Cystocentesis: Lessons from 30 Years of Clinical Experience
Jody P. Lulich, DVM, PhD, DACVIM, University of Minnesota

Overview
Evaluation of urine provides useful information that facilitates rapid diagnosis, treatment, and prevention of many urinary and nonurinary disorders. Results of urinalysis are particularly helpful in verifying or eliminating diagnostic possibilities formulated on the basis of observations from the history and physical examination. For example, consider a dehydrated 12-year-old miniature schnauzer being examined for persistent vomiting. Evaluation of urine specific gravity facilitates localizing the underlying cause. Negative fluid balance in a dog with primary gastrointestinal disease but adequate renal function would be expected to promote compensatory renal tubular reabsorption of water in excess of solute from glomerular filtrate (i.e., formation of urine with a specific gravity greater than 1.030). However, if an inappropriate degree of compensatory urine concentration is observed (urine specific gravity < 1.030), secondary gastrointestinal disorders (e.g., renal, hepatic, and adrenal diseases and certain toxicities) are far more likely to cause vomiting than primary gastrointestinal diseases (e.g., gastritis, pyloric obstruction) or pancreatitis.
Emergency Application
The speed and economy with which urine specific gravity can be measured with a refractometer emphasize the usefulness of urinalysis in the emergency setting. Another example is ketoacidotic diabetes mellitus, which can be rapidly detected with a high degree of certainty by diagnostic reagent strips to detect glucose and ketones in urine. For these reasons, we routinely include urinalysis as part of the initial evaluation of all patients with systemic illness of unknown causes.
The urine collection method may vary depending on the tests selected, disease location, patient cooperation, and veterinarian experience (Table). However, cystocentesis has become the standard of practice for most clinical situations. It is easy to perform and well tolerated by patients. In addition, urine samples collected by cystocentesis are devoid of contaminants from the distal urogenital tract, thereby strengthening the validity of results. This article summarizes the steps necessary to safely perform diagnostic cystocentesis in dogs and cats.
Table: Method of Urine Collection Based on Patient Safety & Diagnostic Quality of Sample*
* P = preferable; A = acceptable; I = inadvisable
† Initial stream refers to the first portion of urine expelled, ensuring collection of urethral components.
Patient Considerations
To minimize iatrogenic trauma to the urinary bladder and adjacent structures and contamination of the urine sample with blood, routine cystocentesis should not be performed unless a sufficient amount of urine is in the lumen to permit localization and immobilization of the bladder by abdominal palpation. Blind cystocentesis without digital localization and immobilization of the urinary bladder is usually unsuccessful and increases iatrogenic risk. To reduce the likelihood of the patient voiding before urine collection, we advise owners to avoid situations that trigger urination in their pets. For example, small dogs can be carried from their car to the hospital and held until cystocentesis can be performed. Cats may be placed in a kennel without a litter pan several hours before urine collection.
Because insertion of a 22-gauge needle through the walls of the abdomen and urinary bladder is associated with little discomfort, tranquilization or anesthesia is rarely required. If needed, uncooperative patients resisting abdominal palpation or mild physical restraint may be more easily handled using distractive maneuvers or chemical sedation. Placing blankets or foam pads between the patient and the examination table may improve patient comfort and cooperation when it is restrained in dorsal or lateral recumbency.
Depending on the severity of dysuria, cystocentesis may not be feasible in cats with lower urinary tract disease. To facilitate urine collection, administer analgesia (e.g., buprenorphine 0.03 mg/kg, IV, IM, sublingual Q 8 H) 12 to 24 hours before cystocentesis. If cystocentesis is still not possible, a voided sample may have to suffice.
It may be difficult to palpate the urinary bladder of an obese patient. In this situation, ultrasonography may be used to guide the needle (discussed below).
If the urinary bladder does not contain sufficient urine, the patient may be given fluids or a diuretic. Although diuretics, such as furosemide (0.25 to 0.5 mg/kg IV or SC), may be used to rapidly increase urine production, alterations of urine specific gravity, pH, and other components of the urinalysis are notable drawbacks of these agents. Even the quantity of bacteria per milliliter of urine may be substantially reduced, altering results of quantitative urine culture. Diuretics to enhance urine collection by augmenting urine flow are thus best suited for serial urine sample collection when interpretation of urine specific gravity and semiquantitative evaluation of routine test components are not important.
