Methicillin-Resistant Staphylococcal Infections
Karen A. Moriello, DVM, DACVD, University of Wisconsin–Madison
Darcie Kunder, VMD, DACVD, University of Pennsylvania
This article was previously published in an earlier issue of Clinician's Brief. It has been updated and modified for present use.
Staphylococcus species are part of the normal mammalian and avian flora, but the worldwide increase in methicillin-resistant infections is likely a reflection of increased antibiotic use.
PROFILE
Definition
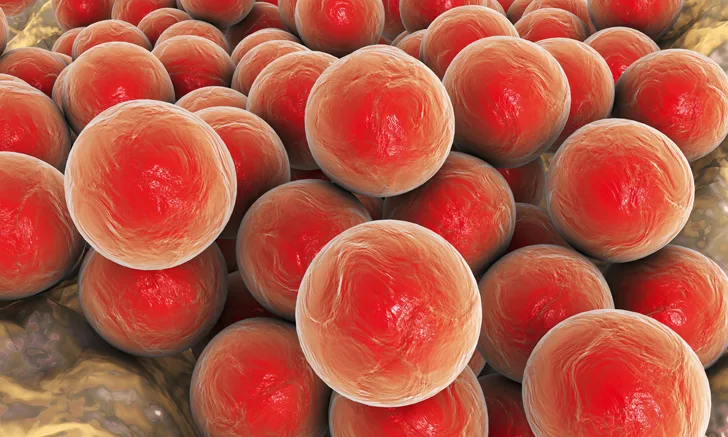
Staphylococcus bacteria (gram-positive, facultative, aerobic cocci) are opportunistic pathogens that can cause skin, body cavity, and soft-tissue infections when inflammation is present and/or the host has compromised defense mechanisms.
S pseudintermedius, S schleiferi (both coagulase-positive and -negative variants), and, to a lesser extent, S aureus are important organisms in veterinary medicine.
Molecular testing has determined that the primary pathogen of dogs is S pseudintermedius; previous S intermedius isolates are now believed to have been S pseudintermedius.
The occurrence of methicillin-resistant staphylococcal infections is increasing.
Methicillin resistance is encoded by the mecA gene, which confers intrinsic resistance to all β-lactam antibiotics (ie, penicillins, cephalosporins).
The gene is located on the staphylococcal chromosomal cassette along with other resistance genes. This allows resistance to multiple antimicrobials.
In humans, methicillin-resistant S aureus (MRSA) can be hospital- or community-acquired.
Human or animal S aureus carriers without clinical signs are classified as colonized.
Studies have shown that up to 30% of humans have nasal colonization of S aureus; approximately 0.5% of those isolates are MRSA.1,2
The Big Misnomer
Although methicillin resistance is the common term, today oxacillin is the antibiotic used for susceptibility testing, as methicillin is no longer manufactured and oxacillin is considered more stable.
Systems
Skin, soft tissue, and the ears are the most common sites of methicillin-resistant infection; however, any organ has the potential for infection.
Geographic Distribution
Methicillin resistance has been noted worldwide in humans and animals, but prevalence of MRSA and methicillin-resistant S pseudintermedius (MRSP) varies widely with geographic distribution.
MRSP can be found in or on clinically healthy dogs and cats. Reported prevalence of colonization ranged from 1.5% to 17% in healthy dogs and in healthy cats was 1.2%.3
Signalment
Methicillin resistance can occur in dogs and cats of any age, breed, or sex.
Veterinary Antimicrobial Susceptibility Testing Recommendations
The Veterinary Antimicrobial Susceptibility Testing subcommittee recently made the following recommendations regarding methicillin resistance
Proposed use of new oxacillin disk diffusion standards (R ≤17 mm) and MIC breakpoints (R ≥0.5 µg/mL) as indicators of mecA-mediated resistance for S pseudintermedius.
The cefoxitin test should not be used for detecting methicillin resistance in S pseudintermedius isolates from dogs. The cefoxitin breakpoints are not predictive of mecA-mediated resistance to methicillin or oxacillin in S pseudintermedius.
Transmission & Risk Factors
Pets are most likely to contract S aureus or MRSA from humans.
Studies have shown that <4% of healthy dogs and cats are colonized with MRSA.
Risk factors for MRSA in pets include infections related to surgery, hospitalization, prior antibiotic use, or exposure to humans with MRSA. Therapy pets in hospital visitation programs are also at increased risk.
Pets can acquire MRSP via animal-to-animal contact where healthy colonized pets are the likely source. Receiving recent (within the last year) systemic antimicrobial therapy has also been shown to be a risk factor for acquisition of methicillin-resistant staphylococcal species. Systemic therapy may alter a patient’s commensal staphylococcal flora and allow drug-resistant strains to colonize.
Signs
Clinical signs of methicillin-resistant infections are identical to methicillin-sensitive infections. Clinical suspicion of methicillin resistance includes lack of response to appropriate empiric therapy, worsening of signs while receiving therapy, and/or recurrent infections (particularly of the skin and ears).
DIAGNOSIS*
Definitive
Speciation of S pseudintermedius, S intermedius, and S delphini requires molecular testing; for simplification purposes, isolates from these species are typically referred to as S pseudintermedius.
S schleiferi and S aureus can be identified by standard laboratory speciation test kits.
Methicillin resistance requires culture and susceptibility testing via broth or agar-based tests.4
Accurate detection of methicillin resistance can be difficult because of heteroresistance (ie, the presence of 2 subpopulations [1 susceptible, the other resistant] that can coexist within a culture).
These cells grow more slowly than oxacillin-susceptible populations and longer incubation periods are required to avoid missing the diagnosis.5
PCR assay is considered the gold standard for detection of the mecA gene.
