Top 5 Liver Conditions in Cats
Craig B. Webb, PhD, DVM, DACVIM (Small Animal), Colorado State University
The feline liver is distinctly different from the canine liver in dysfunction, diseases, and normal metabolic function. Feline liver enzymology, while suitable for a carnivorous species, increases susceptibility to insult from drugs, toxins, metabolites, and oxidative stress. The serum biochemistry profile of a cat’s liver reflects differences in enzyme sensitivity and half-life, induction or lack thereof, and a seemingly unique response to anorexia.
Related Article: Chronic Liver Disease
TOP 5 Liver Presentations in Cats
1. Acute neutrophilic cholangitis (suppurative cholangiohepatitis)
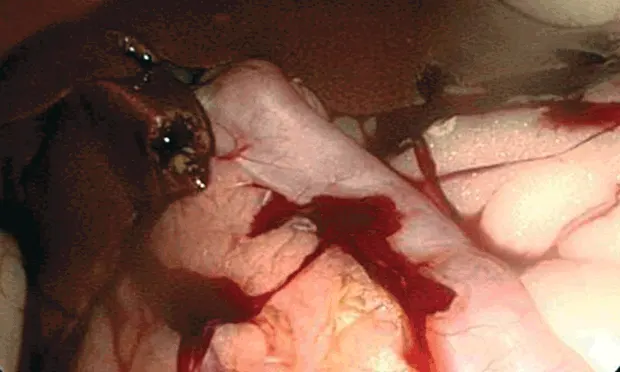
The WSAVA Liver Standardization Group recognized both the acute neutrophilic form (ANF) and chronic neutrophilic form (CNF) of neutrophilic cholangitis, although these may be different stages of the same condition.1 The acute suppurative form may be mediated by enteric bacteria (eg, Escherichia coli, Enterococcus spp, Bacteroides spp). ANF is found primarily in young to middle-aged cats presenting with acute onset anorexia, vomiting, lethargy, and diarrhea; they may be dehydrated, febrile, and jaundiced with abdominal discomfort. Liver enzymes and total bilirubin are elevated while other biochemical abnormalities (eg, azotemia, electrolyte imbalances) are nonspecific.Ultrasonography may reveal bile duct distention (secondary to pancreatitis) or gallbladder sludge and may help guide fine-needle liver aspiration and diagnosis of cholecystitis. Laparoscopy can be used to examine liver and biliary systems, procure samples for hepatic histopathology, and guide spinal needle (22-gauge) placement for gallbladder aspiration. Because of a possible bacterial component, bile cytology and culture and sensitivity (both aerobic and anaerobic) of the hepatic parenchyma and gallbladder contents are important. Vitamin K1 at 0.5 to 1.5 mg/kg SC q12h for 3 doses is warranted before sample acquisition.
Antibiotic therapy is the cornerstone for ANF, based either on culture and sensitivity test results or an empiric choice to cover enteric organisms (usually gram-negative, anaerobes) with good hepatobiliary penetration. Cephalosporins, amoxicillin-clavulanic acid, fluoroquinolones, or combination therapy (enrofloxacin 5 mg/kg q24h, metronidazole 7.5 mg/kg q12h) are logical candidates (≥4–8 weeks). Supportive care with fluids, electrolytes, and complete and balanced nutrition should also be considered. Ursodiol at 10 to 15 mg/kg q24h and pain medications, such as buprenorphine at 0.01 to 0.03 mg/kg OTM q8h, may be indicated.
2. Chronic neutrophilic cholangitis (nonsuppurative or lymphoplasmacytic)
Histopathology reflects a shift in the predominant inflammatory cell type from neutrophils to a mixed population, including lymphocytes and plasma cells. Biliary hyperplasia and fibrosis may be present, reflecting this condition’s chronic nature. Cats with CNF cholangitis are usually older than those with ANF, and signs may be intermittent with weight loss. Cholestatic liver enzyme activity (ALP and gamma-glutamyltransferase [GGT]) is elevated more consistently than ALT or AST, and these cats are often jaundiced with elevated total bilirubin. Ultrasonography may demonstrate bile duct and gallbladder changes, and the liver parenchyma may be hyperechoic because of fibrosis. Histopathology is required for definitive diagnosis, and the procedures and samples are similar to ANF. Both bacterial and immune-mediated processes may be involved in the CNF.
These cats may also be treated with an extended course of antibiotics (4–8 weeks); prednisolone at 1 to 2 mg/kg q24h may be started concurrently or after several weeks of antibiotic therapy. Ursodiol is frequently used, and liver protectants and/or antioxidants (eg, SAMe, vitamin E, silymarin) should be considered.
