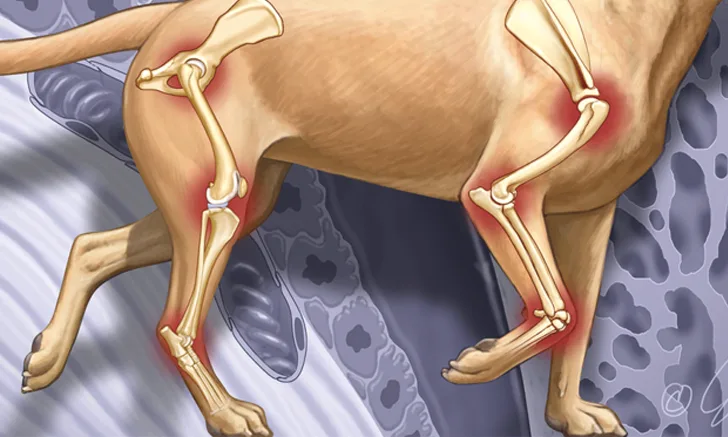
Which Drugs Can Be Used for Osteoarthritis in Dogs?
Kelley Thieman Mankin, DVM, MS, DACVS (Small Animal), Texas A&M University
NSAIDs
As mainstay treatment for osteoarthritis (OA), NSAIDs inhibit one or more steps in arachidonic acid metabolism, including inhibition of prostaglandins by cyclooxygenase (COX).
COX Isoforms: COX-1 and COX-2 are known isoforms; COX-3 was recently recognized.1
COX-1 catalyzes formation of constitutive prostaglandins.2
COX-2 appears to catalyze formation of induced prostaglandins expressed in damaged or inflamed tissue.2
Also involved in pain response to injury
Recently COX-3, a brain-specific COX-1 variant, was identified in dogs.3
Preferentially inhibited by acetaminophen
One NSAID may work better than another for an individual dog, with different classes of NSAIDs having different side effect profiles.6
Inhibition of COX-2: Thought to supply desired benefits of NSAID administration by
Inhibiting induced prostaglandins
Avoiding unwanted NSAID side effects of inhibiting constitutive prostaglandins
Recent studies: COX-2 may have some activity in constitutive prostaglandins, and COX-1 may have some activity in induced prostaglandins.4,5
COX-1 and COX-2 inhibition, therefore, is not clear-cut.4,5
In addition, little difference in improvement of clinical signs has been detected in studies comparing different NSAIDs with different COX-2 selectivity as administered to large groups of dogs.6
One NSAID may work better than another for an individual dog, with different classes of NSAIDs having different side effect profiles.6
Carprofen
Carprofen, one of the first COX-2 preferential NSAIDs approved for dogs, has been shown to be effective treatment for canine OA.7-9
Formulation: Oral, injectable
Dose: 4.4 mg/kg q24h or divided 2.2 mg/kg q12h<sup6,10 sup>
Key Points
Dose-dependent side effects include
Anorexia, vomiting, diarrhea
In dehydrated or older dogs, renal decompensation11
Idiosyncratic hepatotoxicity associated with markedly increased serum ALT occurs less commonly but can lead to acute hepatic failure.12
Reported more commonly in the Labrador retriever as compared with other breeds12
Meloxicam
Clinical trials have shown meloxicam to be effective treatment for OA in dogs.13-15 Like carprofen, meloxicam preferentially inhibits COX-2.
Formulation: Oral (tablet or liquid), injectable
Dose: 0.1 mg/kg q24h<sup6,10 sup>
Key Points
Like carprofen, most commonly reported side effects are
Anorexia, vomiting, diarrhea14
The following severe adverse events can occur with meloxicam administration
Hepatotoxicity10,16
GI ulceration, including perforating ulcers10,17
Deracoxib
Deracoxib, a COX-2 selective NSAID as compared with being COX-2 preferential, is labeled for treatment of canine OA.
Formulation: Oral (chewable tablet)
Dose: 1–2 mg/kg q24h<sup6,10 sup>
Key Points
Approved for treatment of pain and inflammation associated with OA in dogs
Effective in controlling pain associated with induced synovitis18,19
Clinical trials have shown that deracoxib is effective at improving signs associated with OA.20,21
The NSAIDs presented here have all been approved for use in dogs with osteoarthritis and/or associated clinical signs.
When administered at doses higher than labeled, dogs reportedly developed kidney abnormalities.22
Caution/Warning
While no kidney problems have been reported in dogs receiving the recommended dose, deracoxib should be used with caution in dogs with renal disease.