Other Diagnostics
Many methicillin-resistant staphylococcal infections in dogs and cats are complicated by secondary yeast overgrowth; cytologic examination of glass microscope slides or clear acetate tape is useful to identify organisms.
TREATMENT
Inpatient/Outpatient
Inpatient care is indicated only if the animal requires surgery, surgical debridement, or supportive care because of organ involvement.
DO NOT PANIC
Television, internet, and news media have made clients aware (or frightened) of methicillin resistance. In addition to directing clients to trusted websites (eg, wormsandgermsblog.com) for more information, some key points to stress include:
Do not panic.
MRSA and MRSP are not the same.
If MRSA is isolated in the pet, then the most likely source is a human.
Colonization of humans with MRSP is transient, if it occurs at all — MRSP and MRSA have very low zoonotic risk.
Wash your hands.
Medical
All MRSP/MRSA infections are resistant to β-lactam antibiotics; some strains may be resistant to other antibiotics.
Systemic antibiotic selection must be based on culture and susceptibility testing. Length of treatment will depend on severity of infection but is usually no less than 21 to 30 days.
Topical and local therapy (antibacterial shampoos; ointments; leave-on solution; sprays, lotions, or wipes; flushing of abscesses) may be beneficial. This is an underused tool and can be performed in conjunction with appropriate systemic antimicrobrial therapy. Topical therapy can also help prevent recurrence of infection once systemic therapy is complete.
Secondary yeast infections should be treated appropriately.
Grooming and clipping hair from affected areas is crucial in long- or heavy-coated patients.
Decolonization of healthy animals with MRSA is not necessary and is not recommended for healthy animals with MRSP or methicillin-resistant S schleiferi (MRSS). The optimal strategy and efficacy of decolonization practices have not been well-established or well-documented in veterinary medicine. Staphylococcal colonization is widespread over the entire skin and mucosal surfaces so targeted decolonization is difficult.
Careful search for the underlying trigger is critical, particularly when the patient history includes use of multiple antibiotics and/or chronic skin or ear disease.
Activity
Limiting activity is not indicated unless the infected area requires immobilization or bandaging.
Infected or colonized dogs should be exercised where they will not encounter other dogs.
Infected or colonized cats should be kept indoors.
MEDICATIONS
Topical Therapy
Therapy with benzoyl peroxide or chlorhexidine shampoo q24h to q48h is helpful as adjuvant therapy in pets receiving systemic antibiotics.
Multidrug-resistant staphylococcal infections require intensive daily bathing. It is recommended to use 4% chlorhexidine gluconate or chlorhexidine gluconate with tris-EDTA. Medicated bathing is different from a normal grooming bath. Using lukewarm water is preferred so as not to irritate inflamed skin. A minimum contact time of 10 minutes with the shampoo on the skin is ideal for targeting surface bacteria. This should be followed by a thorough rinse.
Mupirocin ointment can be used on focal areas of infection.
At-Home Measures
Hand hygiene (eg, soap and water, alcohol-based hand sanitizers) is best for preventing transmission of infection.
While infection is active, discourage owners from kissing their pet or allowing the pet to lick them.
The pet’s bedding, collars, and clothing should be washed daily or every other day.
During treatment, owners should not allow the pet to sleep in their bed or with children.
Staphylococci can persist in the environment; routine cleaning can be protective.
Systemic Antibiotics
Selection of an antimicrobial agent is based on culture and susceptibility testing.
Use of vancomycin and linezolid in veterinary patients is controversial because of ethical concerns; these drugs are reserved for treatment of MRSA in humans.
Adverse reactions to potentiated sulfonamides (30 mg/kg PO q12h) and chloramphenicol (50 mg/kg PO q8h) can occur. Clients should be warned of idiosyncratic bone marrow suppression, which rarely occurs with chloramphenicol use in humans.6
FOLLOW-UP
Patient Monitoring
Resolution of the infection is monitored by clinical response. Treatment needs to continue beyond resolution of clinical signs. For superficial infections, treatment is recommended for 1 week past clinical resolution; for deeper infections, treatment for 2 weeks past clinical resolution is best.
After resolution of signs, repeat culture is not recommended. Persistence of MRSP on carriage sites is common following resolution of the infection (eg, pyoderma).
Complications
Patients receiving potentiated sulfonamide antibiotics optimally should have tear production monitored before treatment is initiated and during treatment if keratoconjunctivitis sicca is suspected.
Chloramphenicol can cause nausea. Drug-induced bone marrow suppression is a rare side effect, but monitoring CBC results is recommended if the patient shows signs of the condition or if chloramphenicol therapy is used for extended periods (>4 weeks).
MRSP Illustrated
null
A dog was presented with a 3-month history of severe lameness and swelling of the lower leg. Culture of a draining tract between the foot pads (A) revealed MRSP infection susceptible to chloramphenicol. After 5 days of treatment, the paw was markedly improved (B). The dog made a full recovery.


IN GENERAL
Prognosis
Prognosis depends on the site and extent of infection; early intervention in surgical wounds and soft-tissue injuries is important.
Multidrug-resistant infections often have a poorer prognosis because of the time and effort required to treat them.
Future Considerations
Minimization or prevention of methicillin resistance will require thoughtful use of antibiotics and consideration of topical agents as first lines of therapy. Treatment based on culture is becoming the standard of care.
*Addendum: Per CLSI guidelines, latex agglutination testing for the altered penicillin binding protein (PBP2a) can be used as a screening testing for methicillin resistance in Staphylococcus spp isolates. Multiple testing methods are preferred to confirm presence of mecA and PBP2a.7
MRSA = methicillin-resistant _S aureus, MRSP = methicillin-resistant S pseudintermedius, MRSS = methicillin-resistant _S schleiferi__