Constant-Rate Infusions: Practical Use
Douglass K. Macintire, DVM, MS, Diplomate ACVIM & ACVECC, Auburn University
Mary Tefend, Hill’s Clinical Instructor of Critical Care Nursing, Auburn University
Overview
In recent years, delivery of drugs with CRI has become fairly routine in critical care referral practices and in veterinary teaching hospitals. Despite advances in technology allowing for more accurate administration of fluids through intravenous fluid pumps, many veterinarians continue to avoid use of CRI.
Several cardiac and vasoactive drugs have potent hemodynamic effects that can markedly affect the outcome of critically ill veterinary patients. Drugs that have a rapid onset of action and a short half-life are ideal for CRI delivery because the veterinarian can provide a continuous, steady-state concentration of the drug and titrate it to the desired effect. The CRI method is also an excellent way to deliver analgesic agents because it eliminates the peak and trough effects that occur with intermittent dosing.
Why It's Avoided
There seem to be three reasons why many veterinarians avoid CRI. First, the mathematics used to calculate dosages can be intimidating, especially when miscalculations can be fatal. Second, because many of the drugs administered via CRI are relatively new, veterinarians may have little experience in their use. Finally, proper administration of CRI drugs ideally involves the use of specialized equipment, such as infusion pumps and blood pressure monitors. Although lacking in many practices, these items are readily available and have become more affordable for the average veterinarian.
The purpose of this article is to provide some user-friendly formulas and to simplify the calculations needed to administer drugs via CRI. (Numbers in answers are rounded as appropriate.) While it should provide the groundwork needed to start administering drugs with CRI, acquiring the necessary equipment and gaining the confidence and experience needed to use these drugs is the responsibility of the veterinarian.
CRI = constant-rate infusion
How to Calculate Dosages*
Formula 1
By convention, the dosage for many CRI drugs is given as µg/kg/min. The calculations can be confusing since most drugs are available in concentrations of mg/ml and are delivered at a fluid rate of ml/hr. The following formula allows the clinician to "plug in" the numbers and solve for the number of milligrams of drug to add to the base solution.
* Answers have been rounded as appropriate.
M = (D) (W) (V) / (R) (16.67) OR R = (D) (W) (V) / (M) (16.67)
M = number of mg of drug to add to base solution D = dosage of drug in μg/kg/min W = body weight in kg V = volume in ml of base solution R = rate of delivery in ml/hr 16.67 = conversion factor
Case Example 1: A 6-year-old, 28-kg, male Doberman pinscher presents with severe, left-sided heart failure and pulmonary edema due to dilated cardiomyopathy. After treatment with furosemide (2 mg/kg IV) and oxygen, the pulse remains weak and perfusion is poor. Dobutamine, at a dosage of 15 µg/kg/min, is chosen to provide immediate positive inotropic effects. Because the dog has pulmonary edema, a low fluid rate of 10 ml/hr is chosen to administer the drug. The drug was to be added to 100 ml of 5% dextrose solution, because high-sodium fluids should be avoided in patients with congestive heart failure.
M = (15 µg) (28 kg) (100 ml) = 250 mg / (10) (16.67)
Dobutamine is available as a concentration of 12.5 mg/ml (see Table).
250 mg ÷ 12.5 mg/ml = 20 ml
Twenty ml of dobutamine are added to 80 ml 5% dextrose solution to make a total volume of 100 ml administered at 10 ml/hr.
Table: Drugs Commonly Administered by CRI
To illustrate how Formula 1 can be used to adjust the dosage based on clinical signs, consider the following problem:
The dog develops tachycardia when dobutamine is administered at a dosage of 15 µg/kg/min. The dosage can be decreased to 10 mg/kg/min, and we can solve for R to determine the rate adjustment necessary to deliver the drug at the reduced dosage.
R = (D) (W) (V) / (M) (16.67) = (10) (28) (100) / (250) (16.67) = 7
The fluid rate is decreased to 7 ml/hr.
Formula 2
A quick-and-easy formula that allows the clinician to convert directly from the drug dosage in µg/kg/min to mg requires that a standard volume of 250 ml be administered at a standard rate of 15 ml/hr.
Drug dosage (μg/kg/min) ⋅ BW (kg) = no. mg to add to 250 ml base solution at a rate of 15ml/hr
Case Example 2: A 30-kg dog in septic shock has a blood pressure of 60/40 mm Hg that has not improved with fluid resuscitation. You decide to try to increase the pressure with a pressor dose of dopamine at 10 µg/kg/min.
(10 µg) (30 kg) = 300 mg dopamine added to 250 ml at 15 ml/hr
Dopamine is available as a 40 mg/ml solution, so 7.5 ml (300/40) is added to 250 ml base solution. This formula could be manipulated further by multiplying by 2 to determine how many mg to add to 500 ml or by 0.4 to determine how much to add to 100 ml.
Formula 3
Some drugs, including many analgesic agents, are given in a dosage of mg/kg/hr. For these drugs, the easiest way to calculate the daily dose is to administer in a 250-ml fluid bag at 10 ml/hr. At this rate, the CRI will last for 25 hours. Note that most analgesic agents require a loading dose before CRI is begun.
Dose (mg/kg/hr) × BW(kg) × 25 hr / Drug (mg/ml) = no. of ml drug to add to 250 ml base at 10 ml/hr
Case Example 3: A 20-kg dog is placed on a morphine drip for postoperative analgesia. Following a loading dose of 0.2 mg/kg IM, the dog is placed on CRI at a dosage of 0.2 mg/kg/hr.
(0.2 mg) (20 kg) (25 hr) / 15 mg/ml = 6.7 ml added to 250 ml base at 10 ml/hr (will provide continuous pain control for 25 hours)

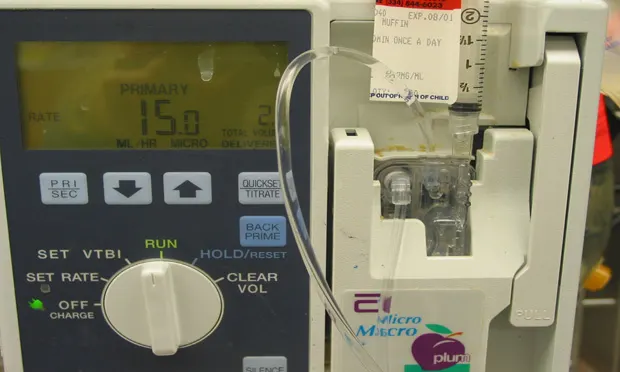
FIGURE 1
The Medfusion 2010 Syringe pump ($2200; Medex, Inc., Carlsbad, CA) can accurately deliver drugs in syringes ranging in size from 3 to 60 ml.