Ehrlichiosis in Dogs
Profile
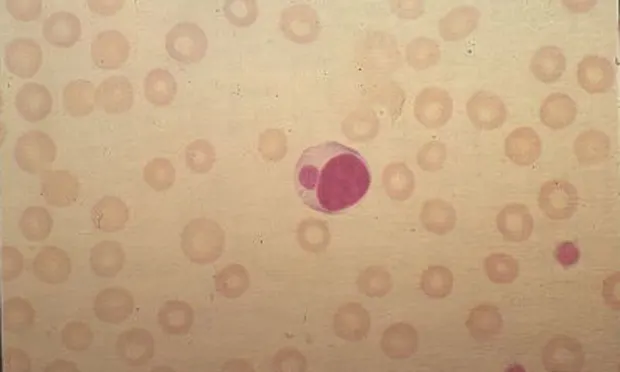
DEFINITIONCaused by small, pleomorphic, gram-negative, coccoid bacteria that are obligate intracellular parasites (Table). Bacteria appear intracytoplasmically in clusters called morulae (Figure 1) and can be divided into three classes based on whether they infect mononuclear cells, granulocytes, or thrombocytes. Ehrlichia canis is the species most often associated with canine ehrlichiosis, but other species also cause natural infection. Molecular technology has resulted in reclassification of Ehrlichia species, and terminology is always changing:1 e.g., E. equi, human granulocytic ehrlichiosis, and E. phagocytophila are now collectively recognized as Anaplasma phagocytophila.
Figure 1. (above) Figure 1. Morulae of an Ehrlichia canis organism in a mononuclear cell.
Systems. Lymphoreticular, neuromuscular, ophthalmic, joint, and hematopoietic systems can be affected, therefore making diagnosis a challenge (Signs).
Incidence/prevalence/geographic distribution. Depend largely on prevalence and geographic distribution of vector and reservoir hosts for specific Ehrlichia species (Table). Practitioners must know prevalence in their own regions. In regions enzootic for E. canis, up to 25% of asymptomatic dogs may have serum antibodies.2 True incidence for all ehrlichiosis is not known.
SIGNALMENT/RISK FACTORSAll dogs are potentially susceptible to Ehrlichia infection. Reinfection can occur. Dogs receiving blood transfusions from unscreened donors may have increased risk, especially if donors reside in enzootic regions. No breed, age, or sex predilection exists, although German shepherds may be more susceptible than other breeds, especially for the severe chronic pancytopenia form.3
PATHOPHYSIOLOGYInfection occurs when an infected tick ingests a blood meal and salivary secretions contaminate the feeding site. The incubation period is 8 to 20 days. Vasculitis and immune mechanisms are involved in the pathogenesis of ehrlichiosis.4
S**IGNS**History. Depression, lethargy, mild weight loss, and anorexia with or without bleeding are common. Owners may notice dermal petechiae and/or ecchymoses. Bleeding can occur from any mucosal surface, but epistaxis is most frequent. Change in eye color, blindness, lameness, stiff-stilted gait, and neck pain may also be present. Course can be divided into acute, subclinical, and chronic phases, but accurate staging is difficult. Two- to 4-week acute phase often goes unnoticed but is characterized by fever, oculonasal discharge, anorexia, depression, petechiae, ecchymoses, and lymphadenomegaly/splenomegaly. Thrombocytopenia may persist in subclinical phase, which can last for months/years. Dogs may eliminate rickettsia or may remain carriers for life or enter chronic phase, which in severe form results in pancytopenia with grave prognosis.
Physical examination. One or all of the following may be found: petechiae/ecchymoses (50%); polyarthropathy with multiple painful joints/effusion (more likely with granulocytic species and may be as high as 90%); lymphadenomegaly/splenomegaly (20% to 25%); pale mucous membranes (45%); stiff-stilted gait with neck/muscle pain (rare); anterior uveitis (8%); and retinal hemorrhage with or without detachment (8%). Thus, tick-borne diseases can be "great imitators" of other diseases.
