Lethargy in a Boxer
Genna Atiee, DVM, North Carolina State University
Karyn Harrell, DVM, DACVIM (SAIM), North Carolina State University

Prancer, a 9-year-old spayed boxer dog, was presented for lethargy and reluctance to move.
History
Approximately 2 weeks before presentation, Prancer had acute onset grade 2/4 left forelimb lameness after jumping off her owner’s bed. Several hours after the incident, she had progressively severe lethargy and was found in lateral recumbency. The owner reported the dog refused to get up or lift her head.
During the 2 weeks before current presentation, Prancer was examined by several veterinarians for decreased appetite, panting, and possible fever. Diagnostic testing was not pursued. She was intermittently febrile despite treatment with enrofloxacin at 10 mg/kg PO once a day, amoxicillin at 33 mg/kg PO twice a day, and metronidazole at 17 mg/kg PO twice a day.
Prancer had previously been healthy with no known exposure to toxins or toxicants. Regular medications included monthly heartworm and flea and tick preventives. She was up-to-date on vaccines and had access to a 2-acre fenced-in backyard.
Examination Findings
On evaluation, Prancer was quiet, alert, and responsive. BCS was 4/9. Temperature was 103.7°F; heart rate and respiratory rate were within normal limits. Mild enlargement of the popliteal lymph nodes was noted; the right was larger than the left.
Cardiac auscultation disclosed a grade I/VI left basilar systolic murmur. Pitting edema was present over the distal portions of the hindlimbs bilaterally. The left carpus was mildly effusive. Mild apparent pain was appreciated on palpation of the cranial abdomen. Probable melena was noted on rectal exam. No lameness was appreciated on walking, but Prancer was reluctant to ambulate.
Left pes with ulcerative lesion of the digital pad. The third phalanx can be seen in the deep portions of the ulcer. Image courtesy of Chie Tamamoto-Mochizuki, DVM.

Case Progress
During a 6-day observation, Prancer had intermittent fevers to 103.7°F. Sloughing of the digital pad of the fifth digit on the left pes was noted (Figure 1).
Related Article: Acute Onset of Skin Lesions in a Dog
DIAGNOSTIC TEST AND RESULTS
Isosthenuria, otherwise unremarkable USG (1.011)
| | ANA | Weakly Positive (1:40) | | Joint taps (left carpus, left hock, right hock, right carpus) | All marked suppurative inflammation with neutrophil counts ranging from 93%-98%. There were no bacteria; rare mononuclear cells were observed. | | Bartonella spp culture and PCR with BAPGM media | Negative | | Coagulation panel | Mildly elevated PTT, dimers, and fibrinogen values | | Popliteal lymph node aspirates | Moderate-to-marked lymphoid reactivity | | Urine culture and susceptibility | No growth | | Bile acids | Normal value | | Abdominal ultrasound | Mild left adrenomegaly, mild right medial iliac lymphadenopathy, cholecystic debris, urinary bladder debris | | Thoracic radiographs | Unremarkable | | Echocardiogram | All valves normal, no regurgitation noted, no evidence of endocarditis | | Spinal radiographs | Multifocal disc narrowing, no evidence of discospondylitis | | Appendicular joint survey radiographs | Normal joints | | Left pes radiographs | Left third phalangeal swelling of the fifth digit with soft tissue defect, no evidence of osseous involvement | | Liver aspirates and cytology | Moderate cholestasis | | Bile cytology | Unremarkable | | Blood culture susceptibility | No growth | | Comprehensive vector-borne panel (Babesia canis, B gibsonii, Ehrlichia canis, Rickettsia rickettsii, Anaplasma spp, Bartonella vinsonii, B henselae, B koehlerae, Mycoplasma spp, Borrelia burgdorferi, Dirofilaria immitis) | All negative | | ACTH stimulation test | 2.3, 17μg/dL (Cortisol levels pre- and post-ACTH, respectively) | | Venous blood gas | Unremarkable | | Coombs' test | Negative | | Biopsies of foot pad | Multifocal fibrinoid vascular necrosis with secondary fat necrosis; neutrophilic ulcerative dermatitis–concerning for systemic lupus erythematosus | | Bile culture and susceptibility | No growth | |
Diagnostic Results
CBC disclosed an inflammatory leukogram characterized by a moderate neutrophilia (24.217 × 103/uL; range, 2.841-9.112) with a left shift (bands, 1.361 × 103/uL); mild anemia (PCV 38%); mild decrease in plasma protein (5.7 g/dL; range, 5.9-7.3); and 5 nucleated red blood cells (nRBCS) by 50× field in oil. Serum chemistry profile showed a low-normal glucose concentration and a low BUN concentration. Hypoalbuminemia, moderately elevated ALP, mild elevation of ALT, and a mildly elevated creatine kinase were also present (Tables 1A and 1B).
