Hospital-Acquired Catheter-Related Bloodstream Infections
Amanda A. Cavanagh, DVM, DACVECC, Colorado State University
Carlee Fiddes, PSM, BS, AAS, LVT, Colorado State University

A hospital-acquired infection (HAI) is an infection developing after 48 hours of hospitalization that was not present or incubating at the time of admission.1-3 Common HAI sites include the respiratory and urinary tracts, surgical incisions, and the bloodstream. Bloodstream infections, while representing only a small percentage of hospital-acquired infections in people, have a high fatality rate.1
Hospital-acquired bloodstream infections most commonly originate from IV catheters and should be suspected in any patient with an IV catheter that develops systemic inflammatory response syndrome without an extravascular infection source.2-4 Catheter insertion- site inflammation may not be present.5 Antimicrobial resistance is common in HAIs; therefore, tissue, blood, and catheter culture and sensitivity testing must be performed to select appropriate antimicrobial therapy.
Case Summary
Amanda A. Cavanagh, DVM, DACVECC, Colorado State University
An 8-year-old neutered male borzoi presented with lung lobe torsion. Following a right middle-lung lobectomy, he was hospitalized in the ICU with a multilumen central venous catheter in his right jugular vein to facilitate fluid and drug therapy. On hospital day 5, he developed a fever of 103.4° F, hypotension, neutropenia, and acute kidney injury. HAI was suspected based on the patient’s acute clinical signs and biochemical changes consistent with severe sepsis.6
Common hospital-acquired infection sites include the respiratory and urinary tracts, surgical incisions, and the bloodstream.
Pneumonia, surgical site, urinary tract, and catheter-related bloodstream infections (CR-BSIs) are the most common HAIs.3,7,8 In this patient, on hospital day 5, the central venous catheter insertion site was erythematous with purulent discharge. Jugular vein palpation suggested thrombosis, which was ultrasonographically confirmed. Additional diagnostic results, including surgical incision inspection, thoracic radiographs, thoracic fluid cytology and culture, and urinalysis with culture, were negative. The patient was diagnosed with CR-BSI.
Related Article: Step-by-Step: Peripheral Catheter Placement
According to the Infectious Diseases Society of America (IDSA) guidelines, blood should be collected for culture in critically ill humans (ie, with hypotension and/or organ failure) who have acute onset of fever and suspected CR-BSI.4 Additionally, all IV catheters should be removed and replaced only as necessary.4 A CR-BSI diagnosis requires paired positive quantitative catheter tip and peripheral blood cultures.9-11
Quantitative culture is performed via sonication of the distal 5 cm of catheter. Sonication is the application of sound waves (55 000 Hz) to a catheter segment submerged in culture broth, thus dislodging bacteria from the catheter surface for plating on agar after serial dilution.12,13 Catheter sonication dislodges bacteria from the extra- and intraluminal surfaces and may dislodge bacteria within a biofilm.4 As colonization of the intraluminal surface is likely the most common source of CR-BSI, sonication is the recommended method of catheter tip culture.
Definitive diagnosis of CR-BSI requires a positive quantitative culture of >103 colony-forming units (CFUs) per catheter segment if the same organism is cultured from peripheral blood.4,9 The greater the number of CFUs obtained from a positive (>103 CFU) catheter culture, the greater the likelihood blood cultures will be positive for the same organism.13,14
Related Article: Protecting the Immunocompromised Patient
The semiquantitative roll plate catheter technique is also an acceptable method of diagnosing CR-BSI, but can result in false-negative results in cases of intraluminal catheter colonization.15-17 Bacteria are cultured from the extraluminal surface in the roll plate technique via rolling the catheter tip on an agar plate.18
A cutoff of >15 CFU distinguishes contaminated catheters from colonized catheters, and >1000 CFU is correlated with CR-BSI caused by the same organism.18 In humans with short-term catheters (ie, indwelling for <7 days), the roll plate technique is superior for detection of catheter colonization.15
Related Article: Biosurveillance: How to Monitor Disease Trends
In this patient, the catheter tip and peripheral blood were cultured according to IDSA guidelines.4 Cytologic examination and gram staining of purulent discharge from the insertion site showed suppurative inflammation with intracellular gram-positive cocci and gram-negative rod bacteria.
