Burns
Paulo Gomes, DVM, DACVD, Purdue University
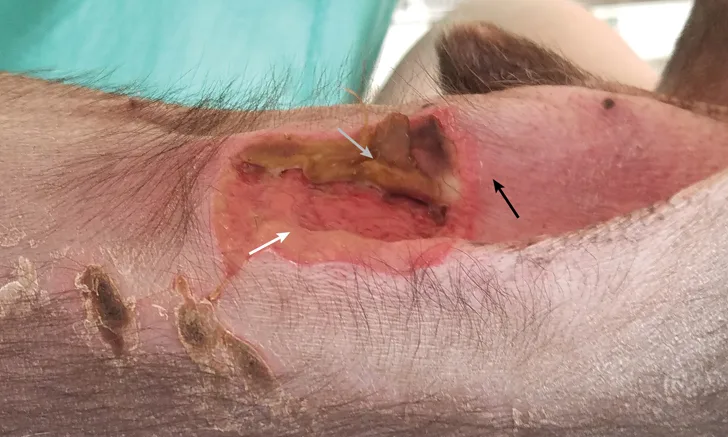
Heating pad burn in a Chihuahua. The 3 zones of injury (ie, coagulation [gray arrow], stasis [white arrow], hyperemia [black arrow]) are visible. Photo courtesy of Dr. Becky Zaremba
Burns are painful injuries with partial or complete skin damage caused by heat (ie, thermal burn), chemicals, radiation, and/or electricity.<sup1- 4sup> Thermal burns are the most common burns in dogs and cats5 and can be caused by fire, liquids, and heating pads and other heating devices (eg, dryers, mufflers, stoves), among others.2,6,7
Burn severity is classified according to the depth and size of injury (Table).3,8 Superficial burns affect only the outermost epidermis, whereas superficial partial-thickness burns encompass the epidermis and superficial dermis. Deep partial-thickness burns involve the full-thickness epidermis and extend to the deep dermis. Full-thickness and subdermal burns affect the epidermis, dermis, and subcutaneous tissue and can include fat, tendons, muscle, bone, and interstitium.8-10 Local burns involve <20% of total body surface area,3,8 whereas severe burn injuries—excluding outermost epidermal superficial burns (eg, sunburns)—affect >20% of total body surface area.11 Severe burn injuries can be superficial partial-thickness, deep partial-thickness, or full-thickness and subdermal.
In veterinary medicine, no method to estimate total body surface area has been described. Because of the various sizes and body conformations in veterinary patients, attempts to estimate the total body surface area involved in burn injuries using human methodology and body diagrams can lead to estimation discrepancies.3,11
Classification, Clinical Signs, & Healing Characteristics of Burns
Mild localized burns can result in local responses, and severe burn injuries can lead to life-threatening cardiovascular, respiratory, metabolic, and/or immunologic disorders.1-3,8-10,12 Localized responses consist of 3 zones of injury (ie, coagulation, stasis, hyperemia; Figure 1). The coagulation zone is the central area of maximum tissue damage and includes coagulation of proteins and irreversible tissue damage. The stasis zone is characterized by progressive thrombosis of surrounding vessels and decreased tissue perfusion. Tissue recovery in the stasis zone is variable. The outermost zone is the hyperemia zone and has increased perfusion and good tissue recovery.1,12
Systemic responses that release inflammatory mediators and cytokines occur with severe burns that affect ≥30% of total body surface area.13 Cardiovascular derangements from burn shock can occur due to reduced cardiac output, fluid loss, and increased vascular resistance.3 Furthermore, an increase in basal metabolic rate and a down-regulation of cell-mediated and humoral immune responses can be associated with severe burn injuries.12,14 Smoke inhalation, an associated comorbid condition in housefire or campfire victims, can be associated with bronchoconstriction, hypoventilation, pneumonia, and respiratory distress.14 Metabolic disorders do not occur with local burn injuries.3
History
When the burn is witnessed, history-taking should be straightforward. However, if the burn was not observed, skin damage may not be easily recognized by the pet owner, and presentation can be delayed, which is not uncommon. Skin lesions can occasionally be associated with a recent event or procedure (eg, contact with heating pads in anesthetic procedures, radiation therapy, heat lamps, hair dryers). In cases of malicious burns, responses during history-taking may be evasive and inconsistent, with a lack of explanation or nonplausible cause given for the burn.2,4-7,12
Clinical Signs
Superficial burns appear as erythematous, painful lesions with no blister formation or systemic involvement.11 The surface of these lesions is generally dry and flaky, blanches under pressure, and is prone to desquamation.3,11
Superficial partial-thickness burns are characterized as erythematous, moist lesions with moderate edema.8 Fluid-filled blisters tend to form shortly after injury and may break open. These wounds are often exceptionally painful due to loss of epidermal integrity and exposure of nerve endings.9
Deep partial-thickness and full-thickness burns develop a leather-like eschar of dead tissue that separates from viable skin (Figure 2).3,10,15 In deep partial-thickness burns, edema is intense and sensitivity to touch is reduced.9 Appearance is variable, with a mixed red to waxy white color. Blisters are often absent, and the wound surface is typically wet. Erythematous lesions still blanch but have a slow capillary refill time, and vascularity is compromised.3,9,11 Full-thickness burn wounds have a variable white, tan, or cherry red to black color and eschar formation. These wounds are dry and leathery in appearance, and hair epilates easily. Lesions do not blanch under pressure due to thrombotic blood vessels and poor distal circulation. Full-thickness burns may be painless or only have discomfort elicited with deep palpation and/or pressure due to complete destruction of nerve endings.9-11,16