3. Lymphocytic cholangitis (nonsuppurative cholangitis or cholangiohepatitis)
Cats with lymphocytic cholangitis (LC) present with signs and biochemical abnormalities similar to other cholangitis classes, but LC is more slowly progressive; its clinical presentation, including hepatomegaly, ascites, hyperglobulinemia, and lymphocytosis, may help distinguish this condition. Persian cats appear overrepresented. Differentials that can mimic LC include FIP, lymphoma, and extrahepatic bile duct obstruction (rare), making histopathologic diagnosis important. Even with histopathology, the distinction between LC and lymphoma may require special assays for designating clonality and gene rearrangement.
Opinions differ as to whether prednisolone at 2 mg/kg PO q12h for 14 to 21 days then tapered or ursodiol at 15 mg/kg q24h for ≥8 weeks should be the foundation of treatment. Both treatments are often used concurrently. Because cobalamin levels are measured more frequently and sometimes low (perhaps because of concurrent GI disease), cobalamin can be added at 250 µg/cat SC q7d.
4. Triaditis
Feline cholangitis is often complicated by concurrent pancreatitis and/or inflammatory bowel disease (IBD), forming triaditis. Although there may be subtle differences, the 3 conditions cannot be distinguished by presentation alone. For example, cats with IBD are more likely to present with diarrhea and less likely to be anorectic, and necrotizing pancreatitis may result in hyperglycemia. Therefore, a high index of suspicion is crucial for a complete diagnostic examination that may include fPLI testing (noting its high interassay variation, spiking, and recovery), folate, cobalamin, full abdominal ultrasonography, and histopathology of multiple abdominal organs (Figure 1).
Triaditis treatment is more complicated than that for one disease, but many supportive efforts are similar: adequate nutrition for an anorectic cat (mirtazapine, cobalamin, esophagostomy feeding tube [E-tube]), aggressive treatment for pain and vomiting (maropitant, buprenorphine), prolonged corticosteroid treatment for CNF cholangitis and IBD, or possibly more aggressive immunomodulation (chlorambucil, 4 mg/m2 PO q2d).
5. Feline hepatic lipidosis
Presentation of “fatty liver” or true hepatic lipidosis in cats is unique, characterized by excessive accumulation of triglycerides within hepatocytes and marked cholestasis resulting from biochemical changes induced by such factors as anorexia, insulin resistance, and arginine deficiency. A period of anorexia precedes presentation that may include lethargy, weight loss, jaundice, weakness, vomiting, and diarrhea. Signs of hepatic encephalopathy (eg, excessive salivation) can be present, although rarely so. The history, marked elevation in ALP (>ALT elevation), and minimal change in GGT suggest diagnosis. Other abnormalities may be seen in CBC results (eg, poikilocytosis, Heinz bodies) and serum biochemistry profiles (eg, hyperbilirubinemia, hypokalemia, hypophosphatemia, low BUN). Clotting times may be prolonged, and proteins induced by vitamin K absence or antagonism (PIVKA) are often elevated. The liver is enlarged on radiographs and hyperechoic on ultrasound. Determining underlying disease is essential, as hepatic lipidosis is frequently secondary to another condition, such as pancreatitis, intestinal disease, cholangitis, neoplasia, or infectious disease.
Hepatic lipidosis can be treated primarily through nutrition, frequently requiring an E-tube. Appetite stimulants (eg, mirtazapine) may be contraindicated in cats with hepatic lipidosis because of unknown metabolism variability by the liver. A nasogastric tube may be used while achieving IV fluid support and electrolyte correction during critical care (with attention to potassium, phosphorus, and magnesium), but E-tube use is more common. The cat should be treated with vitamin K1 at 0.5 to 1.5 mg/kg SC q12h for 24 to 48 hours before E-tube placement, fine-needle aspiration of the liver, or obtaining hepatic biopsy specimens. A high-protein, low-carbohydrate diet can be blended and small, frequent feedings initiated, gradually increasing to the cat’s total daily requirement (usually over 4–5 days). Nonspecific supportive care may include maropitant at 1 mg/kg q24h or ondansetron at 0.22 to 0.5 mg/kg q12h (should vomiting occur), continued vitamin K1 at 2.5 mg/cat q24h, cobalamin at 250 µg/cat SC q7d, l-carnitine at 250 mg/cat q24h, and SAMe at 20 mg/kg q24h (increasing the dose by 50% if crushed and given through a feeding tube).
Nonspecific clinical signs and biochemical changes highlight the importance of a diligent diagnostic examination, remembering that although the liver may be the center of the disease process, it might also be only one component of what is making the cat ill.