CBC
*PCT represents the volume of blood on a percentage or L/L basis that comprises platelets and is a better indicator of the circulating mass of platelets, an important physiologic variable.
CHEMISTRY
URINALYSIS
Urinalysis showed isosthenuria; no other abnormalities were noted. Results of pre- and postprandial bile acid testing were within the reference ranges. Bile acid testing was performed to rule out hepatic dysfunction as the cause of hypoalbuminemia.
Abdominal ultrasonography revealed mild left adrenomegaly, mild right medial iliac lymphadenopathy, cholecystic debris, and urinary bladder debris. Thoracic radiography, echocardiography, and joint survey radiography were unremarkable. Spinal radiography showed multifocal disk narrowing with no evidence of discospondylitis.
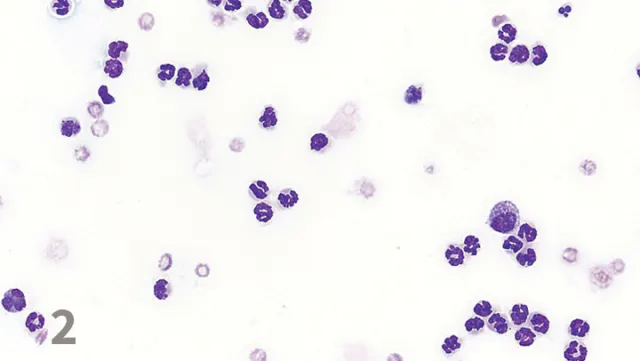
Radiography of the left pes showed swelling of the left third phalanx of the fifth digit with a soft tissue defect; no evidence of osseous involvement was noted. The left carpus was mildly effusive; no other joints were effusive on palpation. Arthrocentesis of the carpi and tarsi was performed, and cytology was suspicious for immune-mediated polyarthritis (Figure 2).
Suppurative joint fluid. Image courtesy of Jennifer Neel, DVM, DACVP.
Results of infectious disease testing for vector-borne diseases prevalent in the region were negative. Blood culture, Bartonella spp enrichment culture, and PCR and culture and susceptibility testing of the urine were negative. An aspirated specimen of the right popliteal lymph node was interpreted as reactive. ANA was present with a 1:40 titer; no reference range was provided.
Biopsy specimens of the area of the paw pad that sloughed and associated tissue were obtained. Histopathologic examination disclosed multifocal fibrinoid vascular necrosis with secondary fat necrosis and neutrophilic ulcerative dermatitis.
Related Article: Mycophenolate Mofetil
Ask Yourself
Diagnosis
Systemic Lupus Erythematosus (SLE)
Prancer was diagnosed with SLE based on the presence of 3 criteria: positive ANA titer, characteristic cutaneous lesions on histopathology, and polyarthritis.1
Although glomerular disease is common, it does not have to be present for a diagnosis of SLE. Prancer’s urine was negative for protein both with a dipstick and on measurement of albumin, so no urine protein:creatinine ratio was performed. A possible cause of Prancer’s hypoalbuminemia was vasculitis, particularly with evidence noted on her cutaneous biopsy specimen.