Treatment & Outcome
Amanda A. Cavanagh, DVM, DACVECC, Colorado State University
Treatment
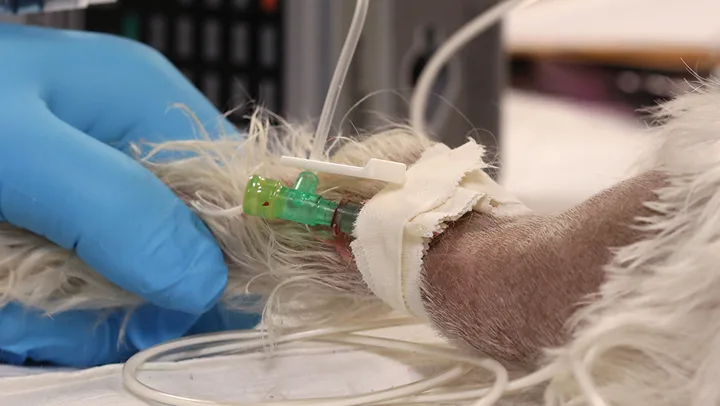
Using aseptic technique during placement and access of IV catheters can help prevent bacterial colonization and CR-BSI. (See Table 1.) IV catheters should be inspected daily as part of CR-BSI surveillance. Because this patient was diagnosed with CR-BSI, the central venous catheter was removed and replaced with a short peripheral IV catheter in the cephalic vein for continued parenteral therapy.
Related Article: Skills for Veterinary Technicians: IV Catheter Placement
Prevention of CR-BSI
Empiric antibiotic therapy was initiated based on evaluation of the hospital’s antibiogram, an annual antimicrobial susceptibilities summary of bacterial isolates submitted for culture from patients hospitalized within the institution.19,20 The antibiogram showed that multidrug-resistant Escherichia coli and Enterococcus spp were the most common nosocomial pathogens. Both pathogens had common susceptibility limited to carbapenem antibiotics and doxycycline. Doxycycline is a bacteriostatic antibiotic with a limited activity spectrum, so carbapenem treatment was initiated.21
Using aseptic technique during placement and access of IV catheters can help prevent bacterial colonization and catheter-related bloodstream infections.
Catheter and blood cultures at 72 hours grew Escherichia coli with an extended spectrum β-lactamase resistance pattern and multidrug-resistant Enterococcus faecalis. Both pathogens were susceptible to imipenem, a carbapenem antibiotic, so antimicrobial treatment was continued. The patient also required norepinephrine for 24 hours after initiation of antibiotics to maintain adequate blood pressure.
Veterinarians must be familiar with resistance patterns of hospital-acquired pathogens within their practice to select empiric antibiotics responsibly. The Surviving Sepsis Campaign recommends initiating antimicrobial therapy with a broad activity spectrum against all likely pathogens within the first hour after septic shock identification.4,6 Failure to begin appropriate antimicrobial therapy promptly significantly increases morbidity and mortality.<sup6 sup>
Failure to begin appropriate antimicrobial therapy promptly significantly increases morbidity and mortality.
HAIs in humans can originate from endogenous (eg, gastrointestinal tract) or exogenous sources (eg, contaminated fomites, caregivers’ hands).3 Gram-negative bacteria are the most common pathogen associated with CR-BSI in humans and dogs; antibiotic resistance has increased significantly during the past decade among gram-negative nosocomial bacteria, particularly in ICU settings.22-29 Prophylactic antibiotic use has not been shown to decrease CR-BSI,30 and routine catheter replacement does not decrease CR-BSI risk.31
Related Article: Antibiotic Resistance: The Veterinary Fight Against a Post-Antibiotic Era
Judicious use of antibiotics is an effective strategy for reducing antibiotic resistance; however, critically ill patients in septic shock have little systemic reserve to tolerate ineffective antimicrobial choices, so initial antibiotic restriction is inappropriate.6 As culture results become available, antibiotic de-escalation tailored to the causal pathogen is appropriate.6
Outcome
The patient recovered with no persistent renal injury. Because the causal pathogens had susceptibility patterns identical to those cultured from the hospital environment, the source of contamination was most likely the catheter, catheter hub, or veterinary team members’ hands.
