Heartworm Infection in Cats
Clarke E. Atkins, DVM, Diplomate ACVIM (Internal Medicine/Cardiology), North Carolina State University
Profile
Definitions
Cats infected with Dirofilaria immitis, with or without clinical signs, are defined as having heartworm infection (HWI). If clinical signs (eg, historical, physical, radiographic) are present, then the syndrome is defined as heartworm disease (HWD). Heartworm infection may also be referred to as dirofilariasis or dirofilarosis.
Heartworm-associated respiratory disease (HARD) refers to respiratory signs associated with HWD that may indicate mature, immature, or aborted infection. When associated with infections that fail to reach maturity (aborted), this syndrome has been referred to as pulmonary larval dirofilariasis since immature L5 (early 5th-stage larvae; also termed young adults) produce disease in the pulmonary arteries, and probably, on the basis of experimental infections, alveolar and bronchial lung disease.
Incidence/Prevalence
The feline prevalence is generally believed to approximate 10% of the unprotected canine prevalence in any given region. This percentage varies with the predominant mosquito species in a region because feline infection requires a species that feeds on both cats and dogs. Figures 1 and 2 demonstrate the proven prevalence in cats by necropsy and by exposure, respectively. Although only 10% to 20% of exposed cats have mature HWI, it is important to remember that all these antibody-positive cats are at risk for pulmonary larval dirofilariasis.
Geographic Distribution
Feline HWI is recognized wherever canine HWI is prevalent, particularly in the southeastern United States and the Mississippi River Valley (Figure 3). HWI has been diagnosed in cats in most states.
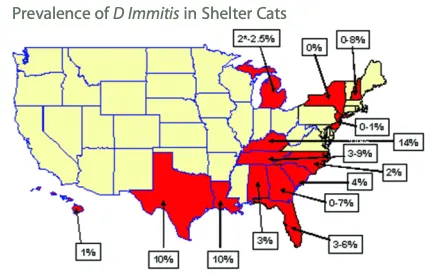
FIGURE 1
Necropsy prevalence of heartworm infection in shelter cats. The shaded states are those in which such studies have been completed. One Michigan study, which showed a prevalence of 2%, was an antigen study.
Signalment
Age and Range
Cats of any age may be infected with D immitis. The median age at diagnosis is approximately 6.5 years. Clinical signs may be recognized within 3 to 4 months (pulmonary larval dirofilariasis) to 7 to 8 months for mature infection.
Gender
Male cats are thought to be at greater risk due to outdoor roaming habits. In addition, experimental infections produce heavier infections in male cats than in females despite equal larval exposure.
Causes & Risk Factors
Risk factors for cats include male gender, short hair coat, and outdoor exposure. Of course, the risk is increased in highly endemic heartworm areas and in situations where neighborhoods have a high prevalence due to standing water or low socioeconomic conditions. Immunosuppression is associated with human HWI, but to date, cats with feline leukemia or feline immunodeficiency virus have not been shown to be predisposed.
Pathophysiology
As in the dog, immature adult heartworms (also termed immature L5) may create pulmonary and pulmonary vascular disease in cats prior to maturation. Uniquely, the disease process develops even in cats that ultimately resist mature infection. A severe myointimal and eosinophilic response produces pulmonary vascular narrowing and tortuosity, thrombosis, and possibly hypertension.
Although uncommon, cor pulmonale and right heart failure can be associated with chronic feline HWD. Right heart failure is manifested by pleural effusion (hydro- or chylothorax) or ascites. The lung itself also is insulted by HWI, with eosinophilic infiltrates in the lung parenchyma (pneumonitis) and pulmonary arteries. The pulmonary vessels may leak plasma, producing pulmonary edema (possibly acute respiratory distress syndrome) and type II cell proliferation, both potentially altering oxygen diffusion. In addition, radiographic findings suggest air-trapping, compatible with bronchoconstriction.
The end result to this multifaceted insult is diminished pulmonary function, hypoxemia, dyspnea, cough, and even death. Recently, a symbiotic bacterium, Wolbachia, has been found within filarid parasites and their microfilariae. This bacterium is essential for filarial reproduction and well-being. It has been hypothesized that antigens from these bacteria are proinflammatory, contributing to HWD (particularly upon the death of the adult heartworm) and that tetracycline might be a possible treatment strategy for adult dirofilariasis.
Signs
History
Historical findings range from none (28% of cats diagnosed with HWI infection have no signs related to this syndrome) to fulminant respiratory failure and death. The most common signs are those associated with the respiratory tract (coughing, wheezing and dyspnea). Clinical signs are listed in the Table.