Another possible source of loss was through the GI tract. Prancer’s melena may have been multifactorial. Human patients with SLE are known to have mesenteric vasculitis and acute pancreatitis as sequelae to their disease.2 It is possible that vasculitis may have manifested in Prancer’s GI tract or that pancreatitis was present.
It is interesting that Prancer’s BUN was low in the face of overt GI bleeding, clinically evidenced by melena. BUN is an insensitive biomarker for GI bleeding, and in the author’s experience it can be low despite profuse melena. This could be because of poor absorption through the GI tract or decreased production by the liver.
In Prancer’s case, pre- and postprandial bile acid levels were normal, making hepatic dysfunction less likely. However, the patient did have evidence of a hepatopathy prior to the administration of steroids. This was likely secondary to SLE, but pancreatitis or cholangiohepatitis could not be ruled out.
The cause of Prancer’s isosthenuria was thought to be secondary to presumptive nephrogenic diabetes insipidus; however, it was notable that she became polyuric after initiation of steroid therapy.
Related Article: Pulmonary Thromboembolism
Treatment
Prancer was hospitalized and supportively treated for her GI bleed with omeprazole, sucralfate, maropitant, and ondansetron.
Pain management included IV fentanyl at varying rates depending on the perceived pain level. Broad-spectrum antibiotic treatment included doxycycline at 5 mg/kg PO twice a day, cefpodoxime at 10 mg/kg PO once a day, enrofloxacin at 10 mg/kg IV that was switched to PO once a day, and metronidazole at 10 mg/kg PO twice a day.
Initially, Prancer was treated for bacterial infection and possible bacteremia, and metronidazole was chosen for GI translocation and anaerobes. Her SLE could have been secondary to a drug reaction, particularly with the cephalosporins.
Prancer received immunosuppressive treatment after all cultures were returned. Initially, leflunomide (2 mg/kg PO twice per day) was chosen because polyarthritis was confirmed. A review of the veterinary literature supports the use of leflunomide with immune-mediated polyarthritis.3-4 Results of examination of the digital pad biopsy specimens1 and the presence of ANA lead to a presumptive diagnosis of SLE, and she was switched to mycophenolate because of the plethora of available human literature supporting the use of mycophenolate in patients with SLE.1-5
An anti-inflammatory dose of prednisone (1 mg/kg PO once a day) was initiated on hospital day 3, because of concerns over the GI bleed and the potential for the digital pad lesion to act as a source for infection. While larger, immunosuppressive doses of steroids are necessary for achieving remission of SLE in dogs, use of lower doses of steroids may help improve clinical signs and result in fewer side effects.
Outcome
Within 24 hours of starting prednisone, Prancer had improved dramatically. She was willing to eat, she walked outside comfortably, and the inflammatory leukogram had improved. The day before steroid administration, WBC count was 39000 cells/mm3 with 2700 bands. One day after steroid initiation, total WBC count decreased to 31000 cells/mm3 with 900 bands. She also appeared brighter and more energetic. After the biopsy specimen showed vasculitis consistent with SLE, leflunomide was switched to mycophenolate, and pentoxifylline was added for vasculitis.
Lesions and ulcers developed over several paw pads within 1 week of discharge; the lesions showed marked healing within several weeks. A slow prednisone taper was initiated after the paw pads had fully healed; results of serum studies improved and the dog continued to do well at home.
Did You Answer?
TREATMENT AT A GLANCE
2.2 mg/kg PO once a day until remission achieved, then given every 2 days
| | Cyclosporine | 5 mg/kg PO once to twice a day | | Mycophenolate mofetil | 10-20 mg/kg PO or IV twice a day | | Immunoglobulin G | 0.5-1 g/kg once a day for 1-4 days, for refractory cases or cases that present on emergency | | Levamisole | 2-5 mg/kg (150 mg max dose) every 2 days for 4 months |
ANA = antinuclear antibody, BUN = blood urea nitrogen, SLE = systemic lupus erythematosus