Clinical Notes: How Cytopoint Paved the Way for Monoclonal Antibody Therapy in Veterinary Medicine
Candace A. Sousa, DVM, DABVP (Emeritus, Canine & Feline), DACVD (Emeritus)
Sponsored by Zoetis
KEY POINTS
Monoclonal antibody (mAb) therapy mimics the body’s natural immune defense processes and works by binding to and neutralizing extracellular targets such as circulating molecules or cellular receptors. mAbs are highly targeted therapeutics and can have distinct advantages over traditional small molecule pharmaceuticals, but understanding the pathophysiology of the disease being treated is key to identifying an effective antibody target.
The cytokine IL-31 has been shown to induce pruritus when injected into dogs, and identifying IL-31 as a therapeutic target has led to the development of more targeted medications for the treatment of canine AD, particularly mAbs.
Cytopoint® (lokivetmab), a caninized mAb therapy, has been shown to be effective in the treatment of dogs against allergic and atopic dermatitis.
Other mAbs that would block canine IL-31 in a different way could potentially be developed for use in animals; however, clinical trials, documented safety, and pharmacovigilance reporting would be needed before a valid, positive comparison of clinical safety or efficacy could be made to Cytopoint.
Monoclonal antibody (mAb) therapy has been available for almost 4 decades to treat a wide range of diseases in human health1 but is a relatively new therapeutic option in veterinary medicine. Cytopoint® (lokivetmab) is a caninized mAb therapy and the first mAb product that has been shown to be effective in the treatment of dogs against allergic and atopic dermatitis. Since the approval of Cytopoint, additional mAb products have been approved in various countries for the treatment of other chronic conditions. Examples include frunevetmab (Solensia®) for the control of osteoarthritis (OA) pain in cats and bedinvetmab (Librela®) for alleviation of OA pain in dogs.
This article outlines the clinical use of mAb therapies for dogs with allergic and atopic dermatitis, developments that may lay ahead, and what clinicians should consider as this area of veterinary medicine continues to expand.
An Introduction to Monoclonal Antibody Therapy
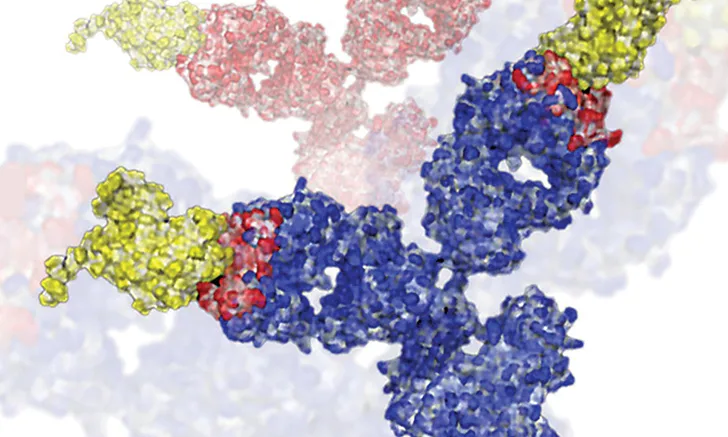
In the 20th century, scientists realized the specific and highly targeted nature of the body’s normal immune response to disease could be applied to the development of a new therapeutic approach.1 Antibodies directed at specific body (or self) proteins involved in a given disease process could be produced outside of the patient, then injected to disrupt a disease process by neutralizing a protein that plays a core role in the pathogenesis of a disease (Figure 1). In 1973, Jerrold Schwaber described the production of mAbs using human–mouse hybrid cells,2 and in 1975, Georges Köhler and César Milstein succeeded in making fusions of myeloma cell lines with B cells to create hybridomas, which could produce antibodies specific to known antigens and that were then immortalized.3

Antibodies bind to a circulating protein to neutralize it.
