Lymphoma in Dogs: Diagnosis & Treatment
Definitions
Lymphoma can be defined as a clonal proliferation of malignant lymphoid cells that primarily affects lymph nodes, bone marrow, or solid visceral organs, such as the liver or spleen.
Approximately 80% of cases involve peripheral lymph nodes.
Alternatively, extranodal sites can involve virtually any system, including the gastrointestinal tract, central nervous system, eyes, skin, bone, or heart.
Approximately 75% of cases involve the B-cell immunophenotype, with T-cell and rare null cell (neither B nor T) types comprising the rest.
Familial forms exist, and several chromosomal and molecular abnormalities have been implicated in the development of lymphoma.
The incidence appears to be increasing in the overall population at risk.
The most current annual incidence rate estimate is 24 per 100,000.
Lymphoma represents 15% to 20% of all malignancies and 80% of all hematopoietic malignancies in the dog.
Signalment
All breeds, ages, and sexes are at risk. Golden retrievers, boxers, bullmastiffs, basset hounds, Saint Bernards, Scottish terriers, Airedales, and bulldogs are at increased risk.
Most dogs are middle age to older at time of diagnosis, although cases have been reported in puppies as young as 1 month.
No significant sex predilection has been identified.
Causes & Risk Factors
Several genetic and molecular factors have been implicated, although none have yet been relevant to diagnostic or therapeutic approaches.
Environmental factors, which have been weakly associated with an increased risk of lymphoma, include phenoxyacetic acid herbicides (eg, 2,4-D), residency in industrial areas, exposure to chemicals (eg, paints and solvents), and exposure to strong magnetic fields.
Individuals with impaired immune function, such as immunosuppressive therapy for organ transplant or immune-mediated disorders and a past history of immune-mediated hematologic disease, are at modestly increased risk.
Pathophysiology
Most clinical and metabolic effects associated with lymphoma result from the presence and extent (clinical stage) of infiltrating tumor cells, either within the lymphoid system or in extranodal sites.
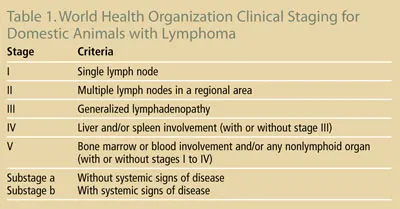
The World Health Organization clinical staging system is presented in Table 1.
Other clinical and metabolic effects can result from the cooccurrence of paraneoplastic syndromes:
Hypercalcemia occurs in approximately 15% of dogs with lymphoma and 40% of those with T-cell or thymic forms
Immune-mediated cytopenias, especially thrombocytopenia, can occur.
Signs
History for most patients is brief, owing to the tumor’s propensity to develop and progress quickly—a so-called “liquid” tumor.
In most presentations, clinical signs are limited to regional or generalized lymphadenopathy (Figure 1) and, therefore, the patient is classified as substage a, meaning without overt systemic illness (although mild inappetance and weight loss may occur).

For dogs that are clinically ill (substage b), moderate to profound inappetance, weight loss, and lethargy are generally present.
If hypercalcemia of malignancy is present, polyuria and polydipsia may occur.
Other possible signs are related to anatomic location of lymphoma.
Splenic or hepatic involvement: Organomegaly
Significant oropharyngeal lymph nodes, cranial mediastinal (ie, thymic) lymphoma, pleural effusion: Dyspnea
Obstructive lymphatic occlusion: Regional lymphedema (including precaval syndrome—a pitting edema of the face and forelimbs)
Gastrointestinal involvement: Vomiting or diarrhea
Significant immune-mediated or myelophthetic anemia, neutropenia, or thrombocytopenia: Pallor, septic fever, and hemorrhage
Bone involvement: Lameness
Cutaneous involvement: Dermal or mucocutaneous masses
Ocular involvement or secondary immune-mediated process: Uveitis
Pain Index
Lymphoma is generally not painful unless there is cortical bone involvement, which may produce lameness.
In some cases, massive lymphadenopathy is associated with local nodal pain.
Diagnosis
Differential Diagnosis
Differentials for regional or generalized lymphadenopathy:
Lymphoma
Systemic infections—bacterial (eg, pyoderma), fungal (eg, blastomycosis), parasitic (eg, leishmaniasis), rickettsial (eg, Rocky Mountain spotted fever), viral
Immune-mediated disease (eg, lupus, immune-mediated hemolytic anemia)
Reactive lymphadenopathy secondary to dermal disease, including allergic skin disease, severe fleas, Demodex mites, and pyoderma
Nodal metastatic solid tumors
Differentials for other presentations are dependent on the anatomic site involved.