Site Considerations
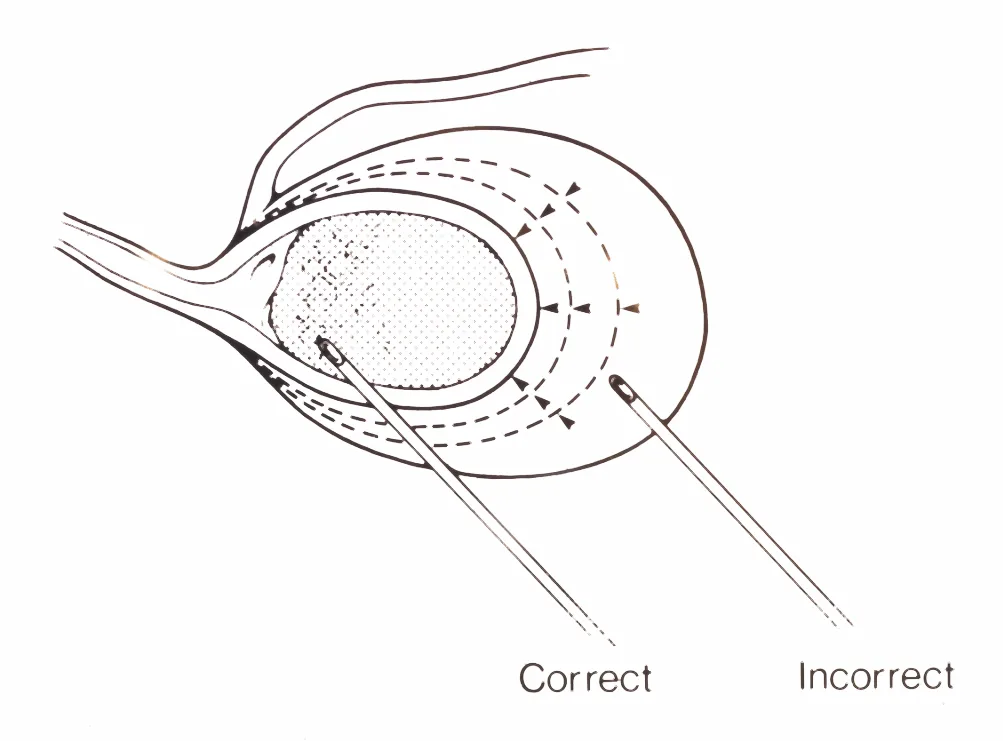
Careful planning minimizes risk. We recommend insertion of the needle into the ventral or ventrolateral wall of the urinary bladder to minimize the chance of trauma to the ureters and major abdominal blood vessels (Figure A). Direct the needle caudally, penetrating the bladder wall at an oblique angle (about 45 degrees), with the tip of the needle terminating at a safe distance from the bladder's attachment to the urethra rather than the vertex. This permits removal of urine without the need to reinsert the needle if the bladder contracts substantially.
One study reported that clipping the hair and disinfecting the skin had no effect on results of samples submitted for urinalysis and bacterial culture compared with samples collected without these procedures.2 However, this study was not designed to assess the effects of lack of disinfection on the patient. To facilitate palpation and visualization of the bladder, minimize iatrogenic infection to the patient, and accurately insert the needle through abdominal skin (and not your hand), clip excessive fur (the ventral midline is relatively hairless; therefore clipping may not be necessary) and swab the fur and skin with alcohol.
Diagnostic Cystocentesis
Advantages
Quick and easy
Less risk for iatrogenic urinary tract infection than with transurethral catheterization
Prevents contamination of urine samples, which frequently occurs during voiding through urethra and genital tract
Aids in localization of hematuria, pyuria, and bacteriuria
Disadvantages
Dependent on adequate urine to allow palpation/immobilization of urinary bladder
Frequently associated with needle-induced microscopic hematuria
May be associated with implantation of neoplastic bladder cells along pathway of needle1
Chance of contaminating urine sample with abdominal/intestinal contents is greatest during blind cystocentesis
Step-by-Step: Performing Diagnostic Cystocentesis
What You Will Need
22-gauge needles; 1.5-inch hypodermic or 3-inch spinal needle may be selected depending on size of patient and distance of ventral bladder wall from ventral abdominal wall
3- to 12-ml syringes; most normal reference values for urine sediment are based on centrifugation of 5 ml urine, so we generally use 6-ml syringes
Cotton balls saturated with 70% alcohol or 70% alcohol in a spray bottle
Step 1
To minimize trauma from needle movement, hold the syringe (with attached needle) with your thumb and first two fingers. This grasp allows you to insert the needle into the bladder and aspirate urine into the syringe (by withdrawing the plunger of the syringe with your second finger) without repositioning the syringe in your hand.

