many can be managed with q48h therapy.
Topical dexamethasone sodium phosphate 0.1% can be substituted for topical prednisolone following the same protocol as above.
Transition to q12h administration of topical cyclosporine 0.2% may be appropriate in some patients to reduce, and eventually substitute, for topical steroid use.
Note: Although treatment success using cyclosporine 1.5% has been reported,11 the authors advise use of a commercially available cyclosporine 0.2% to avoid compounded products when possible.
Concurrent antibiotic and/or antiviral therapy may be added if corneal ulceration is present or FHV-1 involvement is suspected.
If cytology shows evidence of eosinophilic inflammation, clinical signs will not resolve without implementation of immunomodulatory therapy (eg, cyclosporine or corticosteroid). If an active corneal ulceration is noted concurrently, prophylactic topical antibiotic therapy such as oxytetracycline ointment (ie, Terramycin ophthalmic ointment) QID may be initiated for 5-7 days prior to starting treatment for EK. If evidence of concurrent upper respiratory infection leads to suspicion of concurrent FHV-1 infection, oral famciclovir (90 mg/kg PO BID) or topical cidofovir 0.5% ophthalmic solution BID can be initiated for 5-7 days prior to starting treatment for EK.12

FIGURE 1
Typical presentation of relatively early-stage feline EK in the right eye of a 5-year-old domestic shorthair cat. Note the raised plaques on the conjunctiva and dorsotemporal quadrant of the cornea and focal corneal vascularization. No corneal ulcers were associated with the plaques, and the patient did not appear uncomfortable.