Has been associated with GI ulceration and perforation, particularly with administration of higher than recommended doses or in combination with another NSAID or glucocorticoid23,24
Firocoxib
Firocoxib, approved for treatment of canine OA, is a COX-2 selective NSAID shown to be effective in treating pain and inflammation associated with induced synovitis.8
Formulation: Oral (chewable tablet)
Dose: 5 mg/kg q24h6,10
Key Points
In a study comparing firocoxib with carprofen, fewer dogs experienced health problems with firocoxib than with carpofen.8
The most frequent side effects are vomiting and decreased appetite.
Margin of safety is narrow in puppies.
Label Warning
Using doses higher than recommended in puppies younger than 7 months of age has been associated with serious complications, including hepatic abnormalities and decreased weight gain.
Chondroprotectants
Chondroitin Sulfate–Glucosamine Hydrochloride–Manganese Ascorbate
Chondroitin sulfate–glucosamine hydrochloride–manganese ascorbate is proposed to reduce clinical signs of OA and slow or prevent progression of the degenerative process.
Formulation: Oral (chewable tablet)
Dose: Varies based on dog’s weight; refer to product label for recommended initial and maintenance dose schedules for joint disease in dogs
Key Points
Glucosamine hydrochloride and chondroitin sulfate have been shown to accumulate in plasma after multiple doses and to have substantial carryover effect.25
This drug combination can produce beneficial effects in vitro, protect against synovitis,26 slow the degenerative process,27 and modulate metabolism of articular cartilage.28
When administered to dogs in vivo, results have not been as promising.
One clinical study in dogs showed no improvement in objective gait analysis or subjective analysis by owner or orthopedic surgeon during the study period.13
Ground reaction forces measured before and after were not significantly improved.
Glucosamine Hydrochloride–Chondroitin Sulfate–Avocado/Soybean Unsaponifiables
The combination of glucosamine hydrochloride–chondroitin sulfate–avocado/soybean unsaponifiables (ASU) is similar to chondroitin sulfate–glucosamine hydrochloride–manganese ascorbate and likewise is purported to reduce clinical signs of OA and slow or prevent progression of the degenerative process.
Formulation: Oral (chewable tablet)
Dose: Varies based on dog’s weight; refer to product label for recommended initial and maintenance dose schedules for joint disease in dogs
Key Points
Numerous research studies have shown that ASU can decrease inflammation at the cellular level, decrease cartilage degradation, and promote cartilage repair.29-31
Can partially reverse the effects of IL-1 on chondrocytes and decrease matrix metalloproteinase (MMP) production, decreasing inflammation and cartilage degradation29,30
Can increase expression of TGF-β, suggesting stimulation of cartilage repair31,32
An experimental study evaluating ASU administered to dogs with transected cranial cruciate ligaments found reduced development of cartilage and subchondral bone lesions.33
Study authors suspected that ASU worked by inhibiting nitric oxide synthase and MMP-13.<sup33 sup>
Hyaluronan
Hyaluronan, also known as hyaluronic acid (HA), is a polysaccharide found in many tissues. HA is concentrated in synovial fluid, where its major function is to bind water and lubricate joints.
Formulation: Injection (intraarticular)
Dose: Using high molecular weight hyaluronan compound, 10 mg weekly34-36; in Plumb’s Veterinary Drug Handbook, 3–5 mg/kg weekly also recommended for adjunct treatment of synovitis
Follow aseptic technique
Key Points
Most commonly administered directly into the joint.
By this route, HA has been shown to improve gait function in OA mouse models.37
Avocado/soybean unsaponifiables can decrease inflammation and cartilage degradation and promote cartilage repair.29-31
In human studies, intraarticular HA improved viscoelasticity, provided antiinflammatory activity, provided analgesia, and decreased degradation of articular cartilage.38,39
Studies showed no clinical improvement or prevention of OA when administered to dogs with transected cranial cruciate ligaments.34-36,40
Polysulfated Glycosaminoglycan
Polysulfated glycosaminoglycan (PSGAG) is labeled as a disease-modifying OA supplement purported to slow OA development and diminish associated clinical signs.
Formulation: Injection (IM)
For treatment of noninfectious, traumatic, or degenerative arthritis41
Dose: 4.4–5 mg/kg IM twice weekly for 4 weeks (recommended)42,43
Key Points
In one study, 75% of dogs had significantly improved lameness scores after treatment with PSGAG.42
Potential use in inhibiting cartilage matrix degradation42
Full mechanism of action is unknown but has been shown to decrease COMP (cartilage oligomeric matrix protein), a substrate for catabolic MMP enzymes.42
May increase synthesis of collagen (in vitro)<sup44 sup>
Young puppies treated with PSGAGs showed less hip subluxation than did untreated puppies.45
Warning
Similar in structure to heparin and should not be used in dogs with coagulation abnormalities41
Analgesics
Tramadol
Tramadol is a central-acting synthetic opiate-like (mu-receptor) agonist. Its mechanism of action involves numerous metabolites.