Physical Examination
Signs may range from mild wheezing and coughing to profound dyspnea and respiratory collapse. Vomiting is frequently recognized in cats with HWI, but the mechanism is unclear. Neurologic signs (eg, seizures, blindness, paresis/paralysis), due to aberrant worm migration to the brain, eye, or spinal cord are also noted. Heart failure, if present, is typically associated with dyspnea, abdominal distention, diminished lung sounds, and fluid line evident by percussion, jugular venous distention, tachycardia, ashen mucous membranes, and weak pulses. A heart murmur or gallop may be present.
Diagnosis
Definitive Diagnosis
Dirofilariasis (mature HWI) in cats can be diagnosed definitively by several means. Necropsy is considered the gold standard. However, antemortem diagnosis can be assumed with a positive microfilaria test (modified Knott or Millipore filter technique), positive antigen test (indicates mature adult female worms are present), and echocardiographic parasite identification by someone with expertise in this area.
Pulmonary larval dirofilariasis (HARD) is diagnosed by the clinical finding of respiratory signs, antibody-positive status, and suggestive radiographic findings. By definition, these cats will be antigen-negative and will not have worms identifiable by echocardiography.
Presumptive Diagnosis
The antigen test recognizes fewer than 50% of cases because of low female worm burden or immature infection. Consequently, the diagnosis must often be made on a combination of clinical findings (eg, cough or dyspnea), antibody-positive status (indicating exposure, with larval development to the L4 stage and possibly beyond), and radiographic findings.
Laboratory Findings
Eosinophilia is noted in approximately 33% of cases, with occasional basophilia.
Radiographic FindingsRadiographic changes (Figure 4) are variable and inconsistent, with the most common finding being enlargement of the caudal lobar pulmonary arteries (> 1.6¥ the diameter of the 9th rib at the 9th intercostal space). Pulmonary arteries often have ill-defined margins, and pulmonary parenchymal changes include focal or diffuse infiltrates (interstitial, bronchointerstitial, or even alveolar), perivascular density, and occasionally atelectasis. Pulmonary hyperinflation may also be evident.

Dorsoventral thoracic radiograph from cat with heartworm disease. Changes are not dramatic but the right caudal lobar pulmonary artery is enlarged (> 1.6× the diameter of 9th rib at the 9th intercostal space; arrows). The opposite pulmonary artery is somewhat tortuous.
Echocardiographic FindingsRight ventricular hypertrophy may be observed but the echocardiogram is most often normal. Adult heartworms, observed as double-walled (railroad track) echoes (Figure 5) are seen most often in main, right, and left pulmonary arteries, but also in the right ventricle and atrium.

A short-axis, 2-dimensional echocardiogram obtained from an 18-year-old castrated male, feline cancer patient with a cardiac murmur. An adult heartworm can be identified as 2 echo-dense parallel lines in the right pulmonary artery (arrow).
Ao=aorta; RPA=right pulmonary artery; LPA=left pulmonary artery
Postmortem Findings
Mature or immature heartworms are found in heart and pulmonary arteries. Right ventricular hypertrophy and thickened, roughened pulmonary arteries may be noted. Histologic findings include intimal and medial pulmonary arterial hypertrophy with obstruction and eosinophilic infiltrate in alveolar septae, pulmonary interstitium, and bronchi.
Treatment
Inpatient or Outpatient
Most patients are handled as outpatients; however, if severe dyspnea due to respiratory disease or heart failure is present, hospitalization and oxygen are employed on an inpatient basis.
Medical Therapy
The general medical approach to therapy, based on specific signs, is outlined in the Tx at a Glance box.
It should be recognized that there are 2 basic approaches: one that attempts to rid the cat of HWI and one that is based on allowing the worms to live as long as possible because worm death is often cataclysmic for the patient. I use an "in-between" approach in most cases, choosing to prevent future infection, gradually killing the heartworms or allowing them to die naturally, and treating clinical signs should they develop.
Surgical Therapy
Surgical removal of worms provides the advantage of clearing the patient of heartworms without concern of thromboembolic complications, thus potentially effecting a cure. Unfortunately, this is neither practical nor inexpensive and may result in cataclysmic results if worms are broken during extraction. My colleagues and I have had success using a nitinol snare under fluoroscopic guidance to extract worms via the jugular vein.
Nutritional Aspects
Other than an overall good nutritional plane, the only nutritional goal would be to limit salt intake in animals with congestive heart failure. This might include a "senior" or "heart" diet.