Treatment with mAbs mimics the body’s natural immune defense processes, wherein antibodies may be generated to neutralize a target such as bacteria or a virus. Traditional small molecule therapeutics (eg, antibiotics, Janus kinase inhibitors, corticosteroids) target sites inside the cell, whereas mAb therapy works by binding to and neutralizing extracellular targets such as circulating molecules or cellular receptors.
mAbs can have distinct advantages over traditional small molecule pharmaceuticals.4 The antibody–target complexes are broken down in the body slowly over time like other proteins via catabolic processes and lysosomal degradation.4 The half-life and correlated duration of the therapeutic effect of an mAb can be long-lasting, as therapeutic mAbs utilize the neonatal Fc receptor antibody recycling mechanism. Unlike traditional drug therapy, catabolism does not rely on the patient’s kidney or liver drug metabolism function, making antibody therapy a treatment consideration for dogs regardless of age, major organ drug-metabolizing capacity, or potential for interference with metabolism of other medications being administered concurrently.4 In addition, residual unbound mAbs in circulation do not cause adverse effects because they are a small part of the pool of antibodies already present in blood for circulating immunity. Once targets are saturated with mAbs, the remaining unbound mAbs do not have an effect anywhere else in the body.4
Developing Monoclonal Antibody Therapies
Unlike many small molecule therapies, mAb therapies are highly targeted therapeutics.4 Understanding the pathophysiology of the disease being treated is key to identifying an effective antibody target. Furthermore, understanding what role the targeted cytokine (or other protein) has in the body is critical to determining the safety of the therapy. If a targeted cytokine has multiple physiologic functions in the body, unwanted effects could occur, resulting in safety concerns or unwanted adverse effects.4
Research on the pathophysiology of canine atopic dermatitis (AD) has identified the major immunologic mediators driving pruritus and inflammation: cytokines, small protein molecules secreted by cells that have a specific effect on the interactions and communications among cells.5 Cytokines fuel an interconnected multidirectional network of biochemical interactions that create the clinical syndrome known as AD, including the disruption of the barrier function, pruritus, inflammation, and the resultant clinical lesions.
Regardless of the underlying and inciting causes, cytokines are one of the common denominators in allergic and atopic skin conditions.
In allergic skin disease, cytokines are primarily released by cells such as T-helper 2 (Th2) lymphocytes, but many cell types that interact with allergens (eg, keratinocytes, dendritic cells, macrophages) can also respond by releasing cytokines.5 They provide communication among the skin, nervous system, and immune system and are the primary cause of the neuronal itch, which is the hallmark of allergic skin disease.5
Regardless of the underlying and inciting causes, cytokines are one of the common denominators in allergic and atopic skin conditions. In dogs with allergic skin disease, multiple cytokine mediators, including interleukin (IL)-2, IL-4, IL-5, IL-6, IL-13, and IL-31, are implicated. Each of these cytokines plays a specific role in the production of clinical signs such as pruritus and skin inflammation (Figure 2).5

Multiple cytokines are released from lymphocytes to coordinate the clinical signs seen in dogs with atopic dermatitis.
Interleukin-31
The cytokine IL-31 has been shown to induce pruritus when injected into dogs.6 It has also been found to be significantly increased in the serum of dogs with naturally occurring AD (Table).6-8
IL-31 receptors are found on sensory neurons in the skin, and IL-31 mediates pruritus directly by binding to and activating these neurons. IL-31 also binds directly to IL-31 receptors on other cell types to cause the release of proinflammatory mediators from cells such as keratinocytes and immune cells triggering skin inflammation.
TABLE: SERUM LEVELS OF IL-31 IN VARIOUS CANINE POPULATIONS
Identifying IL-31 as a therapeutic target has led to the development of more targeted medications for the treatment of canine AD, particularly mAbs. It became understood that an mAb that inhibits the function of IL-31 could hold the potential to uniquely and specifically improve the signs of allergic dermatitis without the adverse effects associated with broad spectrum pharmacotherapy; this understanding led to the development of Cytopoint.
Pruritus: A Major Pet Owner Concern
Pruritus is the most common reason dog owners present their pet to a veterinarian beyond wellness care.9 There are many conditions that can cause a dog to be pruritic, including parasites, infections, and, commonly, allergic skin disease. Despite how common it is, treatment options for canine AD and its associated pruritus are not always ideal; for example, the International Committee on Allergic Diseases of Animals considers antihistamines to be of little to no benefit in the treatment of acute flares of AD.10 In addition, studies have suggested that 10% to 81% of patients receiving glucocorticoids or cyclosporine may experience adverse effects.11,12
In a survey, when owners were asked about the quality of life of their dogs with allergic and atopic skin disease, ≈90% believed that they understood the disease, and >96% accepted that their dog would require lifelong care.13 Also in this survey, which was conducted prior to FDA approval of Apoquel® (oclacitinib), ≥88% of surveyed dog owners were dissatisfied with the treatment options that were previously available to them, as it was either a major burden or they were unsure about the best therapeutic option.13 In another survey, 36% were also dissatisfied with the treatment options available.14 Thus, a need to develop alternate treatment options for this long-term chronic disease was identified.