DIFFERENTIAL DIAGNOSISBecause of its multisystemic nature, the list is long. As a general rule, infectious, immune-mediated, and neoplastic diseases are those that are usually mistaken for ehrlichiosis. See algorithm on page 30 for diagnostic approach to petechiae/ecchymoses.
LABORATORY FINDINGS/DIAGNOSISUsually based on a combination of clinical signs, hematologic abnormalities, thrombocytopenia, and serologic findings (Clinicopathologic Findings). There is no "gold standard" definitive test.
Thrombocytopenia has often been used for ehrlichiosis screening; thus, the percentage could be overestimated. Ehrlichiosis should never be ruled out because platelet count is normal. Also, in the author's experience, ehrlichiosis is rarely found in conjunction with platelet counts less than 20 to 30 thousand/µl. If count is extremely low, other causes should be strongly considered. Granular lymphocytosis, monoclonal gammopathies, and plasmacytosis of bone marrow are more common with neoplastic diseases, but in a region enzootic for ehrlichiosis, further tests should be done if these disorders are present. Cytologic studies showing morulae in white blood cells of blood smear, CSF, or joint fluid (Figure 2) may provide definitive diagnosis, but this is unusual.
Figure 2. Morulae of an Ehrlichia ewingii organism found in a neutrophil from joint fluid.
Serologic testing/PCR/immunoblotting. IFA or ELISA is used. Seroconversion usually occurs 7 days after exposure but may take 28 days. In the natural setting, almost all clinically ill dogs seroconvert by that time. Species-specific antibody testing is necessary. One Ehrlichia antibody test does not react with all Ehrlichia antibodies. In enzootic areas, although serologic tests may be positive the clinical signs may be due to another condition. Be aware of the test's limitations. Also, successfully treated dogs can retain positive and even high titers for years. A recently marketed "point-of-care" in-clinic ELISA test for E. canis antibodies (SNAP 3Dx-IDEXX Laboratories Inc., Westbrook, ME) yielded positive results at a dilution of 1:100 or greater. A similar in-house ELISA has been developed in Israel (Immunocomb-Biogal, Kibbutz Gal'ed, Israel). These tests have good specificity and sensitivity. Their primary utility, in the author's opinion, is screening dogs for which the practitioner has a strong suspicion of E. canis infection.5 If a dog has active clinical ehrlichiosis, it is unlikely the test would be negative. Thus, negative results probably rule out E. canis infection in most cases (although infection with other Ehrlichia species would still be possible).
PCR and western immunoblotting have been used in research to characterize and distinguish between species of Ehrlichia but have not provided "significant" benefit in the clinical setting. The western blot yields results in the same time frame as IFA or ELISA, and the PCR on blood has not proven to be very sensitive. In one study, only 13 of 49 (27%) naturally infected IFA-positive dogs had positive results for E. canis on PCR.6 In summary, diagnosis is still based on a combination of clinical signs, clinicopathologic abnormalities, and serologic testing.
Postmortem findings. Characteristic histopathologic findings are perivascular plasma cells or lymphoplasmacytic infiltrates in multiple organs (lungs, brain, meninges, kidney, lymph nodes, bone marrow, spleen, and skin). Morulae are infrequently observed in tissue at necropsy.
Treatment
Most dogs can be treated as outpatients. Effective drugs include tetracyclines, doxycycline, chloramphenicol, and imidocarb dipropionate. Doxycycline is the most commonly used agent. The current recommendation is to treat for 3 to 4 weeks (Tx at a glance). The sooner treatment is initiated, the more favorable the prognosis. It is difficult if not impossible to cure dogs in the severe chronic stage (bone marrow suppression). The fluoroquinolones, which are effective against Rocky Mountain spotted fever and some species of Ehrlichia, do not seem to be effective against E. canis infection.7 In addition, recent evidence has also questioned the clinical effectiveness of imidocarb dipropionate.8
Supportive therapy with fluids for dehydration and blood transfusion if the dog is severely anemic (PCV < 20%) may be justified, but routine transfusion will not significantly increase the platelet or neutrophil count. Data on use of such growth factors as erythropoietin (Epogen-Amgen, Thousand Oaks, CA) or granulocyte colony-stimulating factor (Neupogen-Amgen, Thousand Oaks, CA) as adjunctive therapy are limited. However, a single case report suggests they might be useful for severe chronic ehrlichiosis.9 Short-term treatment (2 to 7 days) with glucocorticoids may be beneficial early in treatment because immune-mediated mechanisms may be involved. Such treatment may be more important for dogs with polyarthropathy, meningitis, and/or vasculitis.
