Feline Degenerative Joint Disease Part 1: Diagnosis
Profile
Definition
Degenerative joint disease (DJD) is a term that loosely encompasses various arthropathies, including:
Osteoarthritis (OA)-disease of synovial joints characterized by loss of articular cartilage, osteophyte formation, bone remodeling, and inflammation
Spondylosis deformans-disease involving fibrocartilagenous intervertebral joints of the spine characterized by development of bony spurs.
For the purposes of this article, both forms will be considered together.
Related Article: Treatment of Feline Degenerative Joint Disease
Systems. Musculoskeletal, focusing on inflammation within joints and surrounding soft tissues. Bony changes are part of the cause and effect.
Genetic Implications. Some breeds of cat are at greater risk for hip dysplasia (eg, Maine coon) or patellar abnormalities (eg, Abyssinian), but breed predisposition for osteoarthritis has not been thoroughly studied.
Incidence/Prevalence. DJD and/or OA are extremely common in cats, increasing in frequency with age. Hardie, et al reviewed 100 radiographs of cats (older than 12 years) taken as part of diagnostic workups for multiple reasons and found that 90% had evidence of DJD.1 Godfrey performed a retrospective radiographic study on cats of all ages and found radiographic changes suggestive of OA in 22% of cats, with 33% of those showing clinical signs.2 In a third study (Clarke, et al) the prevalence of radiographic signs of DJD or OA in 218 cats was 33.9%, with 16.5% (mostly cats older than 10 years) exhibiting clinical signs.3
Geographic Distribution. Worldwide
Signalment
Age and Range. Most patients are older than 10 years (see Incidence/Prevalence)but all ages can be affected. DJD should be a consideration in any lame patient or cat that is moving less than it had been. Cats with OA are less likely than dogs to show true lameness (see History).
Gender. There is no gender predilection. Whether neutering plays a role is unknown.
Causes and Risk Factors
The incidence of OA or DJD appears to be more common than previously thought and is probably a major cause of discomfort in older cats. A statistically significant association exists between increasing age and radiographic DJD changes. Secondary osteoarthritis may be caused by:
Joint trauma (eg, fractures or ligamentous injuries)
Infectious or immune-mediated inflammation
Compensation for congenital or developmental neoplastic, endocrine (diabetic), or metabolic conditions.
Pathophysiology
OA involves a cascade of mechanical and biochemical events resulting in articular cartilage deterioration, synovial membrane inflammation, soft tissue changes, osteophyte formation, and bone remodeling (including at the subchondral level).
Signs
History. The hip and elbow are the most commonly affected joints.3,4 Lameness is not typically a clinical sign of DJD; rather, the signs are insidious or incorrectly attributed to aging, including:
Inappropriate elimination (outside the litter box)
Decreased grooming
Developing antipathy for being combed
Reluctance to jump up or down
Sleeping more, moving less
Withdrawing from human interaction
Hiding.
As cats age, their previously flexible spines become stiffer as a result of spondylosis deformans. When these bony protrusions or additional changes to coxofemoral or stifle joints make it difficult for a cat to squat in the litter box, the animal may urinate or defecate immediately outside the box. In addition, stiffness of the spine can make it difficult for a cat to twist to groom the caudal parts of its body. Matting or unkempt hair may be a clue suggesting further orthopedic evaluation, such as radiographs, is necessary.
Careful and thorough questioning by the clinician (see Client Questionnaire) will help determine whether these signs indicate DJD.
Physical Examination. Cats are generally less cooperative than dogs or horses with having their gait assessed. With patience, a full orthopedic exam can be performed on some cats. Radiographic assessment is generally required to evaluate any lameness noted by the client because it is difficult to assess voluntary movement and because passive movement may be protected/guarded in cat that is experiencing pain. Home video can be useful to assess gait.
Pain Index
Given that one may be able to elicit a painful response in a sedated cat with OA and considering research on pain in cats with OA,5 it appears that cats suffer varying degrees of discomfort without our being aware of it. As in dogs, the clinical signs of OA do not correlate well with radiographic findings. Interestingly, medical records in only 4 patients in the Hardie study1 noted client concern about reduced activity or lameness (see Recognizing Pain in Cats).
Client Questionnaire
Diagnosis
Definitive Diagnosis
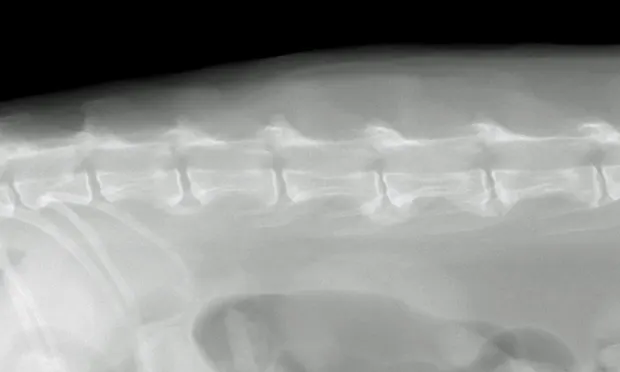
For conclusive proof of osteoarthritis, look for radiographic signs supportive of the loss of articular cartilage, osteophyte formation, bone remodeling, and inflammation along with cytology of joint fluid showing increased inflammatory cell counts and protein levels and decreased viscosity of fluid (see Laboratory Findings/Imaging for further discussion). Spondylosis deformans is diagnosed radiographically by identifying bony spurs of the fibrocartilagenous intervertebral joints of the spine (Figures 1 and 2).


Differential Diagnosis
Causes are multiple and can be primarily classified according to the DAMNIT scheme of disease etiology:
Degenerative: Can cause multifocal lesions that are usually chronic and progressive, but may wax and wane or improve in obese individuals upon weight loss
Anomaly: Present at birth, may or not be progressive (eg, achondroplasia, storage diseases, hip dysplasia, patellar luxation, hemivertebrae)
Metabolic: Chronic, progressive (eg, diabetes mellitus)
Nutritional or neoplastic**:** Chronic, progressive course (eg, vitamin A toxicosis, primary osteosarcoma, metastatic bronchogenic carcinoma)
Inflammation, infectious, or immune-mediated: Often a chronic, progressive course (eg, myasthenia gravis, postvaccinal calicivirus lameness [limping kitten syndrome]). Bacterial joint infection must be ruled out if unilateral limping is present.
Trauma or toxicity: Acute and nonprogressive (eg, fracture, periosteal bruise, ligamentous strain, muscle sprain). Toxicity may be acute and progressive or chronic and progressive (eg, lead).
Vascular: Acute and nonprogressive (eg, Legg-Perthes disease, thrombo-embolic disease)
Recognizing Pain in Cats6,7
Laboratory Findings/Imaging
Radiographs of DJD will depict bone spurs, osteophytes, joint surface lucencies, or narrowed joint space reflecting loss of articular cartilage. There is generally no increase in volume of joint fluid associated with degenerative conditions; however, joint space may be wider than normal if severe inflammation is present.
Color and turbidity of synovial fluid in a degenerative joint is usually normal; viscosity is normal or slightly decreased. There are normal to slightly increased numbers of nucleated cells, with a possible increase in percentage of macrophages. Neutrophils may range from low to high in DJD, as opposed to a typical marked increase in inflammatory arthropathies.
In General
Relative Cost
Physical examination and radiographs: $$$
Minimum database for the older cat (complete blood count with differential, serum biochemical panel, urinalysis, and blood pressure evaluation): $$$
Prognosis
Fair to guarded, depending on concurrent diseases and potential complications from therapy. DJD is a condition that usually remains stable for long periods of time.