The Efficacy of Cytopoint Against Allergic Dermatitis in Dogs
Scientists at Zoetis worked to produce a caninized mAb therapy that would bind to and neutralize soluble IL-31 and could be used as a treatment for AD. This mAb therapy is lokivetmab (Cytopoint). The importance and clinical relevance of targeting IL-31 has been established through the significant improvements reported in allergic pruritus and dermatitis severity in dogs associated with atopic and allergic skin disease following administration of Cytopoint in numerous clinical studies.15-23
Cytopoint has a mean serum half-life of 16 days and therefore remains in circulation for several weeks.15 In the United States, it is labeled to be administered subcutaneously at a minimum dose of 2 mg/kg every 4 to 8 weeks or as needed.24 In Europe, it is labeled to be administered monthly or as needed after a dose of 1 mg/kg.25
In a 2016 clinical trial, Cytopoint was shown to significantly decrease allergic pruritus after 1 day when administered to dogs with AD at 2 mg/kg, with maximal improvement seen by day 7 (Figure 3).15

Cytopoint significantly decreases pruritus after 1 day when administered at 2 mg/kg to dogs with AD, with maximal improvement seen by day 7.
A significantly greater proportion of dogs receiving Cytopoint at 2 mg/kg achieved treatment success from days 1 to 56 based on owner assessment of pruritus (visual analog scale [VAS]) as compared with placebo.15 Treatment success was defined as at least a 2-cm (20-mm) pruritus score reduction from baseline. This same study showed Cytopoint was effective in reducing initial client VAS scores by at least 50% in 57% of patients at 28 days.15 The clinical trial also demonstrated that the skin condition of these dogs significantly improved within the first week as compared with placebo-treated dogs, as measured by veterinary dermatologists using the Canine Atopic Dermatitis Extent and Severity Index (CADESI-03; Figure 4).15

The skin condition of atopic dogs treated with 2 mg/kg of Cytopoint significantly improved within the first week as compared with placebo-treated dogs, as measured by veterinary dermatologists using the Canine Atopic Dermatitis Extent and Severity Index (CADESI-03).
In a retrospective study, 87.8% of dogs with a variety of confirmed allergic dermatoses (eg, AD, adverse food reaction, allergic disease of undetermined cause) treated with Cytopoint were regarded as “successful” using the previously described definition of success.17 Thus, in that study, Cytopoint had demonstrated efficacy not only for dogs with AD but also for dogs with other skin allergies, even when the specific underlying cause of allergic dermatitis was uncertain.18
The Safety of Cytopoint
Cytopoint is safe and effective for dogs of all ages and sizes, those receiving a variety of concomitant medications, and those with comorbidities.15-18,26 Adverse effects reported in the original studies (cited on the US package insert) for dogs that were administered Cytopoint and for the placebeo control group were found to have similar frequency to one another. These adverse effects consisted primarily of minor pain at the injection site.15
During a continuation therapy study, the European Medicines Agency Committee for Medicinal Products for Veterinary Use concluded that there is sufficient safety data to alleviate concerns that chronic use could lead to immunosuppression, an increased need for antibacterial medications, or treatment-induced immunogenicity.27
In another study, the safety of Cytopoint was evaluated, showing it to be well tolerated when administered to laboratory beagles at up to 10 mg/kg for 7 consecutive monthly doses.28 Enhanced pathology evaluations of immune tissue revealed no changes in any lymphoid tissue that would be suggestive of a treatment effect. In addition, no safety concerns regarding immunogenicity of the molecule have been identified. The only treatment-related change in the laboratory- based study was a mild tissue reaction at the injection site and the draining lymph nodes seen on histopathology.28
Cytopoint has changed the quality of life of many of these animals and their owners.
