Handling Potential Rabies Exposure
When presented for a footpad laceration, a young adult, intact male crossbreed dog with no vaccination history bit a veterinary technician.
History
The owners had adopted the dog a month earlier when they found it wandering the neighborhood and had no success finding its owners. The dog had been brought into the house and was apparently adapting well to its new home environment. This was the first time these owners had taken the dog to a veterinarian; it had cut its foot while playing outside.
Physical Examination
At presentation, the dog appeared bright, alert, responsive, and nervous. Except for a clean laceration (1 cm) of the footpad of the right forelimb, the physical examination was unremarkable. During wound cleaning, the dog bit the veterinary technician’s hand. Although the bite appeared minor, it had broken the skin. After cleaning the bite wound, the veterinary technician expressed concern for rabies exposure, considering the patient’s lack of medical history.
Related Article: Keeping Rabies at Bay
Ask Yourself: What should be done to address the potential rabies exposure?
A. The dog should be quarantined for 6 months.
B. The dog should be immediately vaccinated for rabies, then quarantined for 10 days.
C. The dog should be quarantined, and the technician should start rabies postexposure prophylaxis (PEP) while the dog’s health status is monitored for 10 days.
D. The veterinary technician should be tested to determine the rabies titer; if protective, nothing further is required.
E. The dog should be quarantined and observed for 10 days.
F. The dog should be euthanized and tested for rabies.
Correct AnswerE. The dog should be quarantined and observed for 10 days.
Bites are common in veterinary practice, and although the incidence of human rabies in developed countries is low, the risk for rabies exposure should be considered following every mammal bite where rabies is endemic. There is often confusion in addressing potential rabies exposures; this may be compounded by variable knowledge among public health personnel and inconsistent interpretation of guidelines.
The relevant public health authority should be contacted to report the bite, the dog should be quarantined and observed (ie, caged or kenneled at an approved facility) for 10 days, and the bite victim should visit a physician.1,2 During this period, if signs suggestive of rabies develop, the dog should be euthanized and tested for rabies.
Related Article: Rabies Incidence in the US
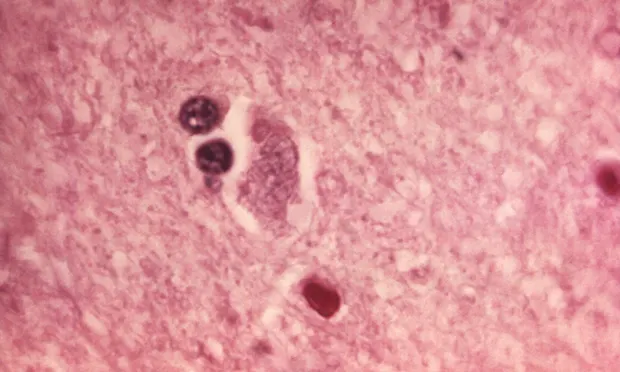
Rabies Transmission
For a dog to transmit rabies via a bite, the virus must have traveled along peripheral nerves to the brain and then to the salivary glands. Even though the incubation period for rabies can be prolonged, if an animal with rabies is capable of transmitting the virus, the disease will be advanced enough that signs will develop within 10 days of observation. If the dog appears clinically normal 10 days after the bite, it could not have been shedding the rabies virus when the bite occurred, and rabies exposure to the bite victim is not a concern.
General Protocol
A 10-day observation period is required regardless of the animal’s vaccination status.1,3 Because rabies vaccination is not completely protective, any bite victim has a potential for rabies exposure, although the risk is presumably much lower if the animal has been properly vaccinated.
If a pet is bitten by a (potentially) rabid animal, vaccination status impacts the response. A properly vaccinated dog typically receives a rabies booster vaccination and undergoes a 45-day observation at home. Dogs that are not current with rabies vaccination are typically subjected to a 6-month quarantine or euthanasia.
During observation, elective euthanasia should not be performed. If euthanasia is required for medical or welfare reasons, the body or head must be submitted to an approved testing laboratory to test brain tissue for rabies. Vaccination during the observation period is discouraged1 to prevent confusion between vaccine-related adverse effects and early rabies signs.
Postexposure Measures
PEP in humans is a highly effective preventive measure but is typically delayed during the 10-day observation period unless there has been potential massive saliva exposure (eg, severe bite) or a head or neck bite (requiring less distance for the virus to reach the brain). Rabies exposure is a medical urgency, not emergency, as there is usually sufficient time to obtain the required information rather than promptly starting PEP.
Rabies titers of blood obtained from a bitten human are of limited value and will not affect outcome. If the dog was rabid, the proper postexposure series would be indicated, regardless of the titer. The advantage of titer testing is to determine whether a human needs a booster vaccination unrelated to the potential rabies exposure.
Rabies: A Global Perspective
Rabies is present in mammals almost worldwide and is a major human health problem in some regions.
An estimated 50,000+ humans die from rabies each year.2
Most human cases occur in rural regions of developing countries and are from dog bites.
Children account for ~50% of human deaths from canine rabies virus.2
The Take-Home
Anytime a mammal bites a human in a rabies-endemic area, rabies exposure must be investigated.
Veterinary personnel must understand the principles of postbite investigation and intervention to properly address potential rabies exposures, ensure protection of owners and staff, and ensure that inappropriate responses (eg, unwarranted euthanasia) do not occur.
The approach to bites is straightforward, and helpful resources are available to guide veterinary and public health personnel. Because rabies is an urgent but not emergent issue, it is important to judiciously gather the required information to ensure an appropriate response.
PEP = postexposure prophylaxis
This article is part of the Global Edition of Clinician's Brief and part of the One Health Initiative.
J. SCOTT WEESE, DVM, DVSc, DACVIM, is veterinary internist and microbiologist, is chief of infection control at University of Guelph Ontario Veterinary College Health Sciences Centre, and holds a Canada research chair in zoonotic diseases. Dr. Weese’s research foci are infectious and zoonotic diseases (particularly of companion animals), infection control, staphylococcal infections, Clostridium difficile infection, and antimicrobial therapy.