Definitive Diagnosis
Complete physical examination (with special attention to lymphoid organs), including rectal examination
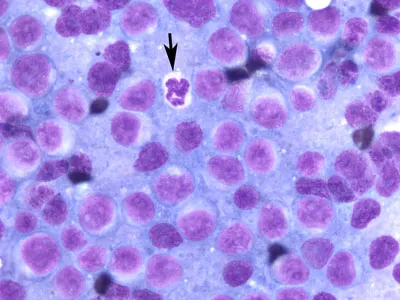
Cytology/histopathology of affected node or tissue (most cases are lymphoblastic, therefore cytology alone is diagnostic)
Monotonous population of generally large or medium-sized lymphoblasts is the norm (Figure 2)
Monotonous population of small lymphocytes is possible if small-cell variant (rare); may require histopathology or molecular diagnostics
Immunophenotyping of cytology or histopathology is recommended and available through most commercial laboratories
Complete blood count, serum biochemistry profile, urinalysis
Special attention to peripheral cytopenias implicating bone marrow involvement and/or presence of frank leukemia (circulating tumor lymphocytes)
Document hypercalcemia of malignancy if present
Assess organ function before initiating chemotherapy
Rule out underlying urinary tract infection before initiating myelosuppressive drug
Complete staging (Table 1) before treatment
Thoracic radiographs (Figure 3)
Abdominal imaging (I typically perform abdominal radiographs or ultrasound only in cases with obvious peripheral lymphadenopathy if there is an unexpected clinical sign referencing the abdomen, or if required for definitive diagnosis where infiltrative tissues are confined to the abdomen)
Molecular diagnostics (in cases where cytologic or histologic assessment is suggestive of, but not diagnostic for lymphoma)
Flow cytometric analysis at an experienced laboratory
Polymerase chain reaction for antigen receptor rearrangement (to test for tumor clonality)

Prognostic Factors
Overall, without treatment, dogs with generalized lymphoma have a median survival of approximately 4 to 6 weeks following diagnosis.
With standard chemotherapy protocols, the median survival for dogs with lymphoma is generally 1 year, with approximately 25% of dogs living 2 years or longer.
The 2 most robust negative prognostic factors currently recognized are the T-cell immunophenotype (median survival is approximately 6 months with treatment) and significant substage b disease (median survival is approximately 4 to 6 months with treatment).
Other negative, but less robust prognostic, indices include cranial mediastinal involvement, hypercalcemia, anatomic location (eg, gastrointestinal, cutaneous), current corticosteroid use, anemia, and presence of frank or bone marrow leukemia.
Low-grade or small-cell variants (rare) are associated with less chemoresponsive disease; however, long-term survival is more likely due to a smoldering course of disease.
Treatment
Generally, lymphoma in dogs is a systemic (multicentric) disease requiring systemic therapy (eg, chemotherapy). The standard of care for treating multicentric lymphoma in dogs is sequential combination chemotherapy.
Sequential Combination Chemotherapy
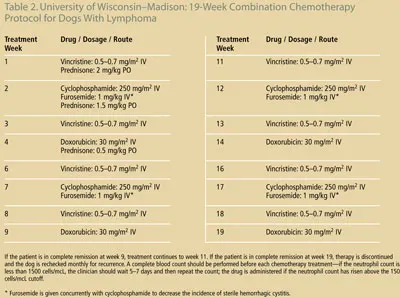
Several different protocols exist; however, all represent combinations of cyclophosphamide (C), doxorubicin (hydroxydaunorubicin [H]), vincristine (Oncovin [O]; elanco.com), and prednisone (P), also known as CHOP.
Regardless of which CHOP–based protocol is used, overall response rate is 80% to 90%, and the median remission and survival times are approximately 8 to 12 months, respectively.
Although response rates are high, cure rates are low (< 10%) and dogs will succumb to relapse of disease in a drug-resistant setting.
An example of a CHOP–based protocol that I have used with success is presented in Table 2.
Consultation with a board-certified medical oncologist is recommended because:
Combination protocols and potential treatment-associated adverse events (side effects) are complex.
New protocols and treatment alternatives may be available.
Cure rates are low and several “rescue” protocols are available when lymphoma relapses in previously treated patients.
Clinical trials of novel treatments are available nationwide that may be of interest to clients.
Alternatives to CHOP–Based Protocols
Single-agent doxorubicin is a less effective but less expensive alternative.
Single-agent oral chemotherapy (eg, cyclophosphamide or CCNU [lomustine]) may be preferred by clients who decline injectable therapy.
Single-agent prednisone therapy will often provide a short (eg, 1 month) partial or complete remission, with survival times around 2 months.
Solitary extranodal lymphoma (uncommon) can be treated as a local disease (eg, surgery or radiation therapy) if no disease is evident elsewhere; in these cases, patients can enjoy long-term survival and do not require systemic chemo-therapy initially; however, they are at risk for systemic disease in the future.
Future of Lymphoma Therapy
A major advance to therapy in humans with lymphoma is the addition of monoclonal antibody (rituximab) therapy to standard CHOP–based protocols. Unfortunately, this monoclonal does not have activity in dogs. Several investigators are currently looking for similar active monoclonal therapies in dogs.
Further advancements in the understanding of molecular targets on lymphoma cells are ongoing; as these targets are better understood, better novel therapeutics may be available.
Cost-effective bone marrow or stem cell transplant options are currently under evaluation.
In General
Relative Cost
Diagnostics can be costly depending on degree of staging that is performed.
Definitive diagnosis (cytology/histology) for generalized lymphadenopathy: $$ to $$$
Complete staging (bone marrow and imaging): $$$$
Therapy
CHOP–based chemotherapy protocol (including monitoring, drug costs, drug disposal costs): $$$$ to $$$$$
Single-agent doxorubicin chemotherapy: $$$$
Prednisone therapy: $ to $$