Follow-up
Patient monitoring. Most dogs with acute ehrlichiosis begin to respond within 48 to 96 hours. Within 7 to 14 days, platelet count generally is normal. If not, another cause should be considered (e.g., immune-mediated thrombocytopenia). Coinfection with other tick-borne agents is increasing and should be considered.6 Platelet count should be performed at end of therapy and, in the author's opinion, again in 6 months. We have had a few research dogs in a tick-free environment that, after apparent successful therapy with doxycycline, developed recurrent thrombocytopenia and positive results on blood and splenic aspirate PCR 6 months later. Others have reported suboptimum long-term results with doxycycline.10 Serologic testing and blood PCR are not effective methods to assess therapy. In contrast to Rocky Mountain spotted fever, long-term immunity does not develop secondary to "successful" treatment or natural exposure, so reinfection is possible.11
Prevention. No vaccine is currently available; chemoprophylaxis and tick-control measures are primary means of prevention. Tetracycline is effective when administered daily at 6.6 mg/kg Q 24 H to dogs in enzootic or tick-infested areas. To date, the author is unaware that any Ehrlichia species has developed resistance to doxycycline. Maintaining strict tick-control programs for the dog and its environment is very important. The most effective products include fipronil,, imidacloprid/permethrin combinationb, and amitrazc.
Relative Cost of TreatmentUncomplicated $$Includes examination, diagnostic evaluation, treatment, and follow-up platelet counts.Complicated (bone marrow disease, severe anemia requiring blood transfusions) $$
Prognosis/Future Considerations
The question persists whether Ehrlichia is eliminated from the dog by treatment. In the natural setting, it is difficult to separate recrudescence from reinfection. As a general rule, the "straightforward" Ehrlichia patient (if there is such a thing) should have a positive response to doxycycline approximately 65% to 70% of the time without future problems unless reinfection occurs. Owners need to realize that reinfection is possible and measures to decrease exposure are extremely important.
Clinicopathologic Findings
Thrombocytopenia (82%)
Anemia (82%-usually nonregenerative)
Leukopenia (32%)
Pancytopenia (18% of chronic cases)
Granular lymphocytosis (has been reported)
Polyclonal gammopathies (occasionally monoclonal)
Bone marrow aspirates: plasmacytosis
Proteinuria, hematuria
Lymphocytic pleocytosis of cerebrospinal fluid (rare)
Neutrophilic inflammation of joint fluid (rare with E. canis; common with granulocytic species)
Prolonged buccal mucosal bleeding times (rare)
TX at a glance
Doxycycline: 5-10 mg/kg PO Q 12-24 H x 30 days
Tetracycline: 22 mg/kg PO Q 8 H x 30 days
Oxytetracycline: 25 mg/kg PO Q 8 H x 30 days
Minocycline: 10 mg/kg PO Q 12 H x 30 days
Chloramphenicol: 15-25 mg/kg PO Q 8 H x 30 days
Imidocarb dipropionate (Imizol-Schering-Plough, Kenilworth, NJ): 5 mg/kg IM once, repeat in 2-3 weeks.
Ehrlichiosis in CatsWhich species of Ehrlichia cause natural disease in cats is still a matter of great debate. However, seroprevalence studies have shown that cats can have circulating antibodies to Ehrlichia canis and Neorickettsia risticii.1 Ehrlichia DNA has been amplified from the blood of cats with PCR. On the basis of sequencing results, infection with Anaplasma phagocytophila and an E. canis-like organism seem to occur in naturally exposed cats.2,3