Caval Syndrome
Bonnie Heatwole, CVT, University of Florida
Amara H. Estrada, DVM, DACVIM (Cardiology), University of Florida
Ashley Jones, DVM, DACVIM (Cardiology), Trillium Veterinary Cardiology
Caval syndrome, a life-threatening heartworm disease characterized by heavy worm burden, prevents normal blood flow through the right side of the heart. Without proper therapy, death can occur 1 to 2 days after onset of clinical signs.
Presenting complaints may include tachypnea, cough, weakness, collapse, dyspnea, hemoptysis, and signs of right-sided congestive heart failure. Examination invariably reveals a right-sided systolic murmur (consistent with tricuspid regurgitation), gallop rhythm, or split S2 suggestive of pulmonary hypertension. Pulses are typically weak as a result of poor cardiac output.
Diagnosis
Clinical presentation and a positive heartworm antigen test are indicative of caval syndrome. Minimum database should include CBC, serum biochemistry profile, urinalysis, and thoracic radiography. Laboratory findings can include thrombocytopenia in patients with disseminated intravascular coagulation, hepatic and renal failure, hemoglobinuria, and proteinuria.
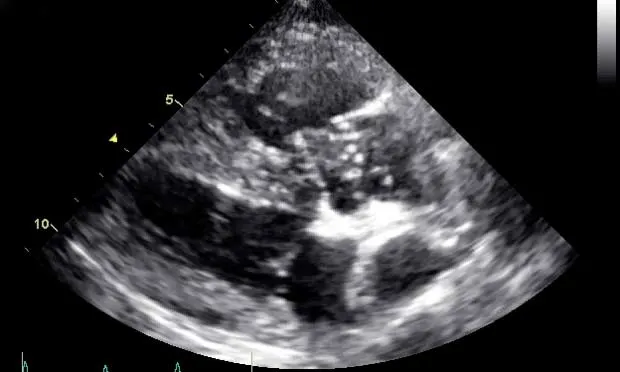
Thoracic radiography typically reveals right-sided cardiomegaly and dilated, tortuous pulmonary arteries. Echocardiography confirms caval syndrome by revealing heartworms across the tricuspid valve (Figure 1). and possibly in the right atrium, right ventricle, and vena cava. The right ventricle is usually dilated and concentrically hypertrophied. The left ventricle is small (as a result of volume underloading) secondary to diminished right-sided cardiac output.

Right parasternal transthoracic echocardiographic image showing typical heartworm echoes entwined around the tricuspid valve in the near field (arrow)
Treatment
Surgical removal of the heartworms is the only treatment option.
Perioperative treatment with heparin to minimize the risk for thromboembolism, diphenhydramine to offset antigen release from crushed worms during retrieval, and broad-spectrum antibiotics should be considered.
Local anesthesia can be sufficient for accessing the right jugular vein. A retrieval device (Figure 2) is passed into the right side of the heart, typically with ultrasonographic or fluoroscopic guidance.

Figure 2 Typical retrieval devices. (A) EnSnare Snare System (infinitimedical.com), (B) multipurpose helical basket (bostonscientific.com), (C) 4-prong retrieval forceps (hobbsmedical.com), (D) Ishihara heartworm removal forceps (no longer available), and (E) 8-Fr red rubber catheter with 0 polypropylene suture (kendallhq.com)


Typical retrieval devices. (A) EnSnare Snare System (infinitimedical.com), (B) multipurpose helical basket (bostonscientific.com), (C) 4-prong retrieval forceps (hobbsmedical.com), (D) Ishihara heartworm removal forceps (no longer available), and (E) 8-Fr red rubber catheter with 0 polypropylene suture (kendallhq.com)
Care should be taken to minimize damage to the tricuspid valve during retrieval and to avoid crushing the heartworms, which can lead to antigen release and anaphylaxis, especially in cats.
The procedure is complete after several passes fail to produce heartworms or when no heartworm echoes are identified. Patients should be treated with a standard heartworm preventive at discharge; adulticide therapy can be instituted once hepatic, renal, and hemodynamic parameters normalize (~3–4 weeks).
Prognosis
With worm removal, some report survival rates of 50% to 80%, but data on long-term survival are limited.1 It has been suggested that having substantially elevated alanine transaminase (ALT) levels coupled with echocardiographic evidence of worms in the pulmonary artery carries a poor prognosis.
For more, see Cardiac Examination and History by Dr. Daniel F. Hogan