Step 2
The patient may be placed in dorsal, right lateral, or left lateral recumbency or in a standing position. If you are right-handed, hold the syringe in your right hand and have the patient's head to your right side (or vice versa if you are left-handed). This facilitates needle advancement in a caudal direction and allows the needle tip to remain in the bladder lumen (i.e., as urine is removed, the vertex of the bladder contracts caudally toward its junction with the urethra) (Figure A).
Step 3
Success is dependent on palpation and immobilization of the urinary bladder. Palpate slowly to allow the patient to become accustomed to your touch. If you are right-handed, localize and stabilize the bladder with your left hand (or vice versa if you are left-handed). Because the bladder is secured caudally by its attachment to the urethra, grasping the caudal aspect of the bladder and applying traction in a cranial direction helps stabilize it during the procedure. When cystocentesis is performed in a patient positioned in lateral recumbency, support the back to minimize movement during palpation. In this position, the needle can be directed dorsocaudally or laterocaudally. Be careful not to apply excessive digital pressure to the bladder wall.
Procedure Pearl
Success is dependent on palpation and immobilization of the urinary bladder.

Step 4
Insert the needle through the ventral abdominal wall, advancing it toward the caudoventral aspect of the bladder. When performing cystocentesis in a dog in a standing position, lift the skin and hair of the flank dorsally to facilitate visualization of the site of needle insertion (Figure 4A). If the dog is in dorsal recumbency, insert the needle in front of or lateral to the prepuce, depending on the size and position of the urinary bladder (Figure 4B).


Needle-Entry Location
Precise location of entry of the needle into the bladder wall is not critical. The needle should be inserted at an oblique angle (about 45 degrees). With this approach, elasticity of bladder musculature and the interlacing arrangement of individual muscle fibers provide a better seal of the pathway created by the needle when it is removed. In addition, subsequent distension of the bladder wall as the lumen refills with urine tends to force the walls of the needle tract into apposition.
Step 5
If urine cannot be aspirated, withdraw the needle and discard it along with the syringe because it may contain blood that will contaminate the sample. In addition, a new needle and syringe minimize iatrogenic microbial infection from the intestine and skin. If several attempts are unsuccessful, wait until sufficient urine has accumulated in the bladder.
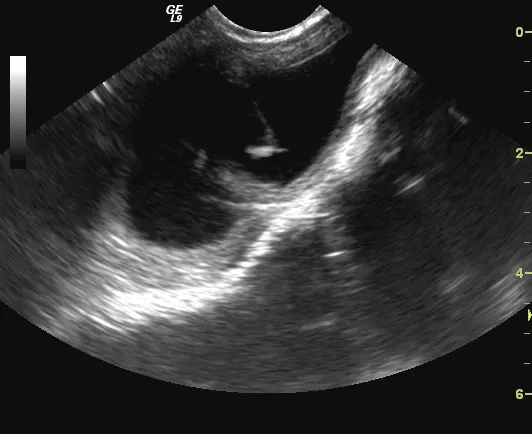
Ultrasound-guided cystocentesis could also be used to safely obtain a urine sample. This method can be done freehand or with a biopsy guide and is done without biopsy gel-sterile saline or alcohol is applied over the biopsy site. Insert the needle close to the transducer, keeping the needle within the plane of the ultrasound beam. After verification that the tip of the needle has advanced to the desired position in the bladder lumen, aspirate urine into the syringe (Figures 5A and 5B).
Procedure Pearl
Routine cystocentesis should not be done unless sufficient urine in is the lumen to permit localization and immobilization of the bladder by abdominal palpation.

