Anesthetic Management in a Hyperthyroid Cat
Berit Fischer, DVM, DACVAA, CCRP, CVA, Crown Veterinary Specialists, Lebanon, New Jersey
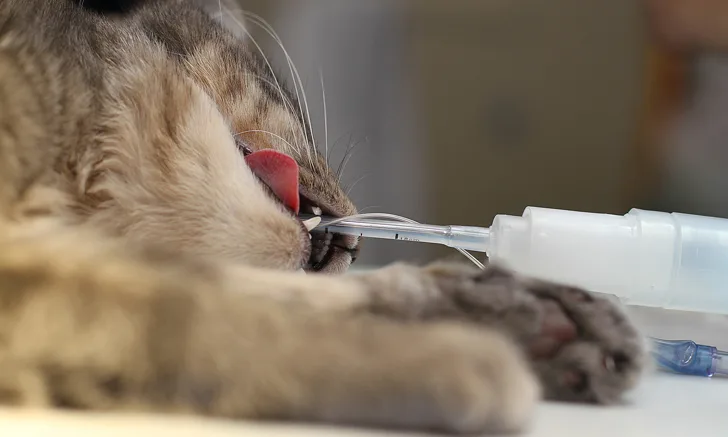
Buttercup, a 12-year-old spayed domestic shorthair cat, is presented for a preanesthetic examination prior to removal of a previously diagnosed, ulcerated basal cell carcinoma on the dorsal aspect of the neck measuring 1.0 × 1.0 × 0.5 cm.
Buttercup had been diagnosed with hyperthyroidism 4 months prior and was initially treated with methimazole; however, because of intolerable side effects (ie, pruritus, diarrhea), she was switched to a low-iodine prescription diet. Her owner reports that Buttercup has shown clinical improvement (ie, less polyuria/polydipsia and vomiting) since starting the low-iodine diet.
An echocardiogram performed when hyperthyroidism was first diagnosed showed mild eccentric hypertrophy of the left ventricle, thickening of the intraventricular septum, and benign right ventricular outflow tract obstruction.
CBC and serum chemistry profile results from 4 days before presentation are relatively unremarkable, other than a mildly elevated ALT of 185 U/L (reference range, 27-158 U/L) and blood glucose of 198 mg/dL (reference range, 72-175 mg/dL). Total thyroxine (TT4) is still elevated at 5.5 μg/dL (reference range, 0.8-4.7 μg/dL) but is greatly improved from 4 months prior, when TT4 was 10.3 μg/dL.
On physical examination, the patient is thin (BCS 3/9) and appears euhydrated. She is visibly nervous and resists restraint, behavior that is atypical from her previous visits. Temperature is 102.5°F (39.2°C), heart rate is 254 bpm, and respiratory rate is 51 breaths/min. A grade 2/6 systolic parasternal murmur and gallop rhythm are present with synchronous and bounding pulses. Lungs are clear on auscultation, but increased effort is noted. A thyroid slip is palpable. Average blood pressure* after 5 readings is 196/93 mm Hg (MAP, 127 mm Hg). The owner expresses concern that Buttercup has not been this agitated at home and became more upset in the waiting room when surrounded by dogs.
*All blood pressure values are provided in a systolic/diastolic (mean arterial pressure [MAP]) format.
MAP = mean arterial pressure, TT3 = total triiodothyronine, TT4= total thyroxine