Formulation: Oral (tablet)
Dose: 4–10 mg/kg q8h46
Key Points
Now a class IV schedule drug
In part, analgesia may be achieved because tramadol and its metabolites are opiate-like mu-receptor agonists.
Because of how dogs metabolize tramadol, they are not expected to experience substantial opioid effects.46
Mechanism of action in dogs likely results from metabolites acting as serotonin and norepinephrine reuptake inhibitors.46
Shown to be effective in alleviating clinical signs of OA in dogs<sup47 sup>
Sedation most common side effect; dogs may develop decreased bioavailability over time (ie, tramadol may undergo decreased absorption with multiple doses).46
Evidence that tramadol alone has a detrimental effect on gastric barrier function is lacking.48
Caution
Dose adjustments may be required in dogs with impaired renal or hepatic function.
Gabapentin & Pregabalin
Both gabapentin and pregabalin were developed as antiepileptic drugs but have been used for treatment of chronic pain.46
Formulation: Oral (liquid or capsule)
Dose recommended (empiric) for gabapentin: 10–20 mg/kg q8h46
Dose recommended for pregabalin: 4 mg/kg q12h46
Key Points
Both are alkylated analogs of gamma-aminobutyric acid (GABA).
Believed to work by blocking voltage-gated calcium channels, reducing neurotransmitter release, and attenuating postsynaptic excitability
Suspected neuropathic pain has been successfully treated with gabapentin.49
Therapeutic success has been achieved with certain analgesics as treatment for chronic pain and inflammation prevalent in dogs with osteoarthritis.
Although both drugs are reportedly effective treatment for chronic pain in humans, no studies have evaluated gabapentin or pregabalin for management of canine OA.
Studies have shown no significant benefit to administration of gabapentin as an adjunct to other analgesics in dogs undergoing forelimb amputation or intervertebral disk surgery.50,51
Caution
Gabapentin liquid contains xylitol; however, the concentration of xylitol in the liquid is low enough that routine dosing of gabapentin is unlikely to result in toxicity.46
Amantadine
Amantadine, first used as an antiviral medication against influenza in humans, is now primarily prescribed for pain relief in both human and veterinary medicine because of its ability to inhibit the N-methyl-D-aspartate (NMDA) receptor.
Formulation: Oral (liquid or tablet)
Dose (recommended): 3–5 mg/kg q24h46
Key Points
Should not be used as sole therapy for OA but should be combined with and may enhance the effects of NSAIDs, opioids, or gabapentin or pregabalin46
Inhibits the NMDA receptor by encouraging channel closure and inhibiting NMDA responses
In one study of dogs with OA pain refractory to NSAID treatment, addition of amantadine to NSAID therapy resulted in improved function, presumably because of pain relief.52
In the same study, no adverse effects or significant changes in laboratory results were detected.
Other Oral Supplements
Dried Milk Protein
Collected from hyperimmunized cows; purported to contain factors that block cytokines and inhibit neutrophil participation in an inflammatory response
One clinical trial reported improvement in clinical signs of OA.53
Green-Lipped Mussel Extract
Green-lipped mussel extract (GLME; Perna canaliculus) has improved clinical signs of canine OA.54
Long-term administration may be required.
How GLME exerts beneficial effects is unknown but suspected to be secondary to high concentrations of omega-3 fatty acids,55 which act as inhibitors of arachidonic acid metabolism by COX and lipoxygenase (LOX) pathways.<sup55,56 sup>
Has been shown to have antiinflammatory effects<sup57 sup>
Omega-3 Fatty Acids
Supplementation may lead to decreased inflammation.6
Higher blood levels were detected in dogs fed diets supplemented with omega-3 fatty acids; owners reported improved mobility in arthritic pets.58
Supplementation may allow reduced NSAID dose.59
S-Adenosyl ʟ-Methionine
S-adenosyl ʟ-methionine (SAMe), a nutraceutical most commonly used to treat canine liver disease, has no reported side effects in dogs.60
SAMe has antioxidant properties that may benefit osteoarthritic joints61 but in one study was not an effective standalone treatment for reducing clinical signs of OA in dogs.62
ALT = alanine aminotransferase, ASU = avocado/soybean unsaponifiables, COMP = cartilage oligomeric matrix protein, COX = cyclooxygenase, GABA = gamma-aminobutyric acid, GLME = green-lipped mussel extract, HA = hyaluronic acid, IL = interleukin, LOX = lipoxygenase, MMP = matrix metalloproteinase, NMDA = N-methyl-d-aspartate, PSGAG = polysulfated glycosaminoglycan, TGF = transforming growth factor, SAMe = S-adenosyl l-methionine