Step 6
To prevent urine from being forced around the needle into the peritoneal cavity, avoid applying excessive digital pressure to the bladder while the needle is in the bladder lumen or immediately after the procedure. In most instances, prophylactic antibacterial therapy is not necessary but should be based on patient status and retrospective evaluation of the technique.
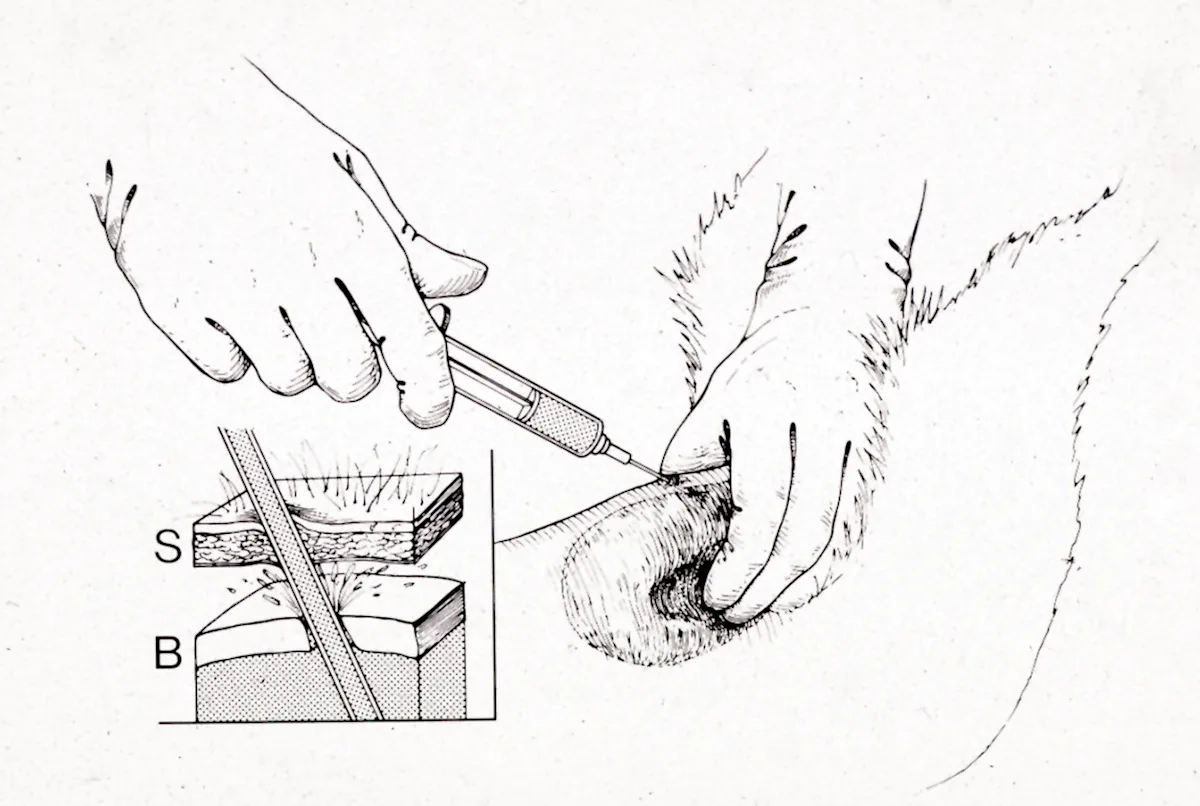
S = skin of abdominal wall;
B = wall of urinary bladder
Step 7
On rare occasions, cystocentesis has been associated with a form of reversible collapse in cats. Although a cause-and-effect relationship has not been established, excessive vagal stimulation has been implicated. Acute bladder distension has been associated with bradycardia in humans.3 In one study, decreased heart rate induced by bladder distension only occurred in human patients with concomitant hypertension.4 Thus, excessive manipulation and compression of the urinary bladder should be avoided.
Step 8
To avoid aspiration of fat or abdominal contents, stop retracting the plunger before withdrawing the needle.
Step 9
Although blind cystocentesis (i.e., without palpating and immobilizing the bladder) has been described,5 we do not recommend it as a routine technique because of the increased risk to the patient and the potential to contaminate the sample.
Procedure Pearl
To prevent urine from being forced around the needle into the peritoneal cavity, avoid applying excessive digital pressure to the bladder while the needle is in the bladder lumen.