Cytopoint is approved for use in most major companion animal markets, including the United States, the European Union, Australia, and countries in Asia. Since Cytopoint became available to veterinarians in 2016, more than 5.5 million dogs in the United States have been treated.29 The reported adverse effects are generally consistent with those observed in clinical trials.15,16 The most commonly reported adverse events not related to the skin in clinical trials to support global registrations were mild GI signs (vomiting and diarrhea) and lethargy.16,26 Adverse events appear to occur in rates similar to placebo groups.24
Cytopoint has changed the quality of life of many of these animals and their owners.30 When US dog owners were surveyed in 2021, 90% reported that they were either “satisfied” or “very satisfied” with Cytopoint therapy.31 In a global survey, 60% of veterinarians surveyed were “satisfied” or “very satisfied” with Cytopoint therapy.32
The Future of Monoclonal Antibody Therapy
Veterinary researchers are now investigating the role of canine IL-31 in pruritus caused by diseases other than allergies. Some initial studies have found that Cytopoint, while binding only to circulating IL-31, has demonstrated an effect on the clinical signs for several different conditions.33,34 Researchers are also looking at other targets for the development of monoclonal antibodies to treat pruritus and allergic dermatitis in a variety of species.5
Other mAbs that would block canine IL-31 in a different way—either by binding to the IL-31 receptor or to an epitope on the cytokine different than lokivetmab—could potentially be developed for use in animals. Large-scale clinical trials, short- and long-term safety documented in laboratory and clinical trials, and postmarketing pharmacovigilance reporting would be needed before a valid, positive comparison of clinical safety or efficacy could be made to Cytopoint. Even a product with the same cytokine target as Cytopoint could have seemingly minor differences that impact efficacy and therefore the clinical condition. Efficacy of an individual product should not be presumed without supportive data.
Other mAbs that would block canine IL-31 in a different way—either by binding to the IL-31 receptor or to an epitope on the cytokine different than lokivetmab—could potentially be developed for use in animals.
Because veterinary medicine has led the way in targeting IL-31 for the treatment of allergic skin disease in dogs, human medicine researchers are now looking at a similar therapeutic with either a humanized anti–IL-31 mAb therapy or an mAb that targets and blocks the IL-31 receptor. There are ongoing studies evaluating mAbs that target IL-4 and IL-13 receptors to treat AD in humans.35 There are also clinical trials using humanized mAbs that target circulating IL-5, -13, -17, -12/23, -22, and -33 and thymic stromal lymphopoietin.35
In human medicine, biosimilar mAbs are now being approved. Biosimilars are not completely identical to the original product for many reasons; biosimilars are developed to have an analogous area of action as the reference molecule but, for example, may bind to a different epitope or may have different impurity profiles (because the processes used to manufacture the reference molecule are proprietary to the company that registered the original reference molecule).36 A certain amount of molecular variability is unavoidable. Biosimilar mAbs are not the same as generic small molecules, which can be precisely replicated and deemed bioequivalent to the original product. Clinicians should have a clear understanding of how these products can be used and prescribed. From a clinical point of view, some differences have to be carefully considered. Differences in efficacy, immunogenicity, and adverse events are possible and may be pronounced with long-term use. The approval of biosimilars is only partially based on the results of clinical trials.37 To date, there are no biosimilars for the few mAbs available in veterinary medicine.
Although Cytopoint has been shown to be an effective treatment for many dogs with AD and allergic dermatitis, not all dogs respond to it; other cytokines or cytokine receptors may be potential targets. In addition to in vitro studies, clinical trials would be needed to prove the relevance and impact on the clinical condition, as well as the safety of blocking the specific target. As has occurred in human medicine, products that combine more than one mAb may be developed for the treatment of allergic skin disease.

Conclusion
For treatment of a lifelong disease such as canine AD, the development and use of a biologic such as Cytopoint has changed the lives of millions of allergic dogs, their owners, and the veterinarians who treat them. As this area of veterinary medicine continues to evolve, with mAbs developed for the management of other canine and feline diseases, clinicians should stay informed and understand the relevance of the molecular target to the disease they are treating and the potential effects of blocking the target with a biologic therapy. Clinicians should also continue to critically assess the evidence available to support the efficacy and safety for each product used in their practice.