Team Management
Carlee Fiddes, PSM, BS, AAS, LVT, Colorado State University
Adoption of hospital-cleaning protocols and standard operating procedures (SOPs) for clinical tasks enables all members of the veterinary team to take an active role in decreasing the incidence of hospital-acquired infections (HAIs).1
Example SOP for Central IV Catheter Placement & Management
Wearing clean gloves, shave the catheter insertion site with a 1-inch minimum margin on each side; ideally, shave the full circumference of the leg. Clean the insertion site with a 2% chlorhexidine solution applied in concentric circles starting near the intended insertion site and extending away from the site.9 Chlorhexidine must have 5 minutes of contact time to be effective. Dry the area with sterile dry gauze.10
Wash hands, don a surgical mask, gown, and cap or hair net, and apply sterile gloves using the open-handed technique.11
Ask assistants to restrain the patient and occlude the vein for catheter placement while maintaining a sterile field. A sterile drape may be used for this purpose.
Place the IV catheter, attach the catheter cap/t-port, and secure and cover the catheter according to hospital protocol. Do not remove gloves until the catheter insertion site is completely covered and the catheter cap/t-port has been attached.
Monitor the catheter insertion site and surrounding area daily for infection signs. Wear gloves to palpate the site. Do not uncover the catheter insertion site unless infection is a concern.
Wear gloves when administering all IV medications and when connecting or disconnecting fluid lines. Use new, sterile needles for all injections. Swab injection ports with alcohol and let dry before use.12,13
Every practice should develop hospital-cleaning policies all team members must follow.
Establish cleaning protocols to ensure all reservoirs for potential pathogens in the hospital are cleaned regularly, including scrub containers, cleaning-spray bottles, blankets, mops, brooms, floors, trash cans, sinks, counters, and ventilator equipment.
Establish SOPs that promote aseptic technique for procedures such as peripheral IV, central venous, arterial, and urinary catheter placement; fluid line maintenance; and surgical preparation.2 (See Example SOP for Central IV Catheter Placement & Management.)
Wear clean gloves for peripheral IV catheter placement and fluid line maintenance. Follow full sterile barrier technique (eg, cap, mask, sterile gloves and drape) for urinary catheterization and central venous and arterial catheter placement.<sup3 sup>
Train all veterinary team members to ensure adherence to protocols and SOPs.
Run an annual antibiogram for the hospital. An antibiogram is an overall profile of antibiotic sensitivity for a particular organism; for example, of the 273 cases of Escherichia coli treated in our hospital, 91% responded to ciprofloxacin, 24% to ampicillin, and 76% to ampicillin–clavulanate. The antibiogram will identify pathogens present in the local area and help guide veterinarians when choosing empiric antibiotics. If the practice does not collect adequate culture and sensitivity data to produce meaningful results, collaborate with other area practices to create a regional or community antibiogram.
The World Health Organization (WHO) provides a free Microsoft Windows-based program called WHONET to help veterinary practices create antibiograms using data collected from cultures. (The clinical testing laboratory used by a practice can help prepare culture information for use in WHONET.)
Related Article: Safety Protocols in Practice
An antibiogram (ie, an overall profile of antibiotic sensitivity for a particular organism) will help when choosing empiric antibiotics.
Every team member must follow established protocols and SOPs when treating every patient.
Follow hospital protocols for all procedures, including urinary and IV catheter placement, and surgical site preparation.
Remove a catheter that was not placed aseptically or has hair near the insertion site within 48 hours.4 A catheter placed aseptically can be left in place for up to 10 days if no signs of infection are present.5
Wash hands frequently. Soiled hands should be washed with soap and water; clean hands should be decontaminated with an alcohol- based hand rub. Perform hand hygiene before and after handling the catheter, and wear gloves each time the catheter is accessed.6,7
Monitor the patient daily for infection signs (eg, heat, pain, redness, swelling, discharge) at surgical, catheter insertion, and urinary catheter sites. Palpate catheter insertion sites through dressings, and only remove dressings if infection is a concern.
Monitor temperature, respiration, and heart rate, and auscultate heart and lung sounds on all hospitalized patients at regular intervals.8 The frequency of these intervals may vary with the patient or hospital but are often the first way to detect a change in patient status, including sepsis. Discuss any changes and concerns with the veterinarian.