Patients with substantial nonsuperficial burns can develop burn shock within 24 to 48 hours. Burn shock is a result of hypovolemia and the release of inflammatory mediators.3 Fluid loss can lead to hemodynamic instability that manifests clinically as hypotension, cardiac arrhythmias, and decreased capillary refill time.11

Same dog as in Figure 1. Localized deep partial-thickness wound 14 days after burn injury. The zone of maximum tissue damage characterized by leathery eschar formation can be noted. Photo courtesy of Dr. Becky Zaremba
Diagnosis
If the patient has a dense overlying haircoat, severity and extent of injury may be difficult to interpret until thick adherent crusts become evident or a necrotic odor is noticed. Toxic epidermal necrolysis is one of the main differential diagnoses; other common differential diagnoses include erythema multiforme, epidermal and subepidermal autoimmune blistering diseases (eg, pemphigus vulgaris, bullous pemphigoid), ischemic dermatopathies, and pressure necrosis.5 Burn wound biopsy can be helpful in determining the cause of injury and extent of microbial infection, establishing anatomic depth of the injury, and evaluating the adequacy of surgical excision17,18; it also has medical, legal, and forensic value.
Histologically, thermal and chemical burns are described as coagulation necrosis of the epidermis and deeper tissue. Electrical burns may display keratinocytes with stretched nuclei and fringed, elongated degenerated cytoplasm.2,5
Initial assessment of burn patients should include identification of superficial, partial, and full-thickness burn wounds and assessment of the total body surface area affected. If the patient is a victim of severe burn injury and/or smoke inhalation, emergency care should be performed according to the Advanced Trauma Life Support guidelines (airway, breathing, and circulation; see Suggested Reading) and requires identification of respiratory distress, cardiovascular derangements, and shock.11
The Table summarizes classification, clinical signs, and healing characteristics of burn wounds.
Treatment & Management
Patients with local and/or superficial burns can be managed as outpatients, whereas patients with severe burn injuries may require immediate intervention and hospitalization due to systemic imbalances.1,14 Burn wounds are initially clean but can be rapidly colonized by bacteria.1 Removal of debris, necrotic tissue, and loose skin is essential in any burn injury.2 Hydrotherapy can lessen the development of the coagulation zone and edema, can help with re-epithelialization and pain management,11 and is most helpful when performed within 2 hours of injury.2,8 Chilled (37.4°F-62.6°F [3°C-17°C]) water or saline should be applied to the wound for at least 15 to 30 minutes.2,8,11 Wounds can usually be clipped and cleaned with sterile saline and diluted chlorhexidine (0.05%), povidone/iodine (0.7%), or mild soap.8,11
Topical Therapy
Most local burns can be properly managed with daily cleaning and topical agents.1 In veterinary medicine, 1% silver sulfadiazine cream is widely used due to its broad-spectrum activity against bacteria, yeast, and fungi, as well as its good eschar penetration and minimal adverse effects. Additional options include triple antibiotic ointments containing neomycin/polymyxin B/bacitracin, mupirocin ointment, or mafenide acetate cream.2,8,11,14 Conversely, in humans, the use of silver sulfadiazine in the conservative treatment of burn wounds has been replaced by less painful, viscous, solid, and/or biologic dressings with superior healing properties, which are as efficacious as silver sulfadiazine in the prevention of wound infection.19,20 Newly developed technologies using tilapia skin have been successfully used to treat dogs, cats, and horses rescued from wildfires or with chemical burns.21,22 Initially developed to be used in humans as a biologic dressing, tilapia skin aids in the healing process by transferring collagen to the affected area; as a biologic dressing, it may also be associated with reduced pain during wound dressing changes.23,24
Fluid Therapy
Severe burn injuries require immediate critical care, including fluid and electrolyte therapy (eg, fluid resuscitation), intense analgesia, and wound management. Fluid resuscitation should be performed with isotonic crystalloids as indicated by the patient’s clinical condition. The use of colloids is controversial, but they may be useful in expanding plasma volume and compensating for the loss of plasmatic protein after initial fluid resuscitation.8,14
Pain Management
Opioids are considered the standard for addressing acute pain from severe burn injuries.25 Strong opioids (eg, morphine, fentanyl, oxymorphone, methadone) should be used intravenously during the acute phase of burn injury.8,25 Nonopioids (eg, NSAIDs, benzodiazepines, ketamine, gabapentin, lidocaine, anxiolytics) should be used alone or in combination with opioids for background and procedural pain. Background pain is generally of low-to-moderate intensity and long duration and occurs while the patient is at rest or developing regular daily activities. Procedural pain tends to be intense but brief in duration and occurs during wound debridement, dressing changes, and rehabilitation activities.26 During burn treatment, benzodiazepines combined with an opioid are regularly used to decrease background and procedural pain. Use of ketamine and propofol has also been adapted from human literature to reduce pain and anxiety during procedural pain in veterinary patients. Burn patients can also experience breakthrough pain, which is characterized by unexpected spikes of pain of short duration that occur despite analgesic treatment, and chronic pain due to nerve-ending damage that remains after burn wounds have healed.14,20,25,26
Surgical Management
For severe burn injuries, early debridement and eschar excision are important to prevent bacterial infection and sepsis and facilitate wound healing. Aggressive surgical debridement of dead skin at the level of the hypodermis favors the formation of healthy granulation tissue within a week after the procedure.8,15
Systemic Antimicrobial Therapy
Prophylactic systemic antibiotic therapy is discouraged, as it is not effective in the prevention of infection from burn wounds and may lead to the development of multidrug-resistant bacteria.2,27 With early escharectomy and aggressive surgical debridement, risk for complications such as burn wound infection significantly decreases. Due to microthrombosis and wound edema, systemic antimicrobials are less successful in the treatment of local infections, as they often do not reach the affected area in therapeutic concentrations.14,28 However, systemic antimicrobials are recommended in cases associated with systemic infection based on culture and susceptibility results.27
Nutritional Support
Nutritional support is necessary to address the increased protein and carbohydrate demand throughout the hypermetabolic phase.29 As long as renal and hepatic function are within normal limits, a high-protein and high-calorie diet should be recommended. Enteral nutrition is usually favored, as it helps maintain gut motility, provides first-pass nutrient delivery to the liver, reduces plasma endotoxin and inflammatory mediators, and decreases intestinal ischemia and reperfusion injury.8 In addition, early administration of antioxidants, particularly high doses of intravenous ascorbic acid (ie, vitamin C) with fluid therapy, can help decrease the formation of reactive oxygen species, improve hemodynamic parameters, and reduce volumes in fluid resuscitation procedures, as demonstrated in humans and animal models.30-32 In a sheep burn model, continuous high-dose intravenous vitamin C reduced net fluid balance requirements, reduced plasma lipid peroxidation, and maintained overall oxidant status.30 In a randomized, prospective study in humans, adjuvant administration of high-dose intravenous vitamin C within 24 hours after injury reduced fluid resuscitation requirements and wound edema and provided an apparent improvement in respiratory function.31 Although controlled studies in dogs to determine the optimal high dose of vitamin C are lacking, the recommended dose has been extrapolated from human- and animal-model studies and ranges from 14-66 mg/kg IV per hour within the first 24 hours after thermal injury.14,31,32
Prognosis
Superficial burns generally heal in 3 to 5 days and leave no scarring. Superficial partial-thickness burns heal in 1 to 2 weeks with minimal scar formation. Deep partial-thickness burns heal in 2 to 3 weeks and require surgical intervention to avoid substantial scar formation. Full-thickness burns heal slowly and also require surgical intervention (eg, undermining and advancement of adjacent skin, skin flaps, axial pattern flaps, skin grafts, skin stretching techniques); these burns can result in deformation and hypertrophic scarring.3,8,9 A higher risk for mortality is expected in patients that develop respiratory dysfunction due to severe burn injuries and smoke inhalation.14,33