Primary Hyperparathyroidism
PROFILE
Primary hyperparathyroidism (PHPT) and primary hypoparathyroidism are the most common primary parathyroid gland diseases.
Two external parathyroid glands lie outside the thyroid capsule, and two internal parathyroid glands are embedded within the thyroid parenchyma.1
Parathyroid glands synthesize and secrete parathyroid hormone (PTH) from chief cells.2
PTH increases plasma calcium concentration by mobilizing calcium from bone, increasing renal calcium reabsorption, and promoting formation of calcitriol, which increases intestinal calcium absorption.
PTH promotes phosphaturia by decreasing renal phosphorus reabsorption.
Parathyroid gland diseases are characterized by abnormalities in serum calcium and phosphorus concentrations.
Clinical signs are frequently secondary to serum calcium abnormalities.
Parathyroid glands may also be affected secondary to other disease states (eg, renal secondary hyperparathyroidism).
Related Article: Anesthesia for Parathyroid Disease
Definition & Pathophysiology3,4
Excessive PTH production from autonomously functioning chief cells, usually in a single parathyroid adenoma
Parathyroid carcinoma, hyperplasia, or multiple parathyroid adenomas are possible but rare.
Systems
Urinary, neuromuscular, and GI signs are possible.
Incidence & Prevalence
Accounts for ~13% of dogs with ionized hypercalcemia5
PHPT is caused by adenoma of the parathyroid gland (75%–85% of cases), hyperplasia (5%–15% of cases), and carcinoma (5%–10% of cases).4,6,7
Rarer in cats8
More common causes of hypercalcemia in cats include renal failure and idiopathic hypercalcemia (see Table)
Related Article: Polyuria, Polydipsia, & Hypercalcemia
Signalment
Breed Predilection
Autosomal dominant inheritance causes increased prevalence in keeshonds,9 but PHPT should be considered as a differential for any dog or cat with hypercalcemia.
Age & Range
Middle-aged to geriatric dogs
Sex Predilection
No known predilection
Related Article: Hypercalcemia in Dogs and Cats
Clinical Signs<sup3,6 sup>
Mainly attributable to hypercalcemia, which may be found incidentally:
Up to 35% of patients show no clinical signs.
Affected patients often appear healthier than those with other causes of hypercalcemia (eg, lymphoma).
Causes(s) and approximate frequency of clinical signs:
Polyuria/polydipsia from decreased renal tubular response to antidiuretic hormone (50%–60%)
Hematuria, stranguria, pollakiuria, urinary tract infection, and urinary tract obstruction (50%)
Calcium phosphate or oxalate urolithiasis may result from calciuria and phosphaturia.
Dilute urine-specific gravity predisposes patients to infection.
Lethargy, muscle wasting, and stiffness from decreased neuromuscular tissue excitability (40%–45%)
Inappetence (37%), vomiting (13%), and constipation (6%) caused by decreased excitability and motility of GI smooth muscle
Physical Examination
Patients may appear lethargic or weak.
A cervical mass may be palpated in cats.
A palpable parathyroid mass is rare in dogs.
A palpated mass could represent an alternative cause of hypercalcemia (eg, thyroid carcinoma).
Examination should not identify any finding consistent with other causes of hypercalcemia (eg, lymphadenopathy).
DIAGNOSIS
Definitive
Histologic examination of parathyroid gland mass(es) following successful surgical removal/ablation and resolution of hypercalcemia
Plasma PTH can be measured to support diagnosis.
Differentials
Differential diagnoses for hypercalcemia can vary (see Table)
Laboratory Findings
Chemistry panel: total hypercalcemia, decreased or borderline-low serum phosphorus concentration, possible azotemia
Ionized hypercalcemia in >90% of cases3
Urinalysis: frequent hyposthenuria or isosthenuria
Crystalluria, bacteriuria, hematuria, and pyuria are possible.
Imaging
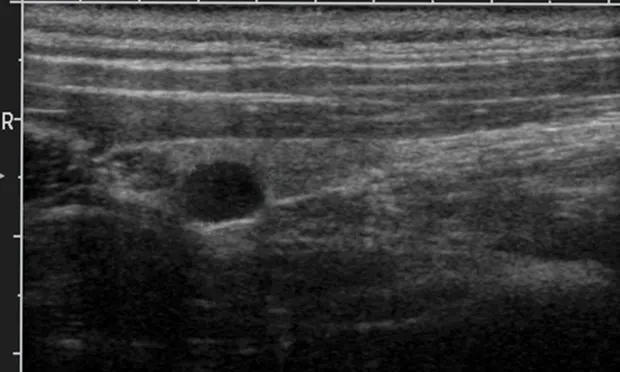
Ventral neck ultrasonography may identify parathyroid masses (see Figure 1, Cervical ultrasound of parathyroid mass (yellow arrow) within the parenchyma of a thyroid gland lobe (white arrow).