Client Education
It is important that owners understand that cats with HWI but no clinical signs are viewed as potential "time bombs" in which severe respiratory signs and even death may occur with little warning. Another key client information note regarding HWI is that this syndrome is far better prevented than treated and that many effective preventatives exist.
Medications
Drugs
Cats without clinical signs
Heartworm preventative administered as chewable tablet, flavored tablet, or topically, with varying spectra for endo- and ectoparasites. I place both cats with and without clinical signs on preventive therapy.
Ivermectin (monthly chewable)
Milbemycin oxime (monthly tablet)
Moxidectin/imidacloprid (monthly topical)
Selamectin (monthly topical)
Aspirin to reduce pulmonary thrombosis
Adulticidal therapies
None approved
Ivermectin at preventive dosages (24 mcg/kg monthly) may hasten worm death while preventing future infection. There is, however, no proof of this effect in cats.
Tetracycline at 5 to 10 mg/kg Q 12 H may hasten worm death by killing Wolbachia; however, there is no proof of this effect in cats.
Respiratory signs (cough, dyspnea, wheezing) due to pulmonary inflammation
Prednisolone or prednisone is used to manage respiratory signs, tapering to a dosage of 50% at 2 weeks and then terminating at approximately 1 month. If signs recur, alternate-day corticosteroid therapy (at the lowest dosage that controls signs) can be continued indefinitely.
Bronchodilators are occasionally used in cats with refractory asthma-like signs.
For respiratory emergencies, administer corticosteroids (dexamethasone or prednisolone sodium succinate), 40% oxygen therapy (administered in cage, hood, or nasal tube) and bronchodilators (aminophylline or terbutaline).
Respiratory signs or ascites due to heart failure
Thoracocentesis or abdominocentesis
Furosemide to prevent fluid reaccumulation
Enalapril or benazepril
Quercetin-3-rutinoside if thoracic fluid is chylous
Other signs (vomiting, central nervous system signs)
Symptomatic therapy
Antiemetics
Anticonvulsants
Prednisolone or injectable corticosteroids, as previously described
Precautions
Aspirin therapy can cause vomiting and inappetence. Use of such off-loading therapies as diuretics and angiotensin-converting enzyme inhibitors can cause hypotension in a small percentage of patients.
Interactions
Drug interactions are always a concern when polypharmacy is employed. The biggest concern in the treatment outlined is the use of aspirin and corticosteroids (prednisolone) together. This should be avoided.
Follow-Up
Patient Monitoring
Patients with HWI should be monitored based on disease severity. Cats without clinical signs may be only monitored twice yearly, while those in heart failure may require more frequent monitoring. Monitoring might include only physical examination, or thoracic radiographs may also be needed. Repeated antigen and antibody tests are not necessary except to determine if an infection has passed. The antibody test will remain positive if exposure to heartworms continues (ie, if L4 develop within the cat) even if the cat is now protected with one of the monthly preventatives.
Prevention
Prevention of HWI is advised in all cats in endemic areas, even if totally indoors. Year-round prevention is ideal, particularly in heavy heartworm endemic areas. Cats with HWI should be placed on a preventative to avoid recurrent infection.
Complications & Course
Complications include recurrent cough and asthma-like signs, pulmonary thromboembolism, fulminant respiratory failure, right-sided heart failure, and sudden death.
HWI does not always end fatally. The clinical course is quite variable and not well understood. Cats may remain free of clinical signs and die of other causes. Most cats with clinical signs demonstrate respiratory signs or vomiting. Respiratory signs are now believed to begin within 3 months of infection, with larval (immature L5 or immature adult) death occurring both in cats that ultimately develop mature infections and in those that do not.
In cats that develop mature infections, clinical signs often follow a waxing and waning course. These cats occasionally develop heart failure. Catastrophic respiratory failure (which may be fulminant) may result from pulmonary thromboembolism, thrombus formation, or worm death (spontaneous or iatrogenic).
In General
Relative Cost
Diagnostic workup: $$
Treatment of uncomplicated disease: $
Treatment of complicated disease: $$-$$$
Cost Key
$ = <$100
$$ = $100-$250
$$$ = $250-$500
$$$$ = $500-$1,000
$$$$$ = >$1,000
(Actual costs will have regional variations)
Prognosis
The prognosis for HWI has been studied. The median survival is 1.5 years, with an approximate average longevity of 8 years of age. If cats survive beyond day 1, the median survival is 4 years, with an average longevity of 10.5 years. At least 22% (and possibly more than 75%) of infected cats survive infection.