Canine Keratoconjunctivitis Sicca
Alison Clode, DVM, DACVO, Port City Veterinary Referral Hospital, Portsmouth, New Hampshire
PROFILE
Keratoconjunctivitis sicca (KCS) results from a deficiency of the precorneal tear film in which either an inadequate quantity or deficient quality of tears are produced.
The precorneal tear film is composed of 3 layers:
Inner mucin layer: adheres the tear film to the cornea
Middle aqueous layer: provides corneal nutrition and waste removal
Outer lipid layer: prevents evaporation of the tear film
Quantitative deficiency involves the aqueous layer, which is produced by the orbital and nictitating membrane (NM) lacrimal glands.
Qualitative deficiency involves the mucin layer, which is produced by conjunctival goblet cells, or the lipid layer, which is produced by meibomian glands.
Related Article: Corneal Cytology & Culture Collection
Causes of Quantitative Deficiency
Most commonly, immune-mediated (T-cell) inflammation of the orbital and NM lacrimal glands occurs as an isolated immune-mediated condition without manifestations in other body systems.<sup1 sup>
Other causes include:
Trauma to the eye or orbit
Congenital lacrimal gland hypoplasia or aplasia
Neurogenic deficiency (loss of sensory innervation from cranial nerve V or loss of parasympathetic innervation via cranial nerve VII)
Drug-induced
Temporary caused by atropine, sedation, local anesthesia, or general anesthesia
Permanent or temporary because of systemic sulfonamide or etodolac administration
Lack of correction or surgical removal of prolapsed NM gland
Local irradiation
Endocrine diseases (eg, diabetes mellitus, hypothyroidism, hyperadrenocorticism)
Canine distemper virus infection
Chronic blepharoconjunctivitis
Related Article: The Concept of Corneal Protection
Causes of Qualitative Deficiency
Chronic blepharitis, blepharoconjunctivitis, or meibomianitis
Immune-mediated diseases targeting mucocutaneous junctions (eg, bullous pemphigoid, systemic lupus erythematosus)
Deficient quantity of tears leads to hypertonicity of tears with subsequent dehydration and hypoxia of the ocular surface.
Signalment
Predisposed breeds for presumptive immune-mediated KCS include1:
Cavalier King Charles spaniel, English bulldog, Lhasa apso, shih tzu, West Highland white terrier, American cocker spaniel, Pekingese, Boston terrier, miniature schnauzer, Samoyed
Predisposed breeds for lacrimal gland hypoplasia/aplasia1,2:
Chinese crested, Yorkshire terrier, Bedlington terrier, pug
Pathophysiology
Deficient quantity of tears leads to hypertonicity of tears with subsequent dehydration and hypoxia of the ocular surface.1
Deficient tear quality leads to destabilization of the tear film with subsequent evaporative loss.
Deficient tear quality also hinders the smooth movement of eyelids over the ocular surface; this creates irritation and decreases clearance of metabolites.1
Inflammation of the conjunctiva and cornea can predispose a patient to secondary bacterial conjunctivitis in association with breakdown of protective barriers.
Ocular surface pigmentation, vascularization, and fibrosis result from chronic irritation associated with insufficient protection of the ocular surface.
Clinical Signs
Conjunctival hyperemia and mucoid-to-mucopurulent (in the presence of secondary bacterial infection) ocular discharge are present in early stages.
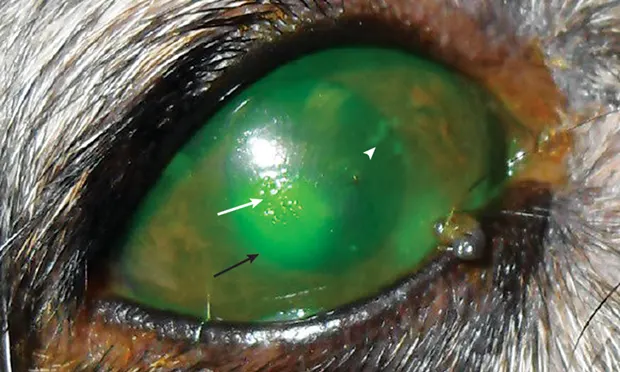
Lackluster ocular surface caused by patchy and incongruous precorneal tear film in early stages (Figure 1) can be seen.
Corneal vascularization, fibrosis, and pigmentation are noted in later stages (Figure 2).
Corneal ulceration may be present (Figure 1).
Immune-mediated, drug-induced, canine distemper virus-associated, and endocrine- associated conditions generally cause bilateral disease.
Congenital, neurogenic, irradiation-induced, and surgically induced conditions may be unilateral or bilateral.
DIAGNOSIS
Diagnosis of quantitative tear film deficiency is made via Schirmer tear test (STT), which measures basal and reflex production of the aqueous component1:
Normal: 15 mm wetting/minute
Early KCS: 11-14 mm wetting/minute
Moderate KCS: 6-10 mm wetting/minute
Severe KCS: <5 mm wetting/minute
The presence of coinciding clinical signs, particularly in the early stages, is important in the diagnosis of KCS.
Diagnosis of qualitative tear deficiency is more difficult, as the STT is normal but clinical signs consistent with KCS are present.
Visual observation should be performed for lackluster, incomplete tear film.
Severe generalized eyelid margin inflammation may be present.
A tear film break-up time test (see Tear Film Break-Up Time Test) may confirm a mucin deficiency that leads to poor adherence of the tear film to the ocular surface.
Rose bengal staining can identify mucin and albumin deficiencies on the ocular surface.
Related Article: Multiple Punctate/Grid Keratotomy for Indolent Corneal Ulcers
TREATMENT
Medical
Treatment of quantitative and qualitative tear film deficiencies requires the use of lacrimostimulants, with the specific type determined by the underlying cause.
As most cases of KCS in dogs are presumed to be immune-mediated, calcineurin inhibitors are most effective for decreasing the T cell infiltration of the lacrimal glands that inhibits lacrimal secretions.1
Cyclosporine is commercially available as 0.2% ointment and is also available compounded to solutions with concentrations as high as 2%.3,4
Tacrolimus is available as compounded preparations (0.02% to 0.03%).5
Administration is generally 1 drop of solution (or 1/4 inch strip of ointment), 2 to 3 times daily for the remainder of the patient's life, for both cyclosporine and tacrolimus.
Neurogenic causes of KCS require cholinergic agonists to provide direct parasympathetic stimulation to the lacrimal glands, which is effective when functional glandular tissue remains.
Pilocarpine ophthalmic solution (1% to 2%) can be administered orally.
Administration starts at 1 drop/10 kg body weight twice daily and gradually increases by 1 drop/day every 5 to 7 days until improvement is noted.
The oral route of administration predisposes to systemic effects of parasympathetic stimulation (eg, vomiting, excessive salivation, urination, defecation), which necessitates decreasing the daily dosage to the highest level that does not cause adverse effects.
As an alternative, topical dilute pilocarpine (0.125%) can be administered.
However, this may cause significant ocular irritation and is less likely to result in increased tear production.
Some cases of neurogenic KCS may be self-limiting, allowing discontinuation of therapy.6
All cases of tear film deficiency benefit from lacrimomimetic agents (tear supplements or artificial tears) that mimic tear film.
Formulations contain molecules with physicochemical properties that improve adherence to and coverage of the cornea by the tear film.
Improve eyelid movement
Improve clearance of metabolites
Improve patient comfort
Common ingredients include hyaluronate, methylcellulose, hydroxypropyl methylcellulose, and polyvinyl alcohol
Many commercial, over-the-counter options are available.
In some cases, tear film deficiency may lead to ocular surface inflammation that is significant enough to necessitate short-term administration of topical corticosteroids in combination with an antibiotic (to address potential coinciding secondary bacterial infection).
Dexamethasone with neomycin and polymyxin B 2 to 3 times daily for 2 to 3 weeks is generally sufficient.
Surgery
Surgical transposition of the parotid salivary duct to the conjunctival fornix can improve signs by redirecting salivary secretions to the ocular surface.
Referral to a veterinary ophthalmologist is advised.
Short- and long-term complication rate is 50%, including (but not limited to) intolerance to saliva, ocular surface mineral deposition, progression of corneal pigmentation, recurrent and recalcitrant ulcerations, and excessive salivation and facial wetting.7
Client Education
Treatment is lifelong.
Recurrence or development of new signs warrants repeat evaluation.
May indicate reduced responsiveness to current treatment regimen
May indicate development of new (and potentially unrelated) ophthalmic condition
Recurrence of previous clinical signs or development of new clinical signs warrants repeat evaluation.
FOLLOW-UP
Evaluation of STT and clinical signs should occur within 1 month of initiation of treatment with lacrimostimulants.
Some cases will not respond completely within 1 month; treatment for an additional 2 to 4 weeks before diagnosing a treatment failure may be appropriate.
If no improvement occurs, or if improvement is followed by deterioration over time, increase the concentration of cyclosporine or substitute tacrolimus, and increase frequency of lacrimomimetic therapy.
Tear film deficiencies require regular (every 6 to 12 months) monitoring to ensure continued appropriate response to therapy.
Uncontrolled KCS results in progressive clinical signs and vision compromise.
IN GENERAL
Relative Cost
$ per month, lifelong
Topical lacrimogenic
Topical lacrimomimetic
Follow-up examination every 6 to 12 months once condition has stabilized
With judicious care and regular monitoring, prognosis for retaining vision and comfort is good, providing the condition is recognized early (ie, prior to onset of significant corneal pigmentation, vascularization, and fibrosis).
KCS = keratoconjunctivitis, NM = nictitating membrane, STT = Schirmer tear test