Most masses are small (4–9 mm in diameter).
Ultrasonography can be highly sensitive and is operator-dependent.
Parathyroid scintigraphy with Technetium (99mTc) sestamibi, nuclear medicine imaging, can identify hyperfunctional parathyroid tissue in patients with negative ultrasound findings but may show poor sensitivity and specificity in dogs.11
Abdominal ultrasonography may reveal urinary tract calculi or other lesions causing hypercalcemia (eg, lymphoma).
Plain radiography may reveal radiopaque urinary calculi or intrathoracic lesions causing hypercalcemia (eg, anterior mediastinal mass).
Other Diagnostics
Plasma PTH concentration
Values that are increased or in the upper half of reference range are consistent with PHPT in hypercalcemic patients, which should have low PTH values.
Serum PTH-related peptide concentration
Identifies most cases of hypercalcemia of malignancy
TREATMENT
Definitive treatment requires removal or ablation of parathyroid mass(es).
Medical
No definitive medical cure
Medical therapy can ameliorate severe hypercalcemia signs before definitive treatment or can be used to treat or prevent postoperative hypocalcemia following parathyroid nodule removal or ablation (see Hypercalcemia: Treatment Basics and Prevention & Treatment of Hypocalcemia below).
Surgical & Interventional
Three definitive treatments are described:
Surgical parathyroidectomy
Mass(es) should be located preoperatively using imaging.
Success rate, 89%–96%6,12
Percutaneous ultrasound-guided radiofrequency heat ablation
Nodule is destroyed by thermal necrosis from radiofrequency waves applied through IV catheter under ultrasound guidance.
Equipment is expensive.
Success rate, 81%–92%12,13
Percutaneous ultrasound-guided ethanol ablation
Ethanol is injected into the nodule with ultrasound guidance, causing coagulation necrosis.
Used less frequently because of lower success rates (~72%)12
Parathyroidectomy is most commonly used by the authors, but preferred treatment method depends on local expertise and experience.
FOLLOW-UP
Patient Monitoring
Patients should be hospitalized with limited exercise for ≥5 days postoperatively to minimize risk and monitor for hypocalcemia.
Total and ionized serum calcium concentrations should be measured q12–24h for ≥5 days postoperatively.
Slightly low serum calcium concentration (8–10 mg/dL) should be maintained to prevent iatrogenic hypercalcemia and promote return of parathyroid function.4
If given, vitamin D and calcium therapy should be tapered and discontinued over 3–5 months, starting 14 days after treatment is initiated.
Serum calcium should be measured before each reduction.
Complications4,7
Postoperative hypocalcemia can occur 4–7 days posttreatment in up to 30% of patients.
May develop after any treatment method
Causes signs in up to 10% of patients
Hypocalcemia risk may correlate with duration and magnitude of preoperative hypercalcemia, but currently there is no method for identifying which patients will be affected.14
Horner syndrome and transient laryngeal paralysis have been reported following ultrasound-guided treatment.
IN GENERAL
Relative Cost
Definitive treatment can be expensive, especially if patient requires cystotomy or has clinical hypocalcemia after treatment: $$$$$
Surgical parathyroidectomy: $$$$$
Percutaneous ultrasound-guided radiofrequency heat ablation: $$$$
Percutaneous ultrasound-guided ethanol ablation: $$$$
Prognosis
Excellent with appropriate management
Definitive treatment is curative in most cases.
Approximately 10% of patients have recurrence.4
Hypercalcemia: Treatment BasicsThe following can be used to treat patients with PHPT and preoperative clinical hypercalcemia2:
Prevention & Treatment of Hypocalcemia4
PHPT = primary hyperparathyroidism, PTH = parathyroid hormone
RUTH GOSTELOW, BVetMed (Hons), DACVIM, MRCVS, is interested in small animal endocrine diseases. Dr. Gostelow graduated from University of London, where she completed a small animal rotating internship. After two years in small animal practice, she returned to University of London to complete a residency in small animal internal medicine to pursue a PhD with a focus in feline diabetic remission.