Anesthesia Monitoring & Pulse Oximeters
Pulse oximetry is a simple, noninvasive method of monitoring arterial hemoglobin oxygen saturation. It also can provide information about a patient's heart rate. Both the American College of Veterinary Anesthesiologists and the American Animal Hospital Association recommend the use of pulse oximetry in anesthetized veterinary patients.
Oximetry is based on the Lambert-Beer law, which relates the absorption of light by a solution (in this case, blood and specifically hemoglobin) to the concentration of a desired substance (in this case, oxygen). If all the light passes through a solution without any absorption, then the amount absorbed is zero and percent transmittance is 100%. If all the light is absorbed, then percent transmittance is zero, and absorption is infinite.
Oxygenated hemoglobin absorbs light in the infrared spectrum (920 to 960 nm) whereas deoxygenated hemoglobin absorbs light in the red spectrum (640 to 660 nm). Analysis of the differential absorption spectra of oxygenated and deoxygenated hemoglobin by the microprocessor in the monitor provides a value for oxygen saturation. Further analysis of pulsatile flow differentiates arterial and venous blood. A pulse oximeter provides arterial oxygen saturation by detecting pulse rate and differentiating the ratio of light absorption during pulsatile and nonpulsatile flow.
Another oximetry device, the cooximeter, uses additional wavelengths of light to differentiate other forms of hemoglobin (eg, carboxyhemoglobin or methemoglobin) in arterial or venous blood. Typically SaO2 refers to oxygen saturation obtained by the cooximeter from an arterial blood sample whereas SpO2 refers to arterial oxygen saturation obtained by the pulse oximeter.
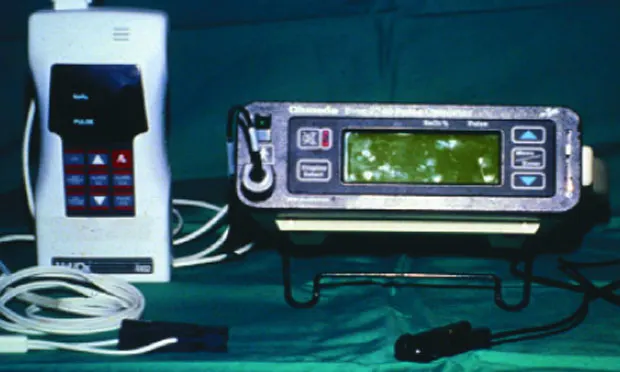
Pulse oximetry requires placing a probe onto a tissue bed with pulsatile flow. There are 2 common probe configurations (Figure 1): A reflectance probe has light emitting photodiodes and a photodetector located on the same side of the tissue bed. A transmittance probe has the photodiodes and photodetector located on opposite sides of the tissue bed.
IndicationsIdeally oxygen saturation should be monitored both during surgery and anesthetic recovery, when a decrease in oxygenation is possible since the patient is no longer breathing a high-inspired oxygen concentration (FiO2). Pulse oximeters are especially useful in patients where oxygenation is compromised by the patient's condition (eg, diaphragmatic hernia, pulmonary conditions, etc), the nature of the procedure (eg, lung lobe resection, diaphragmatic hernia repair, etc), or due to anticipated physiologic changes (ventilation/perfusion abnormality) resulting from recumbency.
Pulse oximetry is critical for patient safety during specialty procedures such as bronchoscopic evaluation or when nitrous oxide is used as part of the anesthetic protocol. It is also used to evaluate oxygenation during mechanical ventilation or in nonanesthetized critically ill patients.
Because they provide continuous information regarding oxygenation, pulse oximeters are frequently used to guide the need for blood gas analysis. Many are battery operated and as a result are portable for use outside the hospital. There are no contraindications to use of pulse oximeters.
AdvantagesAs stated previously, pulse oximeters are simple to use, noninvasive, and provide continuous information about patient oxygenation. In addition, they may be used on a broad spectrum of mammalian veterinary patients.
Application to the patient necessitates placing the probe in an appropriate location: Transmittance probes have historically been designed for the human earlobe or finger; in veterinary medicine they are most commonly placed on the tongue (Figure 2A). Alternative sites vary with species and include the lip, digits, ear, vulvar folds or prepuce, and tail (Figure 2B).
Reflectance probes are usually placed in the esophagus, rectum, or vagina. Transmittance probes are most commonly used in veterinary medicine; however, a reflectance probe may be used in an awake patient where motion does not allow for appropriate transmittance probe placement.
The display averages oxygen saturation associated with pulsatile flow and heart rate at approximately 10- to 20-second intervals. A waveform indicating amplitude of the pulse is a desirable feature and is available on most pulse oximeters (Figure 3). However, it is important to recognize that some monitors may adjust the gain or signal strength to maintain pulse amplitude and may mislead the observer.
Minimal training is required to enable a user to apply the probe and recognize an inappropriate reading.
LimitationsPulse oximeters measure saturation of hemoglobin but do not quantify available hemoglobin. Hence in an anemic patient the saturation percent may be in the normal range but tissue oxygenation, which is dependent on both oxygen content (Box) and regional blood or cardiac output, may be compromised.
Saturation is measured as a percentage with a maximum value of 100. Due to the nature of the oxygen hemoglobin dissociation curve, pulse oximeters are best used to detect life-threatening hypoxemia (PaO2 < 60 to 65 mm Hg) as indicated by values below 90% to 92%. They are unable to assess inadequacy of lung function at PaO2 values greater than 100 to 120 mm Hg as is the case for most patients breathing a high FiO2 during anesthesia (Figure 4). Keep in mind that pulse oximeters do not provide any direct information regarding adequacy of ventilation: a patient breathing high FiO2 may hypoventilate significantly without a change in oxygen saturation.
In general pulse oximeters tend to be most accurate (to about 2%) within the normal range (SpO2 90% to 100%). Their accuracy may be further influenced by pigment and tissue thickness, patient movement or shivering, ambient light, intravenous dyes, and poor perfusion. Abnormal hemoglobins, while not common in veterinary medicine, will also result in an erroneous reading. Carboxyhemoglobin will result in a falsely high reading (its absorption spectrum in the 660 nm wavelength is similar to that of oxyhemoglobin). The absorption coefficient for methemoglobin is the same for red and infrared light wavelengths, corresponding to a saturation of 85%.
The accuracy of pulse oximeters has not been verified for nonmammalian species.
Economic ImpactWhile there is no good documentation of the economic benefit of using a pulse oximeter during anesthetic management in veterinary patients, tissue hypoxia can result in an increased risk for complications (eg, blindness, renal compromise, etc). Cyanosis is a late clinical sign of poor oxygenation (seen with 5 g or more of desaturated hemoglobin) and further depends on the patient's hemoglobin level and circulation. In humans it has been suggested that pulse oximeters detect potentially adverse complications 60% to 90% faster than a trained clinician.
The primary costs are associated with the purchase of the monitor and probes. There are no ongoing costs for disposable supplies or routine unit maintenance/calibration. A monitor should last for years with proper care. A unit with a waveform and pulse display currently costs around $1000; replacement probes and cables begin at approximately $100. When one considers how easily pulse oximetry may be applied to each patient undergoing anesthesia and the information it provides, it is easily among the most cost-effective physiologic monitoring devices available.
OXYGEN CONTENT (mL/dL)=(1.36 × [Hb] × % saturation) + (PaO2 × 0.003)• Hemoglobin (Hb): Measured or approximated (1/3 packed cell volume)• Saturation: Pulse oximeter (%)• Partial pressure of oxygen in arterial blood (PaO2): Blood gas analyzer (mm Hg)95% saturation or better is desirable90% saturation or less indicates a problem with oxygenation100% saturation is the maximum reading
ANESTHESIA MONITORING & PULSE OXIMETERS • Khursheed Mama
Suggested ReadingAccuracy of a third (Dolphin Voyager) versus first generation pulse oximeter (Nellcor N-180) in predicting arterial oxygen saturation and pulse rate in the anesthetized dog. Burns PM, Driessen B, Boston R, Gunther RA. Vet Anaesth Analg 33:281-295, 2006.Practical applications of pulse oximetry. Hill E, Stoneham MD. Practical Procedures Issue 11, 2000, www.nda.ox.ac.uk/wfsa/html/u11/u1104_01.htm.Pulse oximetry. Fearnley SJ. Practical Procedures Issue 5, 1995, www.nda.ox.ac.uk/wfsa/html/u05/u05_003.htm. Pulse oximetry. Grubb T. In Greene SA (ed): Veterinary Anesthesia and Pain Management Secrets-Philadelphia: Hanley and Belfus, Inc, 2002. Respiratory monitoring during anesthesia: Pulse oximetry and capnography. Wright B, Hellyer PW. Compend Contin Educ Pract Vet 18